Introduction to Rhabdomyosarcoma
Rhabdomyosarcoma (RMS) is a type of cancer that arises from rhabdomyoblasts, which are immature muscle cells that have the potential to develop into skeletal muscle. It is one of the most common soft tissue cancers found in children and adolescents, though it can also affect adults, albeit at a much lower frequency. RMS accounts for approximately 3-5% of all cancers in children and can occur in almost any part of the body, with the most common sites being the head and neck, genitourinary system, and extremities.
This form of cancer is classified into different subtypes based on the histological features, with the main ones being embryonal, alveolar, pleomorphic, and spindle cell. Embryonal RMS is the most common form in children, while alveolar RMS tends to be more aggressive and is often found in adolescents and young adults. RMS is typically highly malignant, meaning it can grow rapidly and metastasize to other areas of the body, including the lungs, bones, and lymph nodes.
Early detection and treatment are crucial for improving the prognosis of individuals diagnosed with RMS. Fortunately, with advances in medical science, the survival rate for low-risk patients has improved significantly. However, high-risk cases, such as those with metastasis or alveolar RMS, still present a challenge for oncologists.
Causes and Risk Factors of Rhabdomyosarcoma
The exact cause of rhabdomyosarcoma remains unclear, but research has identified several genetic and environmental factors that may increase the risk of developing this cancer. While most cases occur without any known family history, certain genetic mutations and environmental exposures can predispose individuals to RMS.
Genetic Factors:
-
Inherited Genetic Syndromes: Several genetic syndromes are associated with an increased risk of developing RMS. These include Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, Costello syndrome, Neurofibromatosis type 1, and Noonan syndrome. In these conditions, there is an inherent genetic predisposition to various types of cancers, including RMS.
-
Chromosomal Abnormalities: Certain chromosomal translocations and mutations, particularly PAX3-FOXO1 or PAX7-FOXO1 fusions, are strongly associated with the alveolar subtype of RMS. These genetic mutations cause abnormal cell growth and survival, leading to the development of tumours. Understanding the genetic basis of RMS helps in both diagnosis and treatment.
Environmental and Lifestyle Factors:
-
Prenatal and Early Childhood Exposure: There is some evidence that exposure to certain environmental factors during pregnancy or early childhood may increase the risk of RMS. This includes maternal exposure to ionizing radiation or other toxic chemicals. However, these links remain under study and are not fully understood.
-
Age and Gender: RMS primarily affects children under the age of 10, with a peak incidence between 2 and 6 years of age. However, it can also occur in adolescents and, rarely, in adults. The incidence is slightly higher in males than in females, particularly in the genitourinary and extremity regions.
Other Risk Factors:
-
Family History: A family history of cancer, particularly
in families with inherited cancer syndromes, can increase the risk of
developing RMS.
-
Previous Cancer Treatments: Children who have previously
been treated with chemotherapy or radiation
therapy for other cancers may have an increased risk of
developing secondary malignancies, including RMS.
Family History: A family history of cancer, particularly in families with inherited cancer syndromes, can increase the risk of developing RMS.
Previous Cancer Treatments: Children who have previously been treated with chemotherapy or radiation therapy for other cancers may have an increased risk of developing secondary malignancies, including RMS.
Although the majority of RMS cases are not directly caused by these factors, understanding these risk factors helps in early detection, especially in high-risk populations.
Symptoms and Signs of Rhabdomyosarcoma
Rhabdomyosarcoma symptoms vary depending on the tumour location and extent of disease. Early signs are often nonspecific, which makes early diagnosis challenging. However, some common signs and symptoms can be indicative of RMS, and any unexplained lumps or symptoms should prompt a medical evaluation.
General Symptoms:
-
Lump or Swelling: A noticeable, often painless, swelling
or mass is the most common sign of RMS. The size of the mass and its
location may vary, and it can be tender or hard.
-
Pain: Pain usually occurs when the tumour is pressing
against nearby structures, nerves, or bones. Pain may be localized and
can increase with movement or physical activity.
-
Fatigue and Unexplained Weight Loss: Like many cancers,
RMS can cause general symptoms like fatigue,
fever, and unexplained weight loss as
the body reacts to the cancerous cells.
Location-Specific Symptoms:
-
Head and Neck: Tumours in the head and neck can cause
nasal congestion, nosebleeds,
difficulty swallowing, or changes in voice. When the
tumour is located near the eye socket, it can cause
bulging of the eye, or proptosis, and vision problems.
-
Genitourinary Tract: In males, RMS can affect the
scrotum and cause a painless testicular mass. In
females, tumours can be found in the vagina or
uterus, causing abnormal bleeding, vaginal masses, or
urinary retention. Tumours in the bladder or
prostate can cause issues with urination or bowel
movements.
-
Extremities and Trunk: Tumours on the arms or legs may
cause swelling, difficulty moving the affected limb, and in some cases,
visible or palpable lumps. Tumours in the trunk can affect nearby organs
such as the lungs, intestines, or liver, causing pain, nausea, or other
digestive issues.
Signs of Metastasis:
-
Breathing Difficulty: If the cancer spreads to the
lungs, a person may experience difficulty breathing, coughing, or chest
pain. This can be a sign of lung metastasis.
-
Bone Pain: RMS can metastasize to the bones, causing
pain or fractures due to bone
involvement.
-
Lymphadenopathy: Enlargement of the lymph nodes may
occur if RMS has spread to these structures.
Lump or Swelling: A noticeable, often painless, swelling or mass is the most common sign of RMS. The size of the mass and its location may vary, and it can be tender or hard.
Pain: Pain usually occurs when the tumour is pressing against nearby structures, nerves, or bones. Pain may be localized and can increase with movement or physical activity.
Fatigue and Unexplained Weight Loss: Like many cancers, RMS can cause general symptoms like fatigue, fever, and unexplained weight loss as the body reacts to the cancerous cells.
-
Head and Neck: Tumours in the head and neck can cause nasal congestion, nosebleeds, difficulty swallowing, or changes in voice. When the tumour is located near the eye socket, it can cause bulging of the eye, or proptosis, and vision problems.
-
Genitourinary Tract: In males, RMS can affect the scrotum and cause a painless testicular mass. In females, tumours can be found in the vagina or uterus, causing abnormal bleeding, vaginal masses, or urinary retention. Tumours in the bladder or prostate can cause issues with urination or bowel movements.
-
Extremities and Trunk: Tumours on the arms or legs may cause swelling, difficulty moving the affected limb, and in some cases, visible or palpable lumps. Tumours in the trunk can affect nearby organs such as the lungs, intestines, or liver, causing pain, nausea, or other digestive issues.
Signs of Metastasis:
-
Breathing Difficulty: If the cancer spreads to the
lungs, a person may experience difficulty breathing, coughing, or chest
pain. This can be a sign of lung metastasis.
-
Bone Pain: RMS can metastasize to the bones, causing
pain or fractures due to bone
involvement.
-
Lymphadenopathy: Enlargement of the lymph nodes may
occur if RMS has spread to these structures.
Breathing Difficulty: If the cancer spreads to the lungs, a person may experience difficulty breathing, coughing, or chest pain. This can be a sign of lung metastasis.
Bone Pain: RMS can metastasize to the bones, causing pain or fractures due to bone involvement.
Lymphadenopathy: Enlargement of the lymph nodes may occur if RMS has spread to these structures.
Given the variety of symptoms, it is important for individuals to seek medical attention if they notice any unusual lumps, swelling, or persistent symptoms. Early detection can significantly improve treatment outcomes.
Diagnosis of Rhabdomyosarcoma
Diagnosing rhabdomyosarcoma typically involves multiple steps, including a clinical evaluation, imaging studies, and biopsy. Early diagnosis and accurate staging are essential for planning the most effective treatment.
Key Steps in Diagnosis:
-
Physical Examination: The first step in diagnosis is a
thorough physical exam, which includes checking for any lumps or unusual
masses. The location and size of the tumour will guide further
investigations.
-
Imaging Tests:
-
X-rays: To identify the location of the mass and
rule out bony involvement.
-
Ultrasound: A non-invasive test that can help
identify solid masses in soft tissues.
-
MRI or CT scans: These are the most useful
imaging techniques for soft tissue tumours.
They provide detailed information about the size, location, and
extent of the tumour.
-
PET-CT Scan: A positron emission tomography scan
combined with a CT scan can detect the spread of the cancer to
other parts of the body, helping with staging.
-
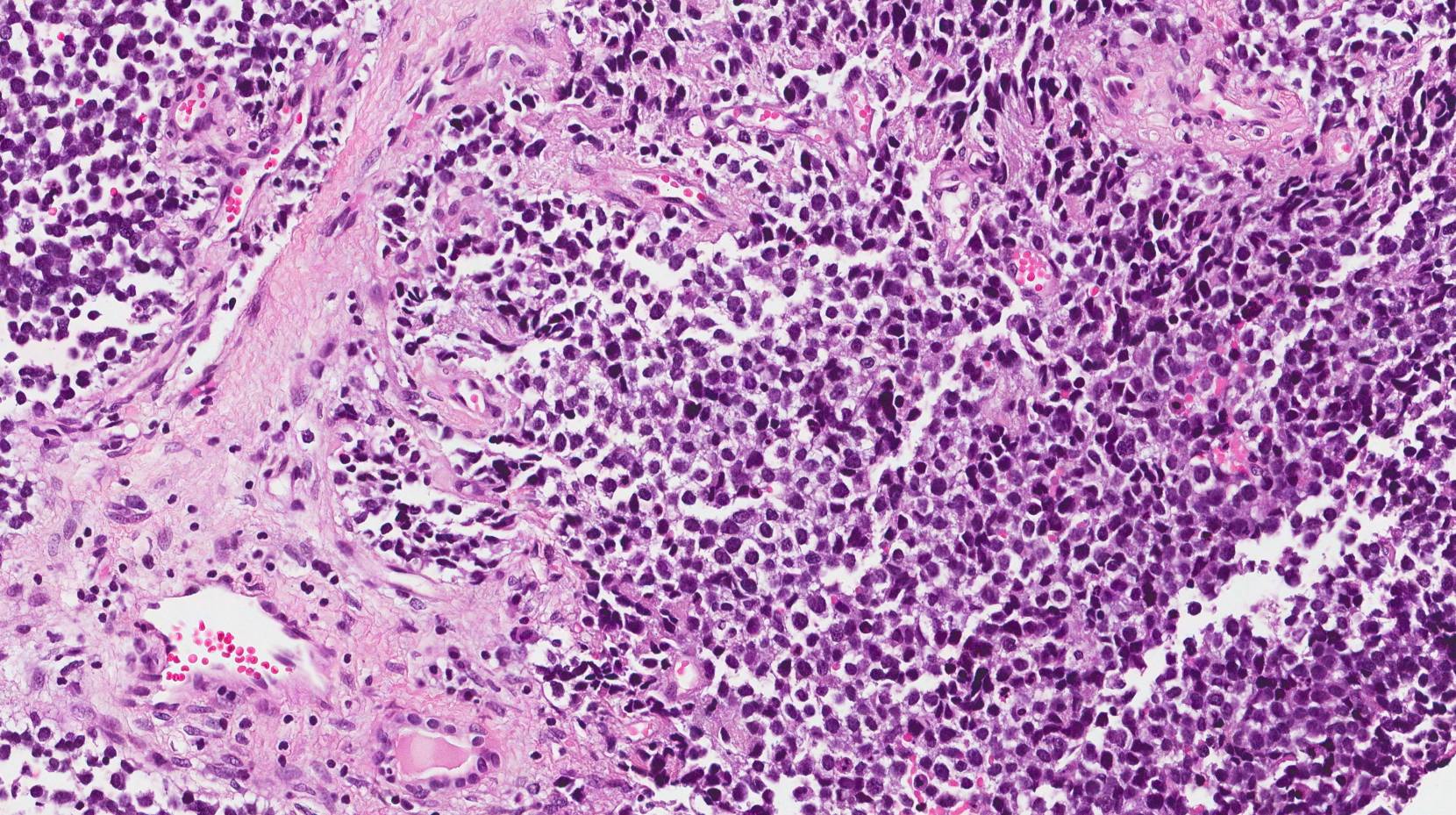
Biopsy: A definitive diagnosis of RMS is made by
removing a sample of the tumour tissue and examining it under a
microscope. This can be done through needle aspiration,
core biopsy, or surgical biopsy,
depending on the tumour's location.
-
Immunohistochemistry: Special staining techniques are
used to identify rhabdomyoblasts (cells that are
characteristic of RMS) and other markers such as
Myogenin, MyoD1, and
Desmin. This helps confirm the diagnosis and
differentiate RMS from other types of soft tissue sarcomas.
-
Genetic Testing: In some cases, molecular analysis of
the tumour may be performed to identify specific genetic mutations or
translocations, such as PAX3-FOXO1 or
PAX7-FOXO1, which are commonly associated with the
alveolar subtype of RMS.
Staging:
Physical Examination: The first step in diagnosis is a thorough physical exam, which includes checking for any lumps or unusual masses. The location and size of the tumour will guide further investigations.
Imaging Tests:
-
X-rays: To identify the location of the mass and rule out bony involvement.
-
Ultrasound: A non-invasive test that can help identify solid masses in soft tissues.
-
MRI or CT scans: These are the most useful imaging techniques for soft tissue tumours. They provide detailed information about the size, location, and extent of the tumour.
-
PET-CT Scan: A positron emission tomography scan combined with a CT scan can detect the spread of the cancer to other parts of the body, helping with staging.
Biopsy: A definitive diagnosis of RMS is made by removing a sample of the tumour tissue and examining it under a microscope. This can be done through needle aspiration, core biopsy, or surgical biopsy, depending on the tumour's location.
Immunohistochemistry: Special staining techniques are used to identify rhabdomyoblasts (cells that are characteristic of RMS) and other markers such as Myogenin, MyoD1, and Desmin. This helps confirm the diagnosis and differentiate RMS from other types of soft tissue sarcomas.
Genetic Testing: In some cases, molecular analysis of the tumour may be performed to identify specific genetic mutations or translocations, such as PAX3-FOXO1 or PAX7-FOXO1, which are commonly associated with the alveolar subtype of RMS.
Once the diagnosis is confirmed, the next step is staging the disease to determine its extent and whether it has spread to other parts of the body. The staging process helps guide treatment options and provides important information about prognosis.
Treatment Options of Rhabdomyosarcoma
The treatment of RMS is multimodal, meaning that it involves a combination of surgery, chemotherapy, and radiation therapy. The exact approach depends on the tumour's location, size, histology, and whether the disease has spread.
Surgery:
-
Primary Tumour Removal: When feasible, the primary goal
is to remove the tumour surgically. In some cases, complete resection
may not be possible due to the location of the tumour or its size.
-
Organ-Sparing Surgery: In some cases, such as when the
tumour is located in a critical area like the eye or genital region,
surgeons will aim to remove the tumour while preserving the function of
the affected organ.
Chemotherapy:
Primary Tumour Removal: When feasible, the primary goal is to remove the tumour surgically. In some cases, complete resection may not be possible due to the location of the tumour or its size.
Organ-Sparing Surgery: In some cases, such as when the tumour is located in a critical area like the eye or genital region, surgeons will aim to remove the tumour while preserving the function of the affected organ.
Chemotherapy is often the cornerstone of RMS treatment, especially if the tumour has spread or is difficult to remove surgically. Common chemotherapy regimens for RMS include:
-
Vincristine
-
Actinomycin-D
-
Cyclophosphamide
Chemotherapy is usually given in cycles, with periods of rest in between to allow the body to recover.
Radiation Therapy:
Radiation therapy may be used to treat the primary tumour, especially if surgery was not possible or if there is residual tumour left after surgery. It is also used to treat metastasis or to prevent recurrence in high-risk patients. Modern radiation techniques like proton therapy help minimize damage to surrounding tissues, which is particularly important for children.
Treatment Options Continued - Considerations, Multimodal Approach
As RMS treatment is tailored based on the individual case, the combination of surgery, chemotherapy, and radiation varies by the following factors:
-
Tumour Size and Location: Larger tumours or those located in difficult-to-access areas may require more aggressive treatment, including higher doses of chemotherapy or radiation.
-
Risk Group: Patients are classified into low-risk and high-risk groups based on the staging and type of tumour. Low-risk patients may receive less aggressive treatment, while high-risk patients may need more intensive chemotherapy, larger radiation doses, or even stem cell transplants.
Targeted Therapies and Immunotherapy:
Research in RMS has led to the development of targeted therapies that aim to specifically attack cancer cells based on genetic or molecular markers. Trials are ongoing to investigate drugs that target the genetic mutations seen in RMS cells, as well as immunotherapy options that can boost the body's immune response to cancer.
Prevention and Management of Rhabdomyosarcoma
Since the exact causes of RMS are not fully understood, there is currently no known way to prevent the disease. However, there are strategies to manage the disease effectively and prevent recurrence:
Prevention:
-
Genetic Counseling: For individuals with a family
history of cancer or genetic syndromes, genetic counseling may help
assess the risk and provide early monitoring.
Management:
-
Follow-Up Care: Survivors of RMS require regular
follow-up visits to monitor for late effects of treatment, such as
secondary cancers, organ damage, or growth and developmental issues in
children.
-
Physical and Emotional Support: Survivors may face
long-term challenges related to physical disabilities, psychosocial
issues, and emotional well-being. Rehabilitation, counselling, and
support groups are essential in managing the impact of the disease.
Genetic Counseling: For individuals with a family history of cancer or genetic syndromes, genetic counseling may help assess the risk and provide early monitoring.
-
Follow-Up Care: Survivors of RMS require regular follow-up visits to monitor for late effects of treatment, such as secondary cancers, organ damage, or growth and developmental issues in children.
-
Physical and Emotional Support: Survivors may face long-term challenges related to physical disabilities, psychosocial issues, and emotional well-being. Rehabilitation, counselling, and support groups are essential in managing the impact of the disease.
Complications of Rhabdomyosarcoma
Like many cancers, RMS and its treatment can result in complications, which can affect the patient's quality of life both during and after treatment:
Complications of the Disease:
-
Metastasis: The most serious complication of RMS is its
potential to spread to other parts of the body, such as the
lungs, bones, and lymph
nodes. This can make treatment more complex and impact
prognosis.
-
Pain and Organ Dysfunction: Depending on where the
tumour is located, it can cause pain, organ dysfunction (e.g.,
respiratory or urinary issues), and other systemic effects.
Complications of Treatment:
-
Chemotherapy side effects: Nausea, vomiting, hair loss,
and bone marrow suppression are common. Long-term effects may include
fertility issues, heart damage, or
secondary cancers.
-
Radiation Therapy: The risk of radiation-induced
cancer, especially when radiation is given at an early age,
can be a significant long-term complication.
-
Surgical Risks: Surgery can lead to infections,
bleeding, and, in some cases, permanent organ damage or functional
impairment, depending on the tumour location.
Metastasis: The most serious complication of RMS is its potential to spread to other parts of the body, such as the lungs, bones, and lymph nodes. This can make treatment more complex and impact prognosis.
Pain and Organ Dysfunction: Depending on where the tumour is located, it can cause pain, organ dysfunction (e.g., respiratory or urinary issues), and other systemic effects.
-
Chemotherapy side effects: Nausea, vomiting, hair loss, and bone marrow suppression are common. Long-term effects may include fertility issues, heart damage, or secondary cancers.
-
Radiation Therapy: The risk of radiation-induced cancer, especially when radiation is given at an early age, can be a significant long-term complication.
-
Surgical Risks: Surgery can lead to infections, bleeding, and, in some cases, permanent organ damage or functional impairment, depending on the tumour location.
Living with the Condition of Rhabdomyosarcoma
Surviving RMS, particularly in children, requires navigating both the immediate aftermath of treatment and the long-term challenges that arise. Survivors often face physical, psychological, and social challenges that need careful management.
Physical Rehabilitation:
Patients may need physical therapy to regain strength and function, especially if surgery or radiation has caused impairment. For children, developmental support and monitoring growth are crucial components of care.
Psychosocial Support:
Psychological support, including counselling, is vital to help patients cope with the emotional toll of cancer treatment. This support is also critical for families who face the emotional strain of seeing a loved one through such a challenging journey.
Long-Term Monitoring:
Post-treatment care includes regular check-ups to monitor for relapse, manage late effects of therapy, and provide necessary interventions for secondary health issues. As patients move into adulthood, the transition from pediatric to adult care should be seamless, ensuring continued support.
Top 10 Frequently Asked Questions about Rhabdomyosarcoma
1. What is rhabdomyosarcoma (RMS)?
Rhabdomyosarcoma (RMS) is a rare and aggressive cancer that originates in the soft tissue of the body, typically in muscles that would normally develop into skeletal (voluntary) muscles. It is the most common type of soft tissue sarcoma in children, although it can also occur in adults. RMS develops when the cells in the muscles grow abnormally, forming a tumor. These tumors can occur anywhere in the body, but are most commonly found in the head and neck area, urinary and reproductive organs, limbs, and sometimes in the trunk. Because RMS is aggressive and can spread quickly, early diagnosis and prompt treatment are crucial to improving the prognosis. The disease presents with various symptoms depending on the tumor's location, which can make diagnosis a challenge in the early stages.
2. What are the common signs and symptoms of rhabdomyosarcoma?
The symptoms of rhabdomyosarcoma vary depending on the location of the tumor. Common signs include a noticeable lump or swelling in the affected area, which may be painless or tender to the touch. In cases where the tumor is located in the head and neck region, symptoms might include difficulty swallowing, changes in facial appearance, or vision problems. If the tumor is located near the urinary tract or reproductive organs, it could cause urinary problems, bleeding, or pain in the pelvic region. Nasal congestion and difficulty breathing are also reported if the tumor is near the nasal passages. In the limbs or trunk, pain, restricted movement, or the growth of a palpable mass are common. In some cases, children with RMS may also experience unexplained weight loss and fatigue. Early detection of these symptoms is crucial for prompt diagnosis and treatment.
3. What causes rhabdomyosarcoma, and who is at risk?
The exact cause of rhabdomyosarcoma is not always clear. However, certain genetic mutations and inherited conditions increase the risk of developing this type of cancer. These include conditions such as Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, neurofibromatosis type 1, and other rare genetic disorders that can affect cell growth and tumor suppression. RMS is most common in children, with a peak incidence occurring between the ages of 2 and 6, although it can affect people of all ages. Environmental factors, family history, and lifestyle factors do not appear to play a significant role in the development of RMS. Research continues to explore potential genetic mutations and environmental triggers for the disease.
4. How is rhabdomyosarcoma diagnosed and staged?
The diagnosis of rhabdomyosarcoma typically begins with a physical examination and an assessment of the symptoms. Imaging tests, such as CT scans, MRI, and PET scans, are used to determine the size, location, and spread (metastasis) of the tumor. If RMS is suspected, a biopsy is performed to confirm the diagnosis. During a biopsy, a sample of the tumor tissue is removed and examined under a microscope to determine if the cells are cancerous and identify the specific type of RMS. Once diagnosed, the tumor is staged to assess how far it has spread. Staging involves determining whether the tumor is localized or has spread to nearby tissues or lymph nodes (regional spread), or to other parts of the body (distant metastasis). This helps guide the treatment plan and predict the prognosis.
5. What are the treatment options for rhabdomyosarcoma?
The treatment of rhabdomyosarcoma typically involves a combination of surgery, chemotherapy, and radiation therapy. The goal of surgery is to remove as much of the tumor as possible, especially if it is located in an area where it can be safely excised. However, complete removal is not always possible due to the tumor's proximity to vital structures. Chemotherapy is used to treat any cancer cells that might have spread beyond the primary tumor site, and it is often given before or after surgery to shrink the tumor or reduce the risk of recurrence. Radiation therapy is also commonly used, particularly for tumors that cannot be surgically removed or for residual disease after surgery. The treatment regimen is tailored to the individual based on the location, size, and stage of the tumor, as well as the patient's overall health. In some cases, clinical trials exploring newer therapies may be recommended.
6. What is the prognosis for someone with rhabdomyosarcoma?
The prognosis for someone with rhabdomyosarcoma depends on several factors, including the type of RMS, the tumor's location, how early the disease is detected, and whether it has spread to other areas. In general, younger patients tend to have better outcomes, particularly if the disease is localized and can be surgically removed. The embryonal subtype of RMS has a better prognosis compared to the alveolar subtype, which is more aggressive. The success rate of treatment also varies based on whether the tumor is in a favorable location (such as the limbs) or a more challenging area (such as the head or pelvis). Overall, the 5-year survival rate for children with localized RMS is around 70%, but this can decrease significantly if the cancer has spread. With advances in treatment, survival rates have improved, but outcomes are highly individualized.
7. What are the potential long-term effects or complications of treatment?
The treatment of rhabdomyosarcoma can lead to several long-term effects, depending on the type and location of the treatment received. Chemotherapy can weaken the immune system, increase the risk of infections, and cause fertility issues, especially if the ovaries or testes are exposed to radiation or chemotherapy. Radiation therapy may cause long-term problems, including growth issues in children, secondary cancers, and damage to surrounding tissues and organs. In some cases, the treatment can lead to cardiovascular problems or damage to the kidneys or lungs. Patients who have had surgery may also face scarring or the loss of function in the affected area. Therefore, regular follow-up care is critical to monitor for late side effects and manage long-term health.
8. Can rhabdomyosarcoma be prevented?
There is no known way to prevent rhabdomyosarcoma because the exact causes are not fully understood. Since it often occurs due to genetic mutations, there are no known lifestyle changes or environmental factors that can significantly reduce the risk of developing this cancer. However, for individuals with genetic syndromes that increase the risk of RMS, regular screenings and early detection through medical surveillance may help identify the disease at an early stage, when treatment is most effective. Genetic counseling may also be recommended for families with a history of inherited conditions that predispose them to RMS.
9. How can I support someone with rhabdomyosarcoma during treatment?
Supporting someone with rhabdomyosarcoma involves being there emotionally and physically during their treatment journey. This can include helping with day-to-day tasks, offering emotional support during chemotherapy or radiation therapy, and providing transportation to and from medical appointments. Encouragement to maintain a positive attitude and staying involved with treatment decisions can also be important. It's crucial to help the patient manage the side effects of treatment, including fatigue, nausea, and pain. Emotional support is especially important, as cancer treatment can be mentally and emotionally taxing, and staying positive can contribute to a better quality of life.
10. What is the role of clinical trials in rhabdomyosarcoma treatment?
Clinical trials play a critical role in advancing the treatment options for rhabdomyosarcoma, especially since the disease is rare and often difficult to treat. Trials may offer access to new treatments, drug combinations, or innovative therapies that are not yet widely available but could potentially improve outcomes. Participating in a clinical trial allows patients to contribute to medical research and potentially benefit from cutting-edge treatment options. However, clinical trials are not without risks, and patients should discuss the potential benefits and drawbacks with their healthcare provider before making a decision.


