Introduction to Rotational and Directional Atherectomy
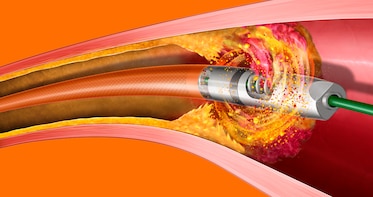
Rotational and directional atherectomy are specialized minimally invasive procedures used to treat patients with complex atherosclerotic arterial disease. These techniques are particularly helpful when dealing with calcified plaque, rigid vessel walls, or long occlusions that traditional angioplasty or balloon dilation cannot effectively treat.
Atherectomy refers to the removal or debulking of plaque from an artery. The goal of these procedures is to restore blood flow in arteries that have been narrowed by the buildup of atherosclerotic plaques, which can cause reduced oxygen supply to tissues and organs, leading to complications such as heart attacks, stroke, and limb amputation.
Rotational atherectomy involves using a high-speed rotating device, typically a diamond-coated burr, which is used to shave off the plaque and debulk calcified or fibrous lesions in the artery. The high rotational speed allows the burr to smooth the plaque while minimizing the risk of damaging the artery wall. The directional atherectomy technique, on the other hand, uses a cutting or shaving device to remove plaque in a controlled direction, usually toward the tip of the catheter. This technique is often employed for focal lesions or targeted debulking.
Both procedures are commonly used to treat coronary artery disease (CAD) and peripheral artery disease (PAD), especially when other treatment options, like balloon angioplasty or stent placement, are not sufficient to restore proper blood flow.
These procedures are an essential part of the toolbox for interventional cardiologists and vascular surgeons, particularly for patients with more complex vascular conditions that require careful plaque removal to optimize treatment outcomes. They are minimally invasive, typically performed via catheterization, and require only a small incision, which significantly reduces recovery time compared to traditional open surgeries.
Causes and Risk Factors of Rotational and Directional Atherectomy
Rotational and directional atherectomy are used to treat advanced atherosclerotic disease—a condition where atherosclerotic plaques (fatty deposits) accumulate on the walls of arteries, leading to narrowing, stiffening, and eventual blockage of the artery. The underlying causes of atherosclerosis involve a combination of genetic and environmental factors, and the risk factors that make atherectomy necessary include:
Causes of Atherosclerosis:
-
Excess Cholesterol and Fat in the Blood: High levels of low-density lipoprotein (LDL), or "bad cholesterol", can cause the buildup of plaque in the arteries. In addition, triglycerides (a type of fat in the blood) can also contribute to plaque formation.
-
High Blood Pressure (Hypertension): Chronic high blood pressure can cause damage to the blood vessel walls, making them more vulnerable to plaque accumulation. The pressure also forces the heart to work harder, which can exacerbate the effects of arterial damage.
-
Diabetes and Insulin Resistance: Diabetes increases the risk of developing atherosclerosis. High blood sugar levels can cause damage to the inner lining of arteries, making them more prone to plaque buildup. People with type 1 and type 2 diabetes are more likely to develop both CAD and PAD.
-
Smoking: Tobacco use is one of the leading contributors to atherosclerosis. Smoking accelerates the development of plaque in the arteries and raises the risk of arterial occlusion.
-
Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis, lupus, or periodontal disease, may increase the likelihood of plaque formation in the arteries.
-
Genetic Factors: Family history plays a significant role in determining a person's risk for developing atherosclerosis. Certain genetic conditions, such as familial hypercholesterolemia, predispose individuals to early plaque buildup in arteries.
-
Age and Gender: The risk of developing atherosclerosis increases with age. Men are generally at higher risk for developing coronary artery disease at an earlier age, but the risk for women increases after menopause.
Risk Factors That Lead to Atherectomy:
The need for rotational or directional atherectomy arises when standard procedures such as balloon angioplasty or stenting fail due to the presence of more complex and heavily calcified lesions. Patients most at risk of needing atherectomy include those with:
-
Severe Coronary Artery Disease (CAD), especially in the presence of calcified lesions that are difficult to treat with angioplasty alone.
-
In-Stent Restenosis, where the artery narrows again after a stent has been placed, often due to calcium buildup or neointimal hyperplasia (growth of new tissue).
-
Peripheral Artery Disease (PAD), particularly in patients with tortuous arteries, calcified plaques, or those who have undergone previous interventions like bypass surgery.
-
Chronic Total Occlusions (CTOs), where the artery is completely blocked for an extended period.
Patients who have one or more of these underlying conditions may require atherectomy to clear the plaque and restore adequate blood flow to the heart or limbs.
Symptoms and Signs of Rotational and Directional Atherectomy
The primary symptoms and signs that lead to the consideration of rotational or directional atherectomy are usually associated with atherosclerosis and its complications, particularly in coronary and peripheral arteries.
Common Symptoms in Coronary Artery Disease (CAD):
-
Chest pain (angina): A hallmark symptom of coronary artery disease, chest pain occurs when the heart's oxygen supply is insufficient due to blocked or narrowed arteries.
-
Shortness of breath (dyspnea): As coronary arteries become more blocked, the heart struggles to pump oxygenated blood, leading to breathlessness even during mild exertion.
-
Fatigue: Reduced cardiac output from restricted blood flow can cause fatigue and diminished stamina during physical activities.
-
Palpitations: Abnormal heart rhythms can develop in patients with CAD due to reduced oxygen supply or vessel blockages.
-
Syncope (fainting): Episodes of fainting may occur when blood flow to the brain is insufficient, particularly during physical exertion.
Symptoms in Peripheral Artery Disease (PAD):
-
Intermittent claudication: A common symptom of PAD, this is pain or cramping in the legs during walking or exercise, which goes away after rest. This pain is due to reduced blood flow to the muscles of the legs.
-
Non-healing wounds or ulcers: In patients with PAD, poor circulation can lead to slow-healing wounds, often on the legs, feet, or toes, and chronic ulcers.
-
Numbness or weakness in the limbs: Poor circulation can lead to feelings of numbness or weakness, particularly in the feet and legs.
-
Cold or pale extremities: Reduced blood flow to the extremities causes the legs or feet to feel cold, look pale, or develop a bluish tint (cyanosis).
-
Rest pain: In severe PAD, pain can occur even when at rest, typically in the feet and toes, and is an indication of significant vascular compromise.
Diagnosis of Rotational and Directional Atherectomy
The decision to perform rotational or directional atherectomy is based on diagnostic imaging, clinical symptoms, and the complexity of the arterial disease. Here's how physicians assess and diagnose the need for atherectomy:
Key Diagnostic Tools:
-
Coronary Angiography: This is the primary test for diagnosing coronary artery disease. A catheter is inserted into the coronary arteries, and contrast dye is injected to reveal blockages or narrowed arteries on X-ray images. It also helps determine the location, severity, and complexity of the lesion.
-
Intravascular Ultrasound (IVUS): IVUS provides cross-sectional images of the blood vessels, allowing physicians to measure the degree of plaque buildup and to assess its composition (fibrous vs calcified). This imaging is crucial for planning atherectomy, as calcified plaques require rotational atherectomy, while softer plaques may benefit from directional atherectomy.
-
Optical Coherence Tomography (OCT): This technique provides high-resolution imaging to visualize plaque morphology in greater detail. It is often used to assess stent placement, plaque burden, and the need for further plaque removal.
-
Peripheral Arterial Duplex Ultrasonography: For peripheral artery disease, a non-invasive duplex ultrasound is often used to measure blood flow, assess plaque buildup, and identify areas of stenosis or occlusion in the arteries.
-
Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA): Both are used to visualize peripheral arterial disease and provide more detailed, three-dimensional imaging, especially in patients with complex lesions.
-
Ankle-Brachial Index (ABI): This simple test compares blood pressure in the ankle and arm to assess the severity of PAD. A lower ABI indicates more severe disease, which may require atherectomy.
These diagnostic tools provide the necessary information to guide the interventional approach, determining whether rotational atherectomy, directional atherectomy, or another intervention will be most effective.
Treatment Options of Rotational and Directional Atherectomy
Both rotational and directional atherectomy offer specialized solutions to treat challenging arterial lesions. The selection of either technique depends on lesion characteristics, the location of the blockage, and the experience of the operator. Both procedures are minimally invasive and performed via catheterization, using small incisions in the groin or wrist.
Rotational Atherectomy:
-
Rotational atherectomy uses a diamond-coated burr that rotates at high speeds to grind away calcified plaque. The device's high rotational speed allows it to cut through rigid plaque while sparing the more elastic vessel walls.
-
It is particularly effective in treating heavily calcified lesions, which are difficult to treat with traditional balloon angioplasty alone.
-
This method allows for the debulking of plaque, making it easier to perform subsequent balloon angioplasty or stent placement.
Directional Atherectomy:
-
Directional atherectomy involves a catheter with a cutting device or shaver at the tip, which is used to excise plaque in a controlled direction. This technique is often used for focal lesions and allows for targeted plaque removal.
-
Unlike rotational atherectomy, which involves grinding plaque, directional atherectomy allows for the excavation of larger pieces of plaque, making it useful for smaller, more localized lesions.
-
Directional atherectomy can also be used for treating in-stent restenosis, where plaque build-up occurs within a previously placed stent.
Adjunctive Procedures:
-
Balloon Angioplasty: After atherectomy, balloon angioplasty is often used to further dilate the artery and prepare it for stent placement.
-
Stenting: In many cases, stent placement is required after atherectomy to maintain arterial patency and prevent restenosis.
-
Drug-Coated Balloons: In some instances, drug-coated balloons are used in conjunction with atherectomy to prevent restenosis by delivering drugs that inhibit smooth muscle proliferation.
Prevention and Management of Rotational and Directional Atherectomy
Although atherectomy is a treatment, prevention and ongoing management of atherosclerosis are key to long-term success and reducing the need for future interventions.
Prevention:
-
Risk factor modification: The foundation of preventing the progression of atherosclerotic disease includes lifestyle changes and medical therapy to control blood pressure, blood sugar, and lipid levels.
-
Smoking cessation: Smoking is one of the most significant modifiable risk factors for atherosclerosis. Quitting smoking can significantly reduce plaque formation and improve heart health.
-
Exercise: Regular exercise improves circulation, lowers blood pressure, and helps control weight, reducing the risk of arterial plaque buildup.
-
Dietary changes: A heart-healthy diet that is low in saturated fats, trans fats, and cholesterol can help reduce the progression of atherosclerosis. Increasing intake of fruits, vegetables, whole grains, and omega-3 fatty acids helps reduce cardiovascular risk.
Post-Procedure Management:
-
Antiplatelet therapy: Following atherectomy, patients are generally prescribed antiplatelet therapy (e.g., aspirin, clopidogrel) to reduce the risk of thrombosis and restenosis.
-
Routine follow-ups: Regular follow-up visits, including imaging and clinical assessments, are crucial to monitor the success of the procedure and identify any complications such as restenosis or new blockages.
-
Rehabilitation: Cardiac or vascular rehabilitation programs, especially for patients with coronary artery disease or peripheral artery disease, can help improve overall cardiovascular fitness and reduce the risk of further interventions.
Complications of Rotational and Directional Atherectomy
Although atherectomy is a minimally invasive procedure, it carries certain risks and potential complications, including:
Common Complications:
-
Embolization: During atherectomy, pieces of plaque can become dislodged and travel to distal vessels, potentially causing microvascular embolism, leading to impaired blood flow and tissue damage.
-
Vessel dissection or perforation: Aggressive plaque removal can lead to tears in the artery wall, causing dissections or perforations that may require immediate intervention, such as stenting or surgical repair.
-
Slow-flow/no-flow phenomenon: A sudden reduction in blood flow due to plaque dislodgement or vessel damage can lead to ischemic damage.
-
Restenosis: In some cases, the artery may narrow again after the procedure, requiring repeat treatment.
Specific Risks for Rotational Atherectomy:
-
Burr entrapment: The rotating burr can sometimes become stuck in the artery, requiring careful management to avoid complications.
-
Thermal injury: In rare cases, excessive friction from the rotating burr can cause thermal damage to the vessel wall.
Specific Risks for Directional Atherectomy:
-
Plaque fragmentation: Larger fragments of plaque may embolize to smaller vessels, causing microvascular blockage.
-
Incomplete plaque removal: Sometimes, directional atherectomy may not fully remove the plaque, leaving residual stenosis or plaque buildup.
Living with the Condition of Rotational and Directional Atherectomy
After undergoing rotational or directional atherectomy, patients can experience significant improvement in their symptoms, such as reduced angina, improved walking ability (in PAD cases), and increased exercise tolerance. However, living with the condition post-procedure requires ongoing management and regular follow-up care.
Post-Procedure Lifestyle:
-
Diet: A heart-healthy diet continues to be essential after atherectomy. Reducing saturated fat and cholesterol intake can help prevent plaque buildup in arteries.
-
Physical activity: Most patients can return to normal activities within weeks of the procedure, but gradual reintroduction of exercise is recommended, especially in patients with PAD.
-
Monitoring symptoms: Patients should remain vigilant for any recurrence of symptoms, such as chest pain, leg pain, or shortness of breath, which may indicate restenosis or other complications.
Psychosocial Considerations:
-
Emotional support: Dealing with heart disease or peripheral artery disease can be challenging, and patients may benefit from support groups or therapy.
-
Family education: Family members should be educated about the patient's condition, recovery process, and lifestyle changes to ensure proper support and understanding.
Top 10 Frequently Asked Questions about Rotational And Directional Atherectomy
1. What is rotational and directional atherectomy?
Rotational and directional atherectomy are minimally invasive procedures used to treat atherosclerosis or blockages in the arteries caused by plaque buildup. In these procedures, special devices are used to remove or reshape the plaque, improving blood flow and preparing the artery for further treatment, such as stenting. Both techniques are particularly useful for calcified plaque, which can be resistant to standard balloon angioplasty.
Rotational atherectomy uses a high-speed rotating burr at the end of a catheter to grind away the plaque. This burr spins rapidly within the artery, removing or shaving off hardened plaque in the process. The rotating action allows the device to break through tough, calcified deposits that might not respond to balloon angioplasty. The debris created by this action is cleared away by the bloodstream.
On the other hand, directional atherectomy involves a catheter with a cutting blade that removes the plaque by shaving off small sections. This device is designed to direct the plaque removal in a controlled manner, which can be especially beneficial when plaque is unevenly distributed or when it forms eccentric lesions, or those that are located more to one side of the artery. In directional atherectomy, the plaque is collected in a protective chamber to prevent it from traveling downstream and causing further blockages.
These techniques provide an alternative to open surgery, offering a less invasive solution to patients suffering from peripheral artery disease (PAD) or coronary artery disease (CAD) who have difficult-to-treat blockages. The choice between rotational and directional atherectomy depends on factors such as the type of plaque, the location of the blockage, and the patient's overall vascular health.
2. When and why is this procedure used?
The rotational and directional atherectomy procedures are typically used when the blockage in the arteries is resistant to traditional methods, such as balloon angioplasty. Atherosclerotic plaques—which can cause narrowing of the arteries and lead to restricted blood flow—can become calcified and hardened over time, making them less responsive to simple balloon expansion.
Atherectomy is often used in cases of severe coronary artery disease (CAD) or peripheral artery disease (PAD), particularly when patients have heavily calcified lesions that would be challenging to treat with a standard angioplasty procedure. These techniques are particularly useful in patients who have complex anatomical features, such as tortuous arteries, or when other treatments have failed.
For example, in PAD, plaque buildup in the legs or other peripheral arteries can impede blood flow, leading to pain, wounds, and even tissue damage. In such cases, atherectomy can remove or reduce the plaque burden, making it easier to perform angioplasty or place stents to restore proper blood flow.
Atherectomy is also recommended when patients have multivessel disease, where multiple areas of the vascular system are affected, requiring precise and effective plaque removal to open up all narrowed or blocked arteries.
3. What is the difference between rotational and directional atherectomy?
The main difference between rotational and directional atherectomy lies in the type of plaque removal and how the devices operate. Both methods aim to remove plaque, but they do so in slightly different ways.
-
Rotational Atherectomy: This procedure involves the use of a high-speed rotating burr that is attached to a catheter and advanced through the artery. The rotating action of the burr shaves off the calcified plaque, turning it into small particles that can be washed away by blood flow. This method is most effective when plaque is hard and calcified, making it more difficult to compress with a balloon. The rotational atherectomy technique has been shown to be particularly useful in complex, heavily calcified lesions and is often preferred when balloon angioplasty alone may not provide sufficient results.
-
Directional Atherectomy: In this technique, the catheter has a side-cutting blade that is positioned against the plaque. The blade shaves the plaque away in a controlled direction, often into a collection chamber designed to prevent embolization (where plaque fragments travel downstream and block smaller vessels). This method is ideal when the plaque is eccentric or off-center, and can be particularly helpful for targeting localized plaques that may be more challenging to treat with a rotational device. The directional approach provides greater precision and control in removing plaque and offers a more direct method of plaque removal, making it useful for certain types of lesions.
In summary, rotational atherectomy uses a spinning device to grind and remove plaque, while directional atherectomy uses a side-cutting blade to shave off plaque in a specific direction, depending on the shape and location of the blockage.
4. How is the atherectomy procedure performed?
The atherectomy procedure is performed under local anesthesia or light sedation, depending on the patient's needs and the complexity of the procedure. Typically, the procedure is carried out in a cardiac catheterization lab (cath lab), a specialized room equipped for minimally invasive surgeries.
To begin, the interventional cardiologist or vascular surgeon will insert a catheter through a small incision, usually made in the groin or wrist, to access the affected artery. Using fluoroscopic imaging (real-time X-ray), the catheter is guided to the area of blockage. Once the catheter reaches the target lesion, the surgeon uses either the rotational or directional atherectomy device to treat the plaque.
-
For rotational atherectomy, the rotating burr is carefully advanced through the artery to the plaque, where it is activated. The spinning burr shaves off the hardened plaque, creating small particles that are cleared by blood flow.
-
For directional atherectomy, the cutting blade is positioned against the plaque, and the plaque is removed in a controlled manner, with the fragments collected in a protective chamber.
After the atherectomy device has done its work, the surgeon may use balloon angioplasty to further open the artery or place a stent to keep the artery open. Once the procedure is complete, the catheter is removed, and the incision site is closed.
5. What are the benefits of rotational and directional atherectomy?
Both rotational and directional atherectomy offer significant benefits, especially in cases where traditional methods are ineffective. The primary benefits include:
-
Effective plaque removal: Both techniques allow for more complete plaque removal, particularly in calcified arteries, which are resistant to traditional angioplasty and balloon dilation.
-
Reduced need for open surgery: Atherectomy provides a minimally invasive option for treating complex arterial blockages, reducing the need for more invasive surgical interventions.
-
Improved stent placement: After plaque removal, it becomes easier to place stents, which are small mesh tubes used to keep the artery open.
-
Faster recovery: Since atherectomy is minimally invasive, patients typically experience a shorter recovery time compared to open surgery, with most patients able to return to light activities within a few days.
-
Better long-term outcomes: Atherectomy can help reduce the risk of restenosis (re-narrowing of the artery), as it removes the plaque rather than just compressing it, leading to better long-term outcomes.
6. What are the risks and complications associated with atherectomy?
While atherectomy is generally safe, there are risks and complications associated with the procedure. Some potential risks include:
-
Embolization: Small particles of plaque can break off during the procedure and travel downstream, potentially blocking smaller vessels and causing complications like heart attack or stroke.
-
Vessel injury: There is a risk of damaging the arterial wall during the procedure, leading to dissection (tear) or perforation.
-
Bleeding: As with any catheter-based procedure, there is a risk of bleeding at the catheter insertion site, particularly if the artery is not properly sealed after the procedure.
-
Stenosis recurrence: In some cases, despite successful plaque removal, the artery may narrow again over time, especially if the underlying cause of the blockage (such as high cholesterol or high blood pressure) is not properly managed.
-
Vessel spasm: The artery may spasm during the procedure, leading to temporary closure or pain.
The risks can be minimized through proper patient selection, careful technique, and appropriate follow-up care.
7. What is the recovery time for atherectomy?
The recovery time for rotational and directional atherectomy is relatively short compared to traditional surgery. Most patients can return to light activities within 1 to 2 days after the procedure. However, strenuous activities and heavy lifting should be avoided for about 2 to 4 weeks to allow the artery to heal properly. If a stent was placed during the procedure, additional precautions may be necessary to prevent complications such as blood clots. Patients are usually advised to follow up with their doctor for imaging studies to ensure the artery remains open and that no further complications have developed.
8. How long will the results of atherectomy last?
The durability of the results depends on several factors, including the location and severity of the plaque, the type of atherectomy performed, and the patient's overall health. While atherectomy removes plaque from the artery, the disease process of atherosclerosis (plaque buildup) can continue, potentially leading to restenosis (re-narrowing of the artery) over time. However, when combined with other treatments such as stenting, atherectomy can provide long-term relief and improve blood flow. Regular follow-up appointments and lifestyle changes such as managing cholesterol, blood pressure, and diabetes are essential to maintaining long-term results.
9. Who is a good candidate for atherectomy?
Candidates for rotational or directional atherectomy are typically patients with calcified, complex plaque in the arteries that cannot be adequately treated with balloon angioplasty or stenting alone. These patients may have peripheral artery disease (PAD) or coronary artery disease (CAD). Other factors such as the location of the blockage, overall cardiovascular health, and the presence of other conditions like diabetes or high blood pressure are also important considerations in determining eligibility for atherectomy.
10. What should I ask my doctor before undergoing atherectomy?
Before undergoing an atherectomy procedure, patients should ask the following questions:
-
What is the nature of my blockage, and why is atherectomy recommended over other treatments?
-
What is your experience with this procedure, and what are the success rates for patients with conditions similar to mine?
-
What type of atherectomy (rotational or directional) will be used, and why?
-
What risks are associated with this procedure, and how will complications be managed?
-
How long is the recovery time, and what activities should I avoid post-procedure?
-
Will I need additional treatments, such as stenting, after the atherectomy?
-
What follow-up care is necessary, and how will we monitor the success of the procedure?


