Introduction to Spinal Column Reconstruction
Spinal column reconstruction refers to a set of complex surgical procedures aimed at restoring the structure, alignment, and function of the spine when it has been compromised by injury, degeneration, deformity, or disease. The spine plays a crucial role in providing structural support to the body, protecting the spinal cord, and allowing movement. When spinal structures such as vertebrae, intervertebral discs, ligaments, or nerves are damaged, they can lead to pain, loss of function, or even permanent disability.
Spinal column reconstruction can involve a variety of surgical techniques, including spinal fusion, vertebral body replacement, decompression procedures, and instrumentation such as screws, plates, and rods to stabilize and align the spine. The goal of the surgery is not only to alleviate pain but also to restore the spine's mechanical function, prevent further degeneration, and improve the patient's overall quality of life. These procedures are often used when more conservative treatments, such as physical therapy or medications, have failed.
This surgery is particularly important for individuals with severe spinal disorders such as scoliosis, kyphosis, spinal fractures, degenerative disc disease, or spinal tumors, where preserving the stability and functionality of the spine is essential to overall well-being.
Causes and Risk Factors Leading to Spinal Column Reconstruction
Several conditions, both congenital and acquired, can lead to the need for spinal column reconstruction. These include:
Spinal Deformities
-
Scoliosis: A condition characterized by an abnormal sideways curvature of the spine, typically diagnosed in adolescence. Severe scoliosis can cause the vertebrae to rotate, leading to reduced lung capacity, nerve compression, and back pain.
-
Kyphosis: This refers to an exaggerated forward curvature of the upper back, often referred to as “hunchback.” It may develop due to aging, degenerative diseases, or congenital defects.
Degenerative Disc Disease
As people age, the intervertebral discs, which provide cushioning and support between the vertebrae, can degenerate. This degeneration leads to loss of height in the discs, bone-on-bone friction, and potential instability of the spinal column. In severe cases, spinal fusion or disc replacement may be required to stabilize the spine.
Spinal Fractures or Trauma
Trauma from accidents, falls, or sports injuries can result in fractures of the vertebrae, which may lead to spinal instability, misalignment, or nerve compression. Fractures can also cause permanent damage to the spinal cord, necessitating reconstruction to prevent further neurological impairment.
Spinal Tumors or Infections
Spinal tumors, whether malignant or benign, can destroy vertebral tissue, compress spinal nerves, and cause severe pain. Infections such as osteomyelitis (bone infection) can also degrade the integrity of the spine and may require both surgical removal of the tumor or infected bone and spinal reconstruction.
Spondylolisthesis
Spondylolisthesis is a condition where one vertebra slips forward over the one below it, often due to degenerative changes or a previous spinal injury. This slippage can lead to instability, nerve compression, and severe pain. Spinal reconstruction, often with fusion, is needed to correct the misalignment and prevent further slippage.
Symptoms and Signs Indicating the Need for Spinal Column Reconstruction
The need for spinal column reconstruction is often driven by symptoms of spinal instability, nerve compression, or severe pain. Common symptoms that may indicate the need for reconstruction include:
-
Chronic Back Pain: Persistent or worsening pain that does not respond to conservative treatments like physical therapy or medications.
-
Neck or Limb Pain: Radiating pain from the neck to the arms or from the lower back down to the legs, often caused by nerve compression due to disc herniation, spinal stenosis, or vertebral slippage.
-
Numbness, Weakness, or Tingling: A sensation of numbness, weakness, or tingling in the arms, legs, or hands, which may indicate nerve root compression or damage to the spinal cord.
-
Impaired Mobility: Difficulty in moving or performing routine activities due to spinal instability or deformity.
-
Spinal Deformity: Visible curvature of the spine, such as in scoliosis or kyphosis, which affects posture and can lead to complications such as difficulty breathing or increased pain.
-
Bowel or Bladder Dysfunction: Difficulty controlling bladder or bowel functions can be a sign of severe nerve compression and requires immediate surgical intervention to avoid permanent damage.
-
Inability to Perform Daily Activities: Loss of function due to pain or instability that affects the ability to walk, stand, or lift objects.
When any of these symptoms are present, especially when they affect quality of life or pose a risk to neurological function, spinal column reconstruction may be necessary.
Diagnosis and Evaluation for Spinal Column Reconstruction
A thorough diagnostic process is essential for identifying the underlying cause of spinal issues and determining the best course of treatment. The diagnosis for spinal column reconstruction typically involves:
Medical History and Physical Examination
A detailed medical history helps identify any past injuries, surgeries, or conditions that may have contributed to spinal issues. Physical examinations evaluate posture, range of motion, reflexes, muscle strength, and sensory function.
Imaging Techniques
-
X-rays: Used to assess the alignment, curvature, and structure of the spine, as well as to identify fractures, degenerative changes, or signs of instability.
-
CT Scans: Provide detailed cross-sectional images of the spine to help identify bone damage, fractures, or abnormalities that may not be visible on X-rays.
-
MRI (Magnetic Resonance Imaging): Offers detailed images of the soft tissues, including intervertebral discs, ligaments, and nerve roots, to detect issues like disc herniation, spinal stenosis, or nerve compression.
-
Bone Scans: Useful in identifying infections or tumors affecting the vertebrae and spine.
-
Myelogram: An imaging procedure involving an injection of dye into the spinal canal to evaluate the spine and nerve roots for pressure or blockage.
Electrodiagnostic Tests
In cases where nerve involvement is suspected, nerve conduction studies or electromyography (EMG) may be used to assess nerve function and identify any damage or compression.
Treatment Options for Spinal Column Reconstruction
Spinal column reconstruction involves various surgical techniques aimed at restoring the spine's function and stability. The treatment plan is tailored based on the specific condition and severity of the spinal issue.
Spinal Fusion
The most common technique used in spinal column reconstruction. In spinal fusion, two or more vertebrae are permanently joined together using bone grafts, metal rods, screws, and plates. This procedure eliminates motion at the affected spinal segment and helps stabilize the spine.
Vertebral Body Replacement (Corpectomy)
When a vertebra is severely damaged, it may be removed and replaced with a prosthetic device or bone graft. This is often necessary in cases of vertebral fractures, tumors, or severe disc degeneration. The adjacent vertebrae are then fused to provide stability.
Decompression Surgery
Decompression surgery is performed to relieve pressure on the spinal cord or nerve roots. This procedure may involve removing portions of the intervertebral discs, bone spurs, or herniated discs. Decompression is often combined with spinal fusion or other stabilization techniques.
Instrumentation and Stabilization
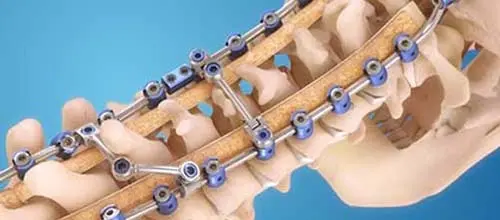
To maintain spinal alignment, screws, rods, plates, or cages are used. These devices stabilize the spine during the healing process, allowing bone fusion or vertebral replacement to take place effectively.
Corrective Surgery for Spinal Deformities
In patients with scoliosis, kyphosis, or other deformities, spinal reconstruction may involve correcting the curvature of the spine. This is achieved by performing osteotomies (cutting and reshaping bones), and then realigning the spine using metal rods and screws.
Minimally Invasive Surgery
In some cases, minimally invasive techniques are used, such as smaller incisions and specialized instruments, which lead to reduced recovery time, less pain, and a lower risk of complications.
Prevention and Management of Spinal Column Disorders
Preventing the need for spinal column reconstruction is not always possible, but there are steps that can be taken to minimize risk factors for spinal problems:
Maintain a Healthy Spine
-
Regular exercise to strengthen the muscles that support the spine, improve flexibility, and promote good posture.
-
Proper ergonomics at work, including using a supportive chair, keeping the back straight, and avoiding prolonged sitting or standing.
-
Healthy diet with adequate calcium, vitamin D, and nutrients for bone health, and maintaining a healthy weight to reduce strain on the spine.
Early Diagnosis and Treatment
If symptoms of spinal issues such as back pain, numbness, or weakness occur, seeking early medical advice can prevent further complications and may delay the need for reconstructive surgery.
Physical Therapy
For individuals with mild to moderate spinal issues, physical therapy and chiropractic care can help improve mobility, reduce pain, and avoid the progression of conditions that could require reconstruction.
Medical Management
For degenerative conditions like disc disease or arthritis, medications, anti-inflammatory drugs, and pain management therapies may help control symptoms and slow disease progression.
Complications of Spinal Column Reconstruction
Like any major surgery, spinal column reconstruction carries risks. The potential complications include:
Infection
Post-surgical infection can affect the wound, bone, or deeper structures, and may require antibiotics or even further surgery to treat.
Blood Loss and Clots
Major surgery on the spine may cause significant blood loss. Blood clots, such as deep vein thrombosis (DVT) or pulmonary embolism (PE), are a risk, particularly in longer procedures or during recovery.
Nerve Damage
The spinal cord and nerve roots are vulnerable during surgery, and accidental damage can lead to nerve impairment, which may cause weakness, numbness, or paralysis.
Implant Failure
In cases where metal rods, screws, or plates are used, there is a possibility that these devices may loosen, break, or shift over time, requiring further intervention.
Adjacent Segment Disease
As spinal fusion eliminates motion at the operated segment, the adjacent segments may experience increased stress, leading to degeneration and pain at the neighboring vertebrae.
Living with Spinal Column Reconstruction: Recovery and Quality of Life
The recovery period following spinal column reconstruction varies depending on the complexity of the surgery, the individual's overall health, and the level of the spine involved. Most patients can expect a recovery timeline of several months, during which physical therapy, rest, and gradual rehabilitation are necessary.
Post-Operative Care
-
Pain Management: Pain following surgery can be controlled with medications, but physical therapy and lifestyle changes play a significant role in long-term recovery.
-
Physical Therapy: Engaging in rehabilitation to strengthen back muscles, improve mobility, and prevent future injury is essential for full recovery.
-
Follow-Up Appointments: Regular check-ups are crucial to monitor the healing process, assess fusion progress, and detect any potential complications.
Lifestyle Changes
Patients who undergo spinal column reconstruction may experience permanent changes in their mobility, including reduced flexibility or difficulty with certain movements. Lifestyle modifications, such as regular exercise, weight management, and ergonomic adjustments at work, can help improve overall spinal health.
Long-Term Outlook
While spinal column reconstruction can significantly improve pain and restore function, it may not fully return the spine to its original state. Patients are encouraged to adopt a long-term management strategy that includes exercise, nutrition, and posture correction to protect the reconstructed spine and avoid future problems.
Top 10 Frequently Asked Questions about Spinal Column Reconstruction
1. What is Spinal Column Reconstruction, and why is it performed?
Spinal Column Reconstruction is a highly specialized surgical procedure designed to restore the stability, alignment, and structural integrity of the spine when it has been severely damaged. It is often performed in cases involving spinal fractures, advanced degenerative spine disease, tumor removal, spinal deformities, instability due to infections, or trauma that compromises the spine's ability to support the body. The goal of reconstruction is not only to stabilize the spine but also to relieve pressure on the spinal cord and nerves, correct deformities, restore normal posture, and prevent further neurological damage. This complex surgery may involve bone grafts, metal screws, rods, plates, cages, or artificial implants to rebuild damaged vertebrae and create a long-term support system for the spine.
2. What conditions commonly require Spinal Column Reconstruction?
Several severe spinal conditions may require reconstruction, especially when conservative measures fail. These include:
-
Traumatic spinal injuries such as fractures or dislocations.
-
Spinal tumors, either primary or metastatic, which can destroy bone structure.
-
Severe degenerative diseases like advanced osteoarthritis or degenerative disc disease.
-
Spinal deformities including scoliosis, kyphosis, or flat-back syndrome.
-
Spinal infections such as osteomyelitis or discitis that weaken vertebrae.
-
Failed previous spine surgeries or hardware failures.
Reconstruction is chosen when the spine becomes unstable, severely misaligned, or unable to support normal function.
3. How is Spinal Column Reconstruction performed? What does the surgery involve?
The procedure varies depending on the severity and cause of the spinal damage but generally includes several major steps:
-
Surgical access: The surgeon may approach the spine from the front (anterior), back (posterior), or both sides depending on the complexity.
-
Removal of damaged tissues: This may involve removing fractured bone, cancerous tissue, infected bone, or degenerative spinal segments.
-
Decompression: Pressure on the spinal cord and nerves is relieved by removing bone spurs, herniated discs, or tumor masses.
-
Reconstruction with implants: Titanium rods, screws, plates, cages, and sometimes expandable artificial vertebrae are used to restore shape and stability.
-
Bone grafting: Bone grafts (taken from the patient or donor bone) are used to encourage fusion and create a stable long-term support structure.
-
Fusion: Vertebrae are fused to ensure long-term stability and alignment.
The surgery may last several hours depending on the number of vertebrae being reconstructed and the degree of spinal instability.
4. What are the risks and complications associated with Spinal Column Reconstruction?
As a major, highly invasive spine surgery, reconstruction carries certain risks. Potential complications may include:
-
Bleeding and need for transfusion due to extensive surgical dissection.
-
Infection, especially when implants or large bone grafts are used.
-
Nerve or spinal cord injury, which could cause numbness, weakness, or paralysis.
-
Hardware complications, such as screw loosening, rod breakage, or graft failure.
-
Non-union (failed fusion), where bones do not fuse properly.
-
Blood clots, deep vein thrombosis, or pulmonary embolism.
-
Spinal fluid leaks and associated headaches.
-
Chronic pain or reduced spinal flexibility after surgery.
Although the risks are significant, the procedure is often necessary to prevent worsening disability or neurological decline.
5. How long is the recovery period after Spinal Column Reconstruction?
Recovery is lengthy and gradual. Most patients stay in the hospital for 5 to 10 days, depending on the surgical complexity and overall health. Initial recovery focuses on pain control, wound healing, and early mobilization with support from physical therapists.
-
First 6 weeks: Patients must avoid heavy lifting, bending, twisting, and strenuous activity.
-
3 months: Many patients resume light activities, depending on fusion progress.
-
6–12 months: Fusion continues to strengthen, and physical therapy improves mobility.
-
1 year: Most patients achieve maximum recovery, though improvements may continue beyond 12 months.
The exact timeline varies based on age, severity of damage, surgical technique, and individual healing ability.
6. Will Spinal Column Reconstruction relieve my pain?
Most patients experience significant relief from pain, especially when the pain was caused by nerve compression, spinal instability, or structural deformity. By decompressing nerves and stabilizing the spine, the surgery often reduces chronic pain that could not be managed with medication, physical therapy, or less invasive procedures. However, it is important to understand that while pain may improve greatly, some discomfort or stiffness may persist, particularly in cases involving extensive fusion or long-standing spinal damage. Pain relief is usually gradual and improves steadily as healing progresses.
7. How successful is Spinal Column Reconstruction, and what results can I realistically expect?
Success rates for spinal reconstruction surgeries are high when performed by experienced surgeons, especially in well-selected patients. Most individuals experience:
-
Dramatic improvement in spinal stability.
-
Reduction or elimination of nerve-related symptoms.
-
Better posture and overall body alignment.
-
Improved ability to perform daily activities.
-
Prevention of further spinal deformity or neurological decline.
However, patients should not expect complete restoration of flexibility, as fused segments will not bend. Success also depends on following rehabilitation plans and maintaining a healthy lifestyle post-surgery.
8. What is the role of physical therapy after Spinal Column Reconstruction?
Rehabilitation is a critical part of recovery. Physical therapy helps:
-
Restore muscle strength in the back, core, and legs.
-
Improve mobility and walking ability.
-
Reduce stiffness and prevent muscle imbalances.
-
Teach patients how to move safely without stressing the healing spine.
Therapy programs usually begin in the hospital and continue for several months afterward. Adhering to these routines significantly enhances overall surgical outcomes and long-term spinal health.
9. Are there lifestyle changes I need to make after undergoing spinal reconstruction?
Yes. Long-term spine health requires certain lifestyle modifications, including:
-
Avoiding smoking, as it drastically slows fusion and healing.
-
Maintaining a healthy weight to reduce stress on the reconstructed spine.
-
Practicing good posture to avoid unnecessary strain.
-
Avoiding heavy lifting, twisting, or high-impact activities even after healing.
-
Regular low-impact exercise such as swimming, yoga, or walking to strengthen back and core muscles.
Additionally, patients must attend regular follow-up appointments to ensure the spine is healing properly and that implants remain in position.
10. Who is a suitable candidate for Spinal Column Reconstructionsurgery?
Ideal candidates include individuals with severe spinal instability, deformity, or nerve compression that cannot be treated through conservative measures. These may include:
-
People with traumatic injuries causing fractures or instability.
-
Those with advanced scoliosis, kyphosis, or spinal collapse.
-
Patients with tumors requiring removal of part of the spine.
-
Individuals with chronic degenerative disease causing nerve compression and spinal weakness.
-
Patients who have had previous failed back surgeries.
Candidates must generally be in good overall health, able to undergo major surgery, and willing to commit to the long rehabilitation process that follows.


