Introduction to Ross Procedure
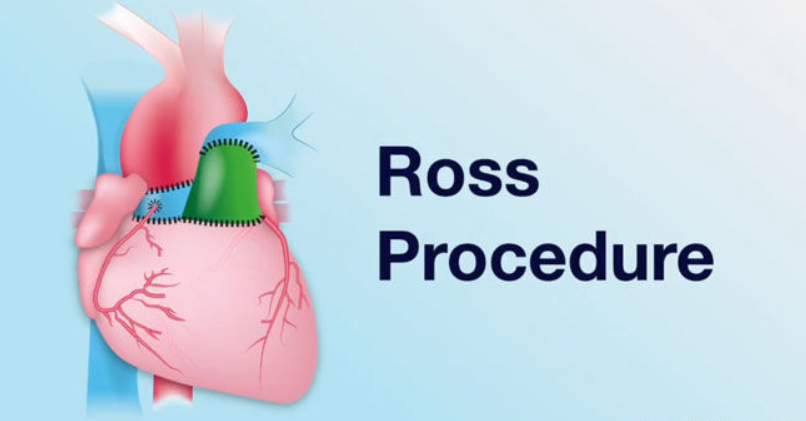
The Ross Procedure is a specialized and sophisticated cardiac surgical operation designed to treat patients with significant aortic-valve disease (such as severe aortic stenosis or aortic regurgitation), especially in children and younger adults. In this procedure, the patient's own healthy pulmonary valve—including the root of the pulmonary valve—is excised and transplanted into the aortic position (known as the autograft). Then a donor pulmonary valve (a homograft) is placed into the right-ventricular outflow tract (pulmonary position). In effect, the diseased aortic valve is replaced with the patient's own living tissue, and their pulmonary valve is replaced with a donor valve. This “double-valve” transformation allows the aortic position to benefit from a living valve rather than a mechanical or conventional bioprosthetic substitute.
Proponents of the Ross Procedure point to its excellent hemodynamic performance (because the autograft behaves very much like a natural aortic valve), the avoidance of lifelong anticoagulation (which is typically required if a mechanical valve is used), and the capacity for growth (important in pediatric patients). The historical origins date back to the work of Donald Ross in the 1960s, and over the decades, many refinements in technique, patient selection and postoperative management have improved outcomes significantly. Recent long-term follow-up data show survival into the third decade that is comparable to the general population in select expert centres, although the procedure remains technically demanding and best done at high-volume centres with experience.
Causes and Risk Factors of the Ross Procedure
The Ross Procedure is typically indicated for patients with severe aortic valve disease, particularly when they are young and need a long-lasting, functional solution. Below are the primary conditions and risk factors that might lead a patient to opt for the Ross Procedure:
Causes of Aortic Valve Disease Leading to Ross Procedure:
-
Aortic Valve Stenosis: This is a condition in which the aortic valve narrows, restricting blood flow from the heart to the rest of the body. Over time, this can cause left ventricular hypertrophy, heart failure, and poor exercise tolerance.
-
Aortic Valve Regurgitation: In this condition, the aortic valve does not close properly, allowing blood to flow backward into the left ventricle. This increases the workload on the heart and can lead to heart failure.
-
Congenital Heart Conditions: Many patients, especially younger ones, may have bicuspid aortic valves (a congenital defect where the valve has two leaflets instead of three), which predisposes them to early aortic valve failure.
-
Aortic Valve Endocarditis: Infections of the aortic valve can damage the valve tissue and impair function, necessitating surgical replacement.
-
Aortic Root Dilation: In patients with connective tissue disorders (such as Marfan syndrome), the aortic root may dilate, leading to aortic valve insufficiency and the need for valve replacement.
Risk Factors for the Ross Procedure:
While the Ross Procedure is an excellent option for younger patients with aortic valve disease, it is not suitable for everyone. Several factors may influence whether a patient is a good candidate for the procedure:
-
Age: The Ross Procedure is most commonly performed on younger individuals, particularly those under 50 years of age. This is because the autograft (pulmonary valve) can grow with the patient, making it an ideal choice for younger people.
-
Pulmonary Valve Health: Since the pulmonary valve is used as the replacement in the aortic position, it is essential that the pulmonary valve is healthy and suitable for transplant. Patients with pulmonary valve disease or dysfunction may not be candidates for this procedure.
-
Aortic Root Size: The aortic root size and the anatomy of the aortic valve are crucial for the success of the Ross Procedure. If the aortic root is too large or too small, it may affect the implantation of the pulmonary valve.
-
Comorbid Conditions: Patients with significant coronary artery disease or other cardiovascular conditions may need a different treatment approach. The Ross Procedure requires careful evaluation of the heart's overall function.
-
Connective Tissue Disorders: Certain connective tissue disorders, such as Marfan syndrome, can present complications in performing the Ross Procedure, though it remains a viable option for some patients with these conditions.
Symptoms and Signs of Ross Procedure Candidacy
The Ross Procedure is generally considered for patients who exhibit signs and symptoms of severe aortic valve dysfunction. These symptoms can include:
-
Chest Pain or Angina: Due to restricted blood flow from a narrowed or leaking aortic valve, patients may experience chest pain or discomfort, particularly during physical exertion.
-
Shortness of Breath (Dyspnea): Reduced cardiac output due to an aortic valve issue can result in fluid buildup in the lungs, leading to difficulty breathing, especially during exertion.
-
Fatigue and Weakness: As aortic stenosis or regurgitation worsens, the heart becomes less efficient at pumping blood, leading to feelings of tiredness and general weakness.
-
Swelling (Edema): Fluid buildup in the legs, abdomen, or lungs can cause swelling, especially in advanced cases of aortic valve disease.
-
Syncope (Fainting): Some patients may experience fainting episodes due to reduced blood flow to the brain caused by aortic valve dysfunction.
-
Murmurs: A heart murmur (an abnormal sound) is often heard during a physical exam, particularly in patients with aortic valve issues. A systolic murmur may be heard in cases of aortic stenosis, while a diastolic murmur may indicate aortic regurgitation.
-
In Children: In pediatric patients, failure to thrive, poor weight gain, or difficulty with exercise or physical activity can suggest the need for a surgical intervention like the Ross Procedure.
If these symptoms are present, patients may be referred for diagnostic testing to assess the severity of their aortic valve condition.
Diagnosis of Ross Procedure Candidacy
Diagnosing the need for the Ross Procedure involves a combination of clinical evaluation and advanced imaging techniques to assess the aortic valve and its functionality. The main diagnostic steps include:
-
Physical Examination: A thorough physical exam can reveal characteristic signs of aortic valve disease, such as heart murmurs, edema, and signs of heart failure.
-
Echocardiography: This is the primary diagnostic tool used to evaluate the structure and function of the aortic valve. Transthoracic and transesophageal echocardiography can provide detailed images of the aortic valve and root, as well as assess the severity of stenosis or regurgitation.
-
Cardiac MRI/CT: These imaging techniques provide more detailed views of the heart and its anatomy, particularly the aortic root, and help surgeons assess whether the Ross Procedure is feasible.
-
Cardiac Catheterization: In some cases, a catheter is inserted into the heart to directly measure pressures within the heart chambers and evaluate the severity of aortic valve dysfunction.
-
Genetic Testing: For patients with suspected connective tissue disorders (such as Marfan syndrome), genetic testing may be performed to assess the risk of complications associated with the Ross Procedure.
Once the severity of the aortic valve disease is assessed and the patient's overall heart health is evaluated, the surgical team can determine if the Ross Procedure is the most suitable option.
Treatment Options of Ross Procedure
The Ross Procedure involves two main steps: replacing the diseased aortic valve with the patient's own pulmonary valve (autograft), and replacing the pulmonary valve with a donor valve (homograft). The procedure is performed under general anesthesia and requires a median sternotomy, where the breastbone is divided to access the heart.
Steps Involved in the Ross Procedure:
-
Preparation: The patient is placed under general anesthesia, and a heart-lung machine is used to take over the function of the heart and lungs while the surgery is performed.
-
Removal of the Pulmonary Valve: The healthy pulmonary valve, along with its root, is carefully excised from the right ventricle.
-
Aortic Valve Replacement: The pulmonary autograft is then implanted into the aortic position, and the coronary arteries are reattached to the autograft.
-
Pulmonary Valve Replacement: A donor pulmonary homograft is then placed in the pulmonary position to replace the removed pulmonary valve.
-
Closure and Recovery: After the procedure, the heart-lung machine is disconnected, and the heart is restarted. The chest is then closed, and the patient is monitored in the intensive care unit (ICU) before being moved to a recovery room.
Advantages of the Ross Procedure:
-
Avoidance of Lifelong Anticoagulation: Since the autograft is made from the patient's own tissue, the need for lifelong anticoagulation is eliminated, unlike mechanical valve replacements.
-
Better Hemodynamics: The autograft valve behaves more like a natural aortic valve, providing superior hemodynamics compared to mechanical or bioprosthetic valves.
-
Growth Potential: In pediatric patients, the pulmonary autograft can grow with the patient, reducing the need for future surgeries.
-
Fewer Long-Term Complications: Compared to mechanical or bioprosthetic valves, the Ross Procedure carries fewer risks of valve degeneration or thromboembolism.
Alternative Treatment Options:
For patients who are not candidates for the Ross Procedure, other options include:
-
Mechanical Aortic Valve Replacement: Suitable for older patients but requires lifelong anticoagulation.
-
Bioprosthetic Valve Replacement: Suitable for older patients or those unable to tolerate anticoagulation but may need to be replaced after 10-15 years.
-
Aortic Valve Repair: For select patients with aortic valve disease who do not require complete replacement.
Prevention and Management of Ross Procedure
While the Ross Procedure itself is designed to treat severe aortic valve disease, there are important aspects of prevention and ongoing management to ensure the long-term success of the procedure:
Preoperative Management:
-
Preoperative Assessment: Comprehensive testing (echocardiography, MRI, genetic screening) should be performed to ensure that the pulmonary valve is healthy enough to be transplanted.
-
Medication Optimization: Medications to control blood pressure, heart rate, and any underlying conditions should be optimized before surgery to ensure the best outcomes.
-
Psychosocial Support: Counseling for patients, especially younger ones, is essential to prepare them for surgery and to manage expectations regarding recovery and lifestyle changes.
Postoperative Management:
-
Blood Pressure Control: Strict blood pressure management is essential to reduce stress on the autograft, which is placed in the high-pressure aortic position.
-
Anticoagulation: Although anticoagulation is not required for the Ross autograft, some patients may require antiplatelet therapy for the homograft or due to the surgical procedure itself.
-
Regular Follow-ups: Routine echocardiograms and imaging studies are essential to monitor the function of the autograft and homograft, checking for signs of dilation or regurgitation.
-
Physical Rehabilitation: Post-surgery rehabilitation is important to help patients return to their normal activities. This is particularly important for younger patients who may be highly active.
Complications of Ross Procedure
Although the Ross Procedure is generally considered to have excellent outcomes, it is not without potential complications. These include:
-
Autograft Dilation and Aortic Regurgitation: Over time, the pulmonary autograft may dilate, leading to aortic regurgitation, especially if the aortic root was initially dilated.
-
Homograft Failure: The donor pulmonary valve may fail over time, leading to stenosis or regurgitation in the pulmonary position, which may require a future replacement.
-
Infection: As with any major surgery, there is a risk of infection at the surgical site or in the heart valve tissue.
-
Bleeding and Arrhythmias: Surgery on the heart carries the risk of bleeding, as well as the development of arrhythmias postoperatively, which may require intervention.
-
Thrombosis and Embolism: Although the Ross Procedure eliminates the need for lifelong anticoagulation, some patients may still require anticoagulation or antiplatelet therapy, increasing the risk of clotting issues.
Living with the Condition of Ross Procedure
After undergoing the Ross Procedure, patients can expect to live a relatively normal and active life, particularly if they are younger. However, there are several factors to consider in the long term:
-
Follow-Up Care: Ongoing monitoring is crucial to check for autograft dilatation, homograft failure, or other complications. Regular echocardiograms and imaging are necessary for detecting problems early.
-
Physical Activity: Many patients, especially younger ones, return to an active lifestyle post-surgery. However, high-contact sports or activities that could put excessive strain on the heart should be avoided.
-
Psychological Support: Having undergone such a major surgery, some patients may experience anxiety about their future health. Regular psychological support and counseling can help patients cope with any emotional or psychological challenges.
-
Diet and Lifestyle: A heart-healthy diet and lifestyle, including weight management, regular exercise, and avoiding smoking, are important for ensuring long-term heart health and the longevity of the valve replacements.
Top 10 Frequently Asked Questions about Ross Procedure
1. What exactly is the Ross Procedure?
The Ross Procedure is a type of heart valve surgery used to treat severe disease of the aortic valve. In this operation, the surgeon removes the diseased aortic valve and replaces it with the patient's own healthy pulmonary valve (known as the autograft). Then, to replace the now-vacant pulmonary valve slot, a donor (homograft) pulmonary valve is implanted. This “swap” allows the patient's living valve tissue to take over the aortic function, while the donor valve assumes the pulmonary role.
2. Who is a candidate for the Ross Procedure?
Candidates typically include younger, otherwise healthy patients who have aortic valve disease (such as aortic stenosis or regurgitation) and have good pulmonary valve anatomy. It is often considered in children, adolescents, or young adults — especially those who wish to avoid lifelong blood-thinning medications, or who have small aortic annulus or other anatomical challenges. The decision depends on overall health, the condition of other heart structures, and surgeon expertise.
3. What are the main advantages of choosing the Ross Procedure?
Key benefits include:
-
The autograft (your own pulmonary valve) tends to work in the aortic position with very good hemodynamics (blood flow) and often better long-term performance than prosthetic valves.
-
Because it is living tissue, there is often no need for lifelong anticoagulation (blood-thinning drugs) which are required with many mechanical valves.
-
For younger patients, especially children, the autograft may grow with the body, making it especially advantageous in growing patients.
-
It may allow a more natural lifestyle (physical activity, pregnancy in women) with fewer restrictions in some cases.
-
Am I a good candidate for the Ross Procedure based on my age, anatomy, health status and lifestyle goals?
-
What is your (the surgeon's) experience with the Ross Procedure (how many have you done, what are your outcomes)?
-
What are the expected benefits for me, and what are the risks (short-term and long-term) specific to my case?
-
What is the expected recovery timeline, what restrictions will I have, and how will my lifestyle be managed afterwards?
-
What follow-up will be required, what are the chances I may need another surgery in the future, and how do you monitor for problems?
4. What are the risks and potential complications of the Ross Procedure?
Though the Ross Procedure has many advantages, it is a technically complex surgery and carries risks. Potential complications include bleeding, infection, arrhythmia (heart rhythm disturbances), dysfunction of the autograft or the donor valve, dilation of the new aortic root (autograft dilatation), or narrowing/stenosis of the pulmonary homograft. Because two valves are involved (your pulmonary valve moved and a donor placed), there is the possibility of needing a future intervention on either valve. Long-term follow-up is required.
5. How is the surgery performed and what is the recovery like?
The surgery is performed under general anesthesia, using a median sternotomy (opening the chest bone) in most cases. After removal of the diseased aortic valve, the pulmonary valve is harvested and implanted in its place, the coronary arteries are reattached, and then the donor pulmonary valve is inserted into the right heart outflow tract. Recovery includes time in an intensive care unit (ICU) post-surgery, hospital stay of several days, and several weeks of recovery at home, with restrictions on heavy lifting or vigorous activity until cleared by the surgical team.
6. How long do the results of the Ross Procedure last, and does it eliminate future valve problems?
The Ross Procedure offers excellent long-term outcomes in appropriately selected patients, and in many series the survival and quality of life approach those of age-matched healthy populations. However, because two valves are involved (the autograft and the homograft), there is a non-zero risk of progressive changes over time, such as autograft dilatation or homograft degeneration. Some patients may require further procedures in the future, so lifelong monitoring is essential.
7. What lifestyle changes or follow-up care are required after the Ross Procedure?
After the procedure, patients must attend regular cardiology follow-ups, including imaging (echocardiography, CT scans) to monitor valve function and root dimensions, as well as general cardiac health. Lifestyle changes include maintaining control of blood pressure to protect the new valve and aortic root, avoiding smoking, maintaining a healthy weight, and engaging in appropriate physical activity as approved. In some cases restrictions (temporary or longer-term) on intense physical exertion may apply depending on the individual's heart condition.
8. Are there any patients for whom the Ross Procedure is not suitable?
Yes. The Ross Procedure is not a fit for everyone. Patients with significant disease of the pulmonary valve, or certain connective tissue disorders (such as Marfan syndrome), severe coronary artery disease, or advanced multi-valve heart disease may not be suitable. Also, patients whose overall health or anatomy make such complex surgery riskier may be offered alternative valve replacement strategies instead.
9. How does the Ross Procedure compare with other types of aortic valve replacements?
Compared to mechanical or standard bioprosthetic aortic valve replacements, the Ross offers the advantages of using living tissue, avoiding lifelong anticoagulation (in many cases), and potentially better long-term hemodynamic performance. On the other hand, it is a more complex operation, involves two valve sites instead of one, and may not be available or advisable in all centers or patients. The choice between methods should involve careful discussion of benefits/risks with the heart surgery team.
10. What questions should I ask my heart surgeon if I'm considering the Ross Procedure?
Before proceeding, it's helpful to ask:


