Introduction to Segmental/Partial Cystectomy
A segmental or partial cystectomy is a surgical procedure that involves the removal of a part of the bladder, typically when a tumor or disease is localized to a specific area. Unlike a radical cystectomy, where the entire bladder is removed, partial cystectomy preserves a significant portion of the bladder. This approach allows for the removal of diseased tissue while maintaining the patient's ability to pass urine naturally, without the need for urinary diversion (such as a stoma or catheter).
This surgery is typically performed in patients diagnosed with bladder cancer where the tumor is confined to a specific area of the bladder and hasn't spread to other parts of the bladder or surrounding tissues. Partial cystectomy is often preferred when the tumor is located in a specific segment of the bladder, allowing the surgeon to remove just the affected portion while preserving the rest of the bladder. The goal of this surgery is not only to remove the tumor but to maintain bladder function and reduce the risk of recurrence.
Partial cystectomy is a less invasive approach than a full cystectomy, and it offers the advantage of retaining bladder capacity and function. The procedure may also be combined with lymph node dissection to assess for potential spread of cancer, ensuring that the surgery is as effective as possible. This surgery can be done through traditional open surgery or with minimally invasive techniques such as laparoscopic or robot-assisted surgery, depending on the location of the tumor, the patient's health, and the surgeon's expertise.
Causes and Risk Factors Leading to Partial Cystectomy
Partial cystectomy is commonly performed to treat bladder cancer, but it is also considered for other conditions that cause localized damage to the bladder. Several conditions and factors increase the need for this surgery, and they include:
Bladder Cancer:
The most common reason for performing a partial cystectomy is bladder cancer, which often presents as a localized tumor. The cancer may be confined to a small region of the bladder, and if detected early, it can be successfully treated by removing just the affected portion. This is particularly beneficial for patients who are young, in good health, or want to avoid the more drastic measure of radical cystectomy.
Non-cancerous Tumors:
In some cases, benign tumors or growths in the bladder can cause significant symptoms or damage. These tumors may include bladder polyps, fibroids, or bladder diverticula (small pouches that form in the bladder wall). If these growths are localized and causing discomfort or other issues, partial cystectomy may be recommended to remove the abnormal tissue while preserving the rest of the bladder.
Bladder Trauma:
If a person experiences severe trauma to the bladder, such as from an accident or injury, localized damage may require surgical intervention. When the damage is confined to a specific area of the bladder, partial cystectomy can be performed to remove the injured portion, allowing for functional recovery.
Urinary Tract Infections (UTIs):
In some cases, recurrent or severe infections of the bladder may cause inflammation and damage to the bladder lining. While most UTIs are treated with antibiotics, if an infection leads to the development of bladder diverticula or damage to the bladder wall, a partial cystectomy may be necessary.
Bladder Diverticula:
Bladder diverticula are small, balloon-like pouches that form in the bladder wall. These can be congenital (present at birth) or acquired due to chronic pressure in the bladder. When diverticula cause symptoms such as pain, infections, or retention of urine, partial cystectomy may be required to remove the affected part of the bladder.
Symptoms and Signs of Segmental/Partial Cystectomy
The primary symptom that leads to the consideration of partial cystectomy is often hematuria (blood in the urine). Other common signs and symptoms include:
-
Visible Blood in Urine (Hematuria): One of the most common signs of bladder cancer or significant bladder pathology is blood in the urine. This can either be gross hematuria (visible to the naked eye) or microscopic hematuria (only visible under a microscope). Hematuria is often the reason that patients seek medical attention and may prompt imaging and diagnostic procedures, including cystoscopy and biopsy, which could lead to the diagnosis of bladder cancer and the need for partial cystectomy.
-
Painful Urination: Patients may experience discomfort or pain when urinating, especially if the bladder is inflamed or infected, or if there is a tumor pressing against the bladder walls. This pain, known as dysuria, can be a sign of a more serious bladder condition requiring surgical intervention.
-
Frequent Urination or Urgency: Increased frequency or urgency to urinate, especially if accompanied by discomfort or incomplete bladder emptying, may signal an issue with the bladder, such as a mass or obstruction. These symptoms often prompt further testing and imaging to evaluate the underlying cause.
-
Pelvic Pain or Pressure: Patients may feel a dull, constant pain or pressure in the lower abdomen or pelvic area, which may be caused by a mass or abnormal growth in the bladder. This can be particularly concerning if the pain is persistent and is not relieved by typical treatments.
-
Urinary Retention: In some cases, the bladder may have difficulty emptying due to an obstruction, tumor, or other condition. This can lead to urinary retention, which can cause discomfort and increase the risk of infection.
-
Unexplained Weight Loss or Fatigue: Advanced stages of bladder cancer or other significant bladder conditions may cause systemic symptoms such as weight loss, fatigue, or weakness. While not always present, these symptoms may indicate the progression of disease, leading to a recommendation for partial cystectomy.
Diagnosis of Segmental/Partial Cystectomy
Before partial cystectomy is performed, a thorough diagnostic work-up is essential to evaluate the extent of the disease, ensure the suitability of the patient for surgery, and plan the best approach. Diagnostic methods include:
Cystoscopy:
A cystoscopy is a procedure in which a thin, flexible tube with a camera (cystoscope) is inserted into the bladder through the urethra. This allows the surgeon to directly visualize the bladder and any tumors or abnormalities. Cystoscopy is typically used to confirm the diagnosis and determine the tumor's location, size, and appearance. A biopsy may also be performed during cystoscopy to obtain a tissue sample for analysis.
Imaging Studies:
-
CT Urogram: A CT urogram is a specialized type of CT scan that provides detailed images of the bladder, kidneys, and urinary tract. This imaging study helps evaluate the size of the tumor, whether it has spread to nearby structures, and whether lymph nodes are involved.
-
MRI: Magnetic resonance imaging (MRI) can also be used to assess the extent of the tumor and its relation to surrounding tissues. MRI is particularly useful in evaluating deeper tissue involvement and in patients who cannot tolerate CT scans due to contrast allergies or other issues.
Ultrasound:
Ultrasound imaging may be used to assess the size and structure of the bladder, detect masses, and evaluate bladder wall thickness. This non-invasive test can also help identify signs of obstruction or other structural abnormalities.
Biopsy:
If a tumor is detected, a biopsy is performed to confirm whether the lesion is benign or malignant. This can be done via transurethral resection during cystoscopy or through a needle biopsy if needed. The biopsy results are critical for determining the treatment approach and whether partial cystectomy is appropriate.
Blood Tests:
Blood tests are routinely performed before surgery to evaluate kidney function, liver enzymes, and to check for any signs of infection or anemia. Blood tests are essential to ensure that the patient is fit for surgery.
Treatment Options of Segmental/Partial Cystectomy
The main treatment for localized bladder tumors is partial cystectomy. However, the decision to proceed with this surgery depends on various factors, including tumor location, patient health, and surgical goals. Here are the main options and approaches for treatment:
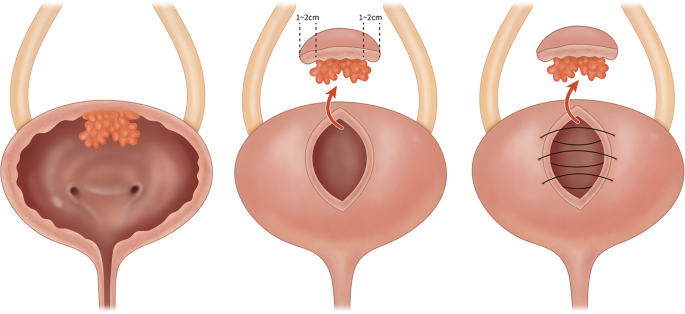
Partial Cystectomy (Segmental Bladder Resection):
As mentioned earlier, partial cystectomy is the removal of a portion of the bladder affected by a tumor or disease while leaving the remainder of the bladder intact. This allows the patient to continue using their bladder for normal urination without the need for a urinary diversion.
-
Surgical Approach: The surgery can be done through traditional open surgery or using laparoscopic or robot-assisted techniques. Minimally invasive approaches generally offer quicker recovery, less postoperative pain, and fewer complications, but not all tumors are suitable for this approach.
-
Lymph Node Dissection: In some cases, pelvic lymph node dissection is also performed to check for the spread of cancer and provide more accurate staging. This is typically done during partial cystectomy if the tumor is suspected to have spread beyond the bladder.
Adjuvant Therapies:
In addition to surgery, some patients may receive adjuvant therapies such as chemotherapy, radiation therapy, or immunotherapy. These treatments may be used to shrink tumors before surgery or to treat any remaining cancer cells postoperatively.
-
Chemotherapy: Chemotherapy may be used in cases of invasive cancer or when there is a risk that the cancer has spread beyond the bladder.
-
Intravesical Therapy: After partial cystectomy, some patients may receive intravesical chemotherapy, where drugs are delivered directly into the bladder to prevent cancer recurrence.
Prevention and Management of Segmental/Partial Cystectomy
While partial cystectomy cannot always be "prevented," certain lifestyle choices and management techniques can reduce the risk of complications and recurrence.
Preoperative Management:
-
Optimizing General Health: Ensuring that the patient is in the best possible health before surgery is critical. This includes managing any existing health conditions, maintaining a healthy weight, and improving nutritional status.
-
Preoperative Counseling: Patients are informed about the procedure, the potential risks, the need for follow-up care, and the possibility of recurrence. They are also counseled about changes in bladder function post-surgery, such as reduced bladder capacity.
Postoperative Management:
-
Bladder Care: Following surgery, patients need to manage their bladder function carefully. This includes monitoring for signs of infection, urinary retention, or changes in voiding patterns.
-
Follow-up Care: Regular follow-up visits are essential to monitor for cancer recurrence. Cystoscopy is typically performed every 3 to 6 months after surgery for the first few years, followed by annual follow-up.
Managing Complications:
-
Infections: Patients need to be vigilant about infections, particularly urinary tract infections (UTIs), which can complicate recovery. Antibiotics are prescribed when necessary.
-
Bladder Function: Patients are often advised to perform bladder training and pelvic floor exercises to maintain or improve bladder function.
Complications of Segmental/Partial Cystectomy
Although partial cystectomy is generally well-tolerated, like all surgeries, it carries some risks and complications, including:
-
Infection: The risk of infection is present, especially in the bladder, surgical site, or urinary tract.
-
Bleeding: Significant bleeding can occur during surgery, especially if there is involvement of blood vessels near the bladder.
-
Bladder Dysfunction: After partial cystectomy, the bladder may not function as efficiently as it did prior to surgery. Patients may experience urinary frequency, urgency, or retention.
-
Recurrence of Cancer: Even after a successful partial cystectomy, there is always a risk that cancer may recur either at the site of surgery or elsewhere in the bladder.
-
Damage to Surrounding Organs: The surgery may unintentionally affect surrounding structures, such as the ureters (the tubes that carry urine from the kidneys to the bladder) or pelvic organs.
Living with the Condition After Partial Cystectomy
Life after partial cystectomy involves recovery, regular monitoring, and ongoing adjustments to urinary function. While most patients can retain normal bladder function, some may need to adapt to changes in bladder capacity or voiding patterns.
Recovery:
-
The recovery time after partial cystectomy varies, but most patients spend several days in the hospital. Physical recovery involves avoiding strenuous activity for a few weeks and following instructions for managing post-surgery bladder function.
Follow-up:
-
Long-term follow-up is crucial. Patients need regular cystoscopy examinations and urine tests to detect recurrence. The first few years after surgery typically require more frequent monitoring.
Top 10 Frequently Asked Questions about Segmental/Partial Cystectomy
1. What is a segmental/partial cystectomy?
A segmental or partial cystectomy is a surgical procedure in which a portion of the bladder is removed. This surgery is typically performed to treat conditions such as bladder cancer, benign bladder tumors, or other serious bladder conditions. During a partial cystectomy, the surgeon removes the affected part of the bladder while preserving the rest of the organ. This approach is beneficial in preserving bladder function and reducing the risk of needing a more invasive procedure, such as a total cystectomy (removal of the entire bladder).
2. Why is a partial cystectomy performed?
A partial cystectomy is performed for several reasons, including:
-
Bladder cancer: When cancer is confined to a localized area of the bladder, a partial cystectomy can remove the tumor while preserving the bladder's function.
-
Benign tumors or growths: Non-cancerous tumors or masses that may be causing bleeding, pain, or obstruction in the bladder can be removed through partial cystectomy.
-
Bladder trauma or injury: In some cases, significant trauma or injury to the bladder may require the removal of the damaged portion.
-
Prevention: In certain conditions, partial cystectomy may be done to prevent the spread of disease, particularly if the cancer is localized and operable.
3. How is a segmental/partial cystectomy performed?
The procedure is typically done under general anesthesia. The surgeon may use one of the following approaches:
-
Open surgery: A larger incision is made in the lower abdomen to access the bladder and remove the affected portion.
-
Laparoscopic surgery (minimally invasive): This involves small incisions through which the surgeon inserts a camera and specialized instruments to remove the affected tissue. Laparoscopic surgery usually results in less post-operative pain, faster recovery, and smaller scars.
During the surgery, the surgeon carefully removes the diseased portion of the bladder while preserving the rest of the organ. The remaining healthy tissue is reconnected, ensuring the bladder continues to function as normally as possible.
4. What is the recovery process like after partial cystectomy?
Recovery time after partial cystectomy varies depending on the type of surgery performed:
-
Open surgery: The recovery time is generally longer, with patients staying in the hospital for 4-7 days. It may take 4 to 6 weeks to fully recover, during which patients should avoid strenuous activities.
-
Laparoscopic surgery: Recovery is typically quicker, with most patients being able to go home within 1 to 2 days. Full recovery may take 2-4 weeks.
Patients can expect some discomfort, including abdominal pain, swelling, and possibly urinary urgency or frequency as the bladder heals. Pain management, wound care, and rehabilitation are essential to a smooth recovery. Regular follow-up visits with the surgeon are necessary to monitor progress and address any complications.
5. What are the risks and complications associated with a segmental/partial cystectomy?
As with any surgery, partial cystectomy carries some risks, including:
-
Infection: There's a risk of infection at the surgical site, in the urinary tract, or within the bladder itself.
-
Bleeding: Excessive bleeding may occur during or after surgery, especially if the surgery is complex or involves a large portion of the bladder.
-
Urinary leakage: After the removal of a portion of the bladder, there is a small risk that urine may leak from the surgical site, requiring further treatment.
-
Damage to surrounding organs: There's a slight risk of injury to nearby organs, such as the intestines, ureters, or blood vessels, during the procedure.
-
Recurrence of cancer: If the cystectomy is being performed for bladder cancer, there is a risk of the cancer returning, even after the affected tissue is removed. Regular follow-up appointments and screenings are necessary.
6. What are the benefits of segmental/partial cystectomy over a total cystectomy?
The main advantage of partial cystectomy over total cystectomy is the preservation of the bladder. Removing only the affected portion allows the bladder to remain intact, which means patients can maintain normal urinary function in most cases. Benefits include:
-
Less invasive: Since only a part of the bladder is removed, the surgery is less invasive than a total cystectomy.
-
Better quality of life: Preserving the bladder reduces the need for urinary diversion (creating a new pathway for urine to exit the body) and allows for more normal urination.
-
Shorter recovery time: Patients typically experience a quicker recovery than with a total cystectomy, as less tissue is removed.
7. How long does it take to see the results after partial cystectomy?
The primary result of a partial cystectomy is the removal of the diseased tissue, which should help prevent cancer recurrence or resolve other bladder-related issues. The immediate results are seen in the days following surgery, as the bladder heals. However, the full benefits of the surgery — such as improved bladder function and cancer control — may take several weeks to months to become fully evident.
If the procedure was done to treat bladder cancer, regular follow-up exams will be necessary to monitor for recurrence. Imaging tests, cystoscopies (bladder exams), and urine tests will help assess the long-term success of the procedure.
8. Will I need a catheter after partial cystectomy?
Yes, it is common for patients to need a catheter after surgery, especially if the bladder needs time to heal. A catheter is typically placed in the bladder to allow for urinary drainage and to prevent any strain on the healing tissues. In many cases, the catheter is removed within 7-14 days, depending on the healing progress and the surgeon's instructions. Some patients may need a catheter for a longer period if there are complications with bladder function.
9. Can partial cystectomy be used for all bladder conditions?
No, partial cystectomy is generally reserved for localized conditions that affect only a portion of the bladder. Common conditions treated with this approach include:
-
Bladder cancer (if the tumor is confined to a small area)
-
Benign bladder tumors (non-cancerous growths)
-
Bladder trauma or injury (where only a part of the bladder is damaged)
If the entire bladder is diseased or cancerous, a total cystectomy (removal of the whole bladder) may be required. Your surgeon will determine the appropriate procedure based on your individual condition and the extent of the disease.
10. What is the long-term outlook after partial cystectomy?
The long-term outlook after partial cystectomy depends largely on the condition being treated, as well as the success of the surgery. If the procedure is done to treat bladder cancer, follow-up care is crucial to monitor for recurrence. In most cases, patients who undergo partial cystectomy for localized bladder cancer have a good chance of long-term survival, particularly if the cancer is caught early and fully removed.
For patients undergoing the procedure for non-cancerous conditions, the outlook is generally positive, with a good chance of preserving bladder function and improving symptoms. Patients are typically monitored regularly through imaging, cystoscopy, and urine tests to ensure that the bladder is healing properly and that no further issues arise.


