Introduction to Scleral Buckling Surgery
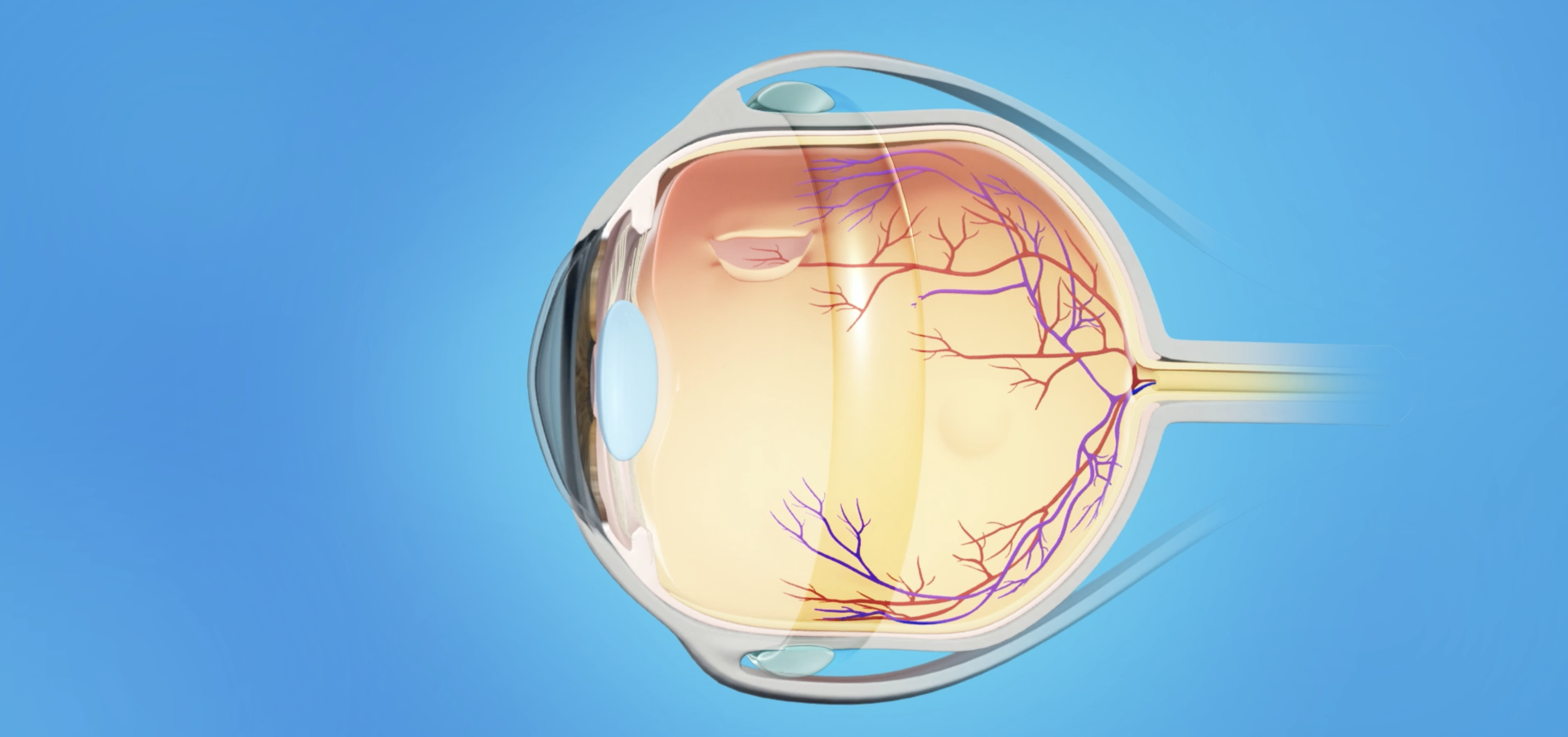
Scleral buckling surgery is a critical surgical procedure used to treat retinal detachment, a condition where the retina (the light-sensitive tissue at the back of the eye) separates from its supporting structures. This detachment can lead to permanent vision loss if not treated promptly. Retinal detachment often occurs due to a tear or hole in the retina, which allows fluid from the vitreous (gel-like substance inside the eye) to seep behind it, further separating the retina from the eye.
Scleral buckling involves the application of a silicone band (buckle) around the sclera, which is the white outer layer of the eye. The buckle creates a small indentation on the outer eye wall, helping to push the retina back into its proper position, encouraging reattachment. The surgeon also typically uses techniques like laser photocoagulation (a laser to seal retinal tears) or cryotherapy (freezing the tear site) to ensure that the retina stays attached.
While vitrectomy (removal of the vitreous) is a more commonly used procedure in modern retinal detachment surgery, scleral buckling remains highly effective, particularly for certain cases, such as detachment due to a single tear, younger patients, or when the retina is difficult to access with vitrectomy. It can be used alone or in combination with other procedures like vitrectomy, depending on the complexity and cause of the detachment.
The main advantage of scleral buckling is that it's an external approach that does not require removal of the vitreous, and it has a high success rate in preventing further detachment and restoring vision. The procedure is generally performed under local anesthesia and involves a relatively short recovery time compared to more invasive surgeries.
Causes and Risks of Scleral Buckling Surgery
Scleral buckling is used primarily to treat retinal detachment, which occurs when the retina detaches from the underlying tissue. The detachment can be caused by various factors, and understanding these risk factors is important when considering the procedure.
Primary Causes of Retinal Detachment
-
Rhegmatogenous retinal detachment (RRD): This is the most common type of retinal detachment, caused by a tear or hole in the retina. Once a tear forms, the vitreous gel inside the eye can leak behind the retina, causing it to separate. This is the primary condition for which scleral buckling is indicated.
-
Trauma or injury to the eye: Severe blows to the head or eye can cause retinal tears or detachments. Although not as common as other causes, trauma-related retinal detachments can be addressed effectively with scleral buckling.
-
Vitreous degeneration: As a person ages, the vitreous gel inside the eye shrinks and pulls away from the retina. This can lead to tears, which may eventually result in retinal detachment. This is especially common in people with high myopia (nearsightedness).
-
Previous eye surgeries: Surgical procedures, especially those involving the lens (such as cataract surgery), can weaken the retina and make it more susceptible to detachment.
Risk Factors for Retinal Detachment
-
Age: Older adults are at higher risk for retinal detachment due to natural aging processes that cause changes in the vitreous body and retina.
-
High myopia: People with severe nearsightedness have elongated eyeballs, which puts extra strain on the retina and increases the risk of tears and detachment.
-
Family history: Retinal detachment can run in families, suggesting a genetic predisposition. People with a family history of retinal detachment may be more likely to experience it themselves.
-
Previous retinal tears or detachments: If a person has had one retinal detachment, they are at a higher risk for future detachments, which may require scleral buckling surgery.
-
Trauma or injury to the eye: Any physical trauma or injury that damages the eye can increase the likelihood of a retinal tear and subsequent detachment.
-
Other eye conditions: Conditions such as diabetic retinopathy, retinal vein occlusion, or retinitis pigmentosa can increase the risk of retinal detachment due to the effects they have on the retina.
Understanding these causes and risk factors is essential for determining
whether scleral buckling is the right treatment. If retinal detachment
occurs, prompt diagnosis and treatment are crucial to preserve vision.
Symptoms and Signs of Retinal Detachment Indicating the Need for Scleral Buckling
Retinal detachment can develop suddenly, and recognizing the symptoms early is essential for timely treatment and to prevent permanent vision loss. Common symptoms and signs include:
1. Sudden Increase in Floaters
-
Floaters are small specks, cobweb-like shapes, or dots that appear in the field of vision. They are caused by tiny clumps of gel or cells inside the vitreous. When the retina is at risk of detaching, the vitreous can pull on the retina, leading to an increase in floaters.
2. Flashes of Light
-
These appear as bright streaks or flashes in the peripheral vision, usually due to the vitreous gel pulling on the retina. This symptom is typically reported as a sudden burst of light in the corner of the eye, often seen in low light conditions.
3. A Dark Curtain or Shadow
-
A significant sign of retinal detachment is the sudden appearance of a curtain or shadow across the visual field, often starting in the peripheral vision and gradually moving towards the center. This occurs when the retina detaches, cutting off the transmission of visual information from that part of the eye.
4. Blurred or Distorted Vision
-
If the macula (the central part of the retina) detaches, the vision may become blurred or distorted, leading to difficulty with reading, seeing fine details, or recognizing faces.
5. Loss of Peripheral Vision
-
Since retinal detachment often begins at the edges of the retina, a person may experience a loss of peripheral vision (side vision) that progresses over time if not treated.
6. No Pain
-
One of the most deceptive aspects of retinal detachment is that it is typically painless. Many patients don't experience discomfort, which is why the symptoms of detachment must be recognized early to seek medical attention.
If any of these symptoms occur, it is crucial to seek immediate medical attention. Retinal detachment is an ophthalmic emergency, and delayed treatment can lead to irreversible vision loss.
Diagnosis of Retinal Detachment and Scleral Buckling Surgery
The diagnosis of retinal detachment is typically made through a comprehensive eye exam performed by an ophthalmologist. Common diagnostic tests include:
1. Dilated Eye Examination
-
The ophthalmologist uses eye drops to dilate the pupil, allowing a detailed examination of the retina. This is the most common and effective way to identify retinal tears, holes, or detachments. The doctor will look for any signs of fluid under the retina or the presence of tears or breaks that may cause detachment.
2. Indirect Ophthalmoscopy
-
This is a procedure where the ophthalmologist uses a specialized lens and light source to examine the retina more thoroughly. It allows for a clearer view of the retinal surface, helping identify tears or detachments.
3. Optical Coherence Tomography (OCT)
-
This non-invasive imaging technique produces cross-sectional images of the retina, allowing the doctor to detect subtle retinal detachment and examine the depth of the detachment or any accompanying macular edema (swelling).
4. Ultrasound (B-Scan)
-
If the view of the retina is obscured due to blood or cataracts, an ultrasound may be used to get a more detailed view of the retina's condition.
5. Fluorescein Angiography
-
This test is performed by injecting a fluorescent dye into a vein, which is then tracked as it travels to the retina. The dye helps highlight areas of fluid accumulation and retinal tears that may not be visible during a standard exam.
Once diagnosed, a retina specialist will assess the severity and type of detachment and determine the best course of treatment, which may include scleral buckling surgery, vitrectomy, or other surgical options.
Treatment Options for Retinal Detachment and Scleral BucklingSurgery
The treatment for retinal detachment depends on the type of detachment, its location, and severity. Here are the primary treatment options:
Scleral Buckling Surgery
-
Scleral buckling is a standard treatment for rhegmatogenous retinal detachment, where tears or holes in the retina allow fluid to accumulate behind the retina. During the procedure, a silicone band or sponge is placed around the eye to create an indentation on the sclera. This helps to reposition the retina and press it back against the underlying tissue. The procedure is often combined with laser photocoagulation or cryotherapy to seal retinal tears and prevent further fluid buildup.
Vitrectomy
-
A vitrectomy is a surgical procedure where the surgeon removes the vitreous gel that is pulling on the retina. This is followed by the reattachment of the retina, often with the help of a gas bubble that temporarily holds the retina in place while it heals. Vitrectomy is commonly performed in conjunction with scleral buckling for more complex detachments.
Laser Treatment (Laser Photocoagulation)
-
In cases where there are small retinal tears or areas of fluid leakage, laser photocoagulation can be used to create small burns around the tear site. This helps to seal the break, preventing fluid from entering and causing further detachment. It is often used in conjunction with scleral buckling or vitrectomy.
Cryotherapy
-
Cryotherapy involves using freezing probes to treat retinal tears. The freezing process creates a scar around the tear, helping to seal it and prevent further fluid from accumulating beneath the retina.
Gas or Silicone Oil Injection
-
In certain cases, a gas bubble or silicone oil may be injected into the eye to push the retina back into place and help it reattach. The gas or oil remains in the eye for several weeks, gradually being absorbed by the body as the retina heals.
Prevention and Management of Scleral Buckling Surgery
While retinal detachment can't always be prevented, there are ways to reduce the risk and manage the condition effectively after surgery.
Before Surgery: Risk Mitigation
-
Regular eye exams are crucial for individuals at high risk, such as those with high myopia, a family history of retinal detachment, or prior eye surgeries. Early detection of retinal tears can prevent detachment from occurring.
-
Protecting the eyes from trauma is essential, especially for individuals who engage in high-contact sports or other activities that may pose a risk of eye injury.
After Surgery: Post-Operative Care
-
Follow-up visits with the surgeon are necessary to monitor the healing process and ensure the retina remains attached.
-
Post-operative medications, such as antibiotics and anti-inflammatory eye drops, are typically prescribed to prevent infection and reduce swelling.
-
Eye protection: Patients should wear protective eye shields and avoid rubbing or pressing on the eye to reduce the risk of complications.
Long-Term Management
-
Eye health monitoring: Regular eye exams are essential to ensure the retina stays attached, especially if there is a history of detachment in one eye.
-
Vision rehabilitation: If there has been significant vision loss due to the detachment, vision rehabilitation therapies may be necessary.
Complications of Scleral Buckling Surgery
While scleral buckling surgery has a high success rate, it is not without potential risks and complications. Some of the common complications include:
-
Recurrence of retinal detachment: In some cases, the retina may detach again, particularly if there are new tears, insufficient sealing, or external factors such as trauma.
-
Infection: As with any surgery, there is a risk of infection. Post-operative care, including the use of antibiotics, helps minimize this risk.
-
Elevated intraocular pressure (IOP): The procedure can lead to an increase in eye pressure, which can contribute to glaucoma. Regular monitoring of eye pressure is crucial.
-
Vision changes: Scleral buckling can sometimes lead to an increase in nearsightedness (myopia), as the surgery can change the shape of the eye.
-
Double vision: In rare cases, patients may experience double vision if the buckle affects eye alignment.
-
Buckle complications: In rare cases, the silicone band can cause discomfort, become displaced, or lead to scarring of the conjunctiva (the membrane covering the eye).
Living with the Condition After Scleral Buckling Surgery
After undergoing scleral buckling surgery, many patients experience significant improvements in vision, but some adjustments and care are necessary.
Recovery Process
-
Immediate Recovery: Patients typically spend 1-2 hours in the recovery room after surgery before being sent home. Eye discomfort, redness, and mild swelling are common in the first few days.
-
Visual Recovery: Vision may improve gradually over several weeks to months, but full recovery may take several months, depending on the severity of the detachment and involvement of the macula (the central part of the retina).
-
Follow-up Visits: Regular visits to the ophthalmologist will be required to monitor healing, check for any complications, and ensure the retina remains securely attached.
Long-Term Outlook
-
Vision Stability: Many patients regain functional vision, although some may experience ongoing distortion or reduced visual acuity, particularly if the macula was involved in the detachment.
-
Psychosocial Impact: Successful retinal repair can significantly improve a patient's quality of life, but adjustments to lifestyle and vision may still be needed, such as using glasses or coping with mild visual distortions.
Top 10 Frequently Asked Questions about Scleral Buckling Surgery
1. What is scleral buckling surgery?
Scleral buckling surgery is a procedure used to treat retinal detachment, a serious eye condition where the retina (the light-sensitive layer at the back of the eye) becomes separated from its underlying supportive tissue. In scleral buckling, a silicone band is placed around the outside of the eye, specifically the sclera (the white part of the eye), to gently push the wall of the eye inward. This helps to relieve the tension on the retina, allowing it to reattach to the back of the eye.
The surgery may also involve other techniques, such as laser treatment or freezing (cryotherapy), to seal retinal tears or holes that caused the detachment.
2. Why is scleral buckling surgery performed?
Scleral buckling surgery is performed to treat retinal detachment, which can occur due to various factors such as:
-
Trauma or injury to the eye
-
Retinal tears or holes caused by aging or other underlying eye conditions
-
High myopia (nearsightedness)
-
Diabetic retinopathy
-
Posterior vitreous detachment (PVD)
If left untreated, retinal detachment can lead to permanent vision loss, so scleral buckling surgery is essential to prevent further damage and reattach the retina.
3. How is scleral buckling surgery performed?
Scleral buckling is typically performed under local anesthesia, which numbs the eye area, and in some cases, sedation may also be used to ensure the patient is relaxed. Here's how the procedure generally works:
-
The surgeon creates small incisions in the eye or around the eye.
-
A silicone band (the buckling material) is placed around the sclera (the white part of the eye) to gently push the eye wall inward.
-
If there are tears or holes in the retina, the surgeon may use laser treatment or cryotherapy to seal them.
-
The silicone band is secured, and the eye is carefully closed.
-
A gas bubble may be placed in the eye to help keep the retina in place while healing.
The surgery generally lasts about 1 to 2 hours, and the patient may need to stay in the hospital for 1 day or more, depending on individual circumstances.
4. What is the recovery process after scleral buckling surgery?
After scleral buckling surgery, the recovery process typically involves the following:
-
Initial recovery: Most patients are able to go home the same day or the next day, depending on the procedure.
-
Post-surgical discomfort: You may experience mild pain, redness, and swelling around the eye for a few days. Cold compresses and prescribed pain medications can help alleviate discomfort.
-
Positioning: In some cases, the surgeon may ask the patient to maintain a certain head position (such as lying face down) to ensure that the gas bubble stays in the correct position for healing. This is generally for about 2 to 3 weeks.
-
Follow-up appointments: Regular follow-ups are crucial to monitor the healing process and check for potential complications.
-
Vision recovery: Vision may be blurry initially, but it typically improves as the retina heals. Complete vision recovery can take several weeks to months.
It is important to follow the surgeon's post-operative care instructions carefully to ensure optimal healing.
5. What are the risks and complications associated with scleral buckling surgery?
As with any surgery, scleral buckling carries some risks, including:
-
Infection: Any surgical procedure carries the risk of infection, although this is rare.
-
Glaucoma: The surgery can sometimes lead to increased intraocular pressure, which may cause glaucoma.
-
Retinal re-detachment: In some cases, the retina may re-detach after surgery, requiring additional treatments.
-
Visual disturbances: Some patients may experience double vision or difficulty focusing after the procedure.
-
Ocular complications: The band placed on the eye could cause discomfort, change in eye shape, or affect eye movement.
Your surgeon will take steps to minimize these risks and discuss potential complications during your consultation.
6. Will I need to stay in the hospital after scleral buckling surgery?
In most cases, scleral buckling surgery is performed on an outpatient basis, and patients are able to return home on the same day or after one night in the hospital. If you have had complications or if your surgeon feels it's necessary, you may need to stay for a longer period.
The decision to stay in the hospital depends on the surgeon's recommendation, the complexity of the surgery, and your overall health.
7. How long will it take to see results after scleral buckling surgery?
The full effects of scleral buckling surgery take time to become apparent. The initial recovery period usually takes about 1 to 2 weeks, during which any swelling or discomfort should begin to subside. However, it may take several months for the retina to fully heal and for vision to stabilize. The outcome of surgery can be influenced by the severity of the retinal detachment, the size of the detachment, and the presence of any other eye conditions.
Vision may improve gradually as the retina heals, and most patients will need to return for follow-up exams to monitor progress.
8. Can scleral buckling surgery be combined with other treatments?
Yes, scleral buckling surgery is often performed in conjunction with other treatments for retinal detachment, such as:
-
Vitrectomy: A procedure that involves removing the vitreous gel from the eye to clear up any debris and help reattach the retina.
-
Laser therapy: Often used to seal any holes or tears in the retina.
-
Cryotherapy: Freezing treatment to seal retinal tears or holes.
-
Gas or silicone oil tamponade: A gas bubble or silicone oil is often used to press against the retina to keep it in place during healing.
Your surgeon will evaluate the best treatment approach for your individual case based on the severity of the detachment and any other underlying issues.
9. How much does scleral buckling surgery cost?
The cost of scleral buckling surgery can vary based on several factors:
-
Location of the surgery
-
Surgeon's experience and expertise
-
Hospital or surgical center fees
-
Whether the surgery is combined with other procedures (e.g., vitrectomy)
On average, scleral buckling surgery can cost between $3,000 and $6,000 per eye. It's important to check with your insurance provider to determine if the procedure is covered under your plan, especially if the surgery is necessary due to retinal detachment.
10. Will I be able to return to normal activities after scleral buckling surgery?
After scleral buckling surgery, most patients can resume light activities within 1–2 weeks. However, it's important to avoid:
-
Strenuous activities (e.g., heavy lifting, intense exercise) for about 4–6 weeks to prevent pressure on the eye.
-
Direct exposure to sunlight without protective sunglasses to shield the eyes.
-
Rubbing or pressing on the eye during recovery.
Follow-up appointments are crucial to monitor the progress of your recovery and ensure the retina remains attached. Your surgeon will guide you on when it's safe to fully return to regular activities, including driving.


