Introduction to Spinal Cord Stimulation (SCS)
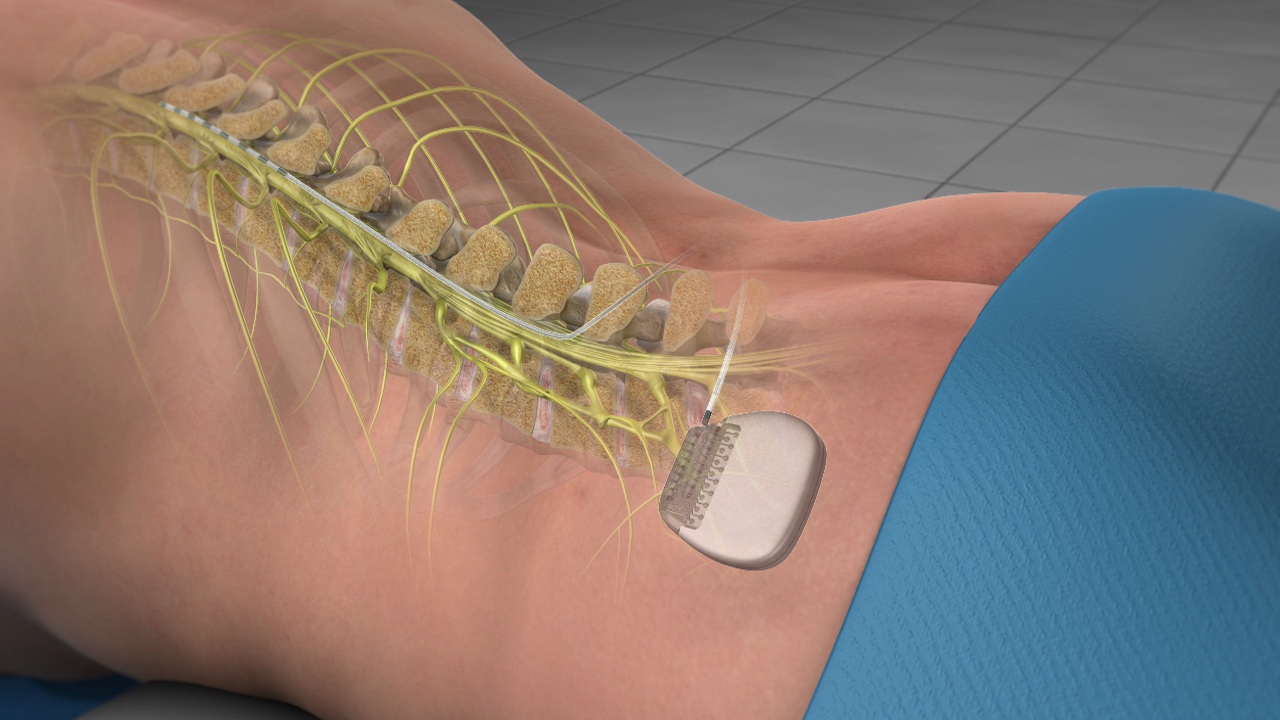
Spinal Cord Stimulation (SCS) is an advanced pain-management therapy used for patients with chronic, difficult-to-treat pain that has not responded to conventional medical or surgical treatments. It is a form of neuromodulation, which means it modifies pain signals traveling through the nervous system rather than directly "cutting" nerves or removing tissue. In SCS, a small, programmable device (similar to a cardiac pacemaker) delivers mild electrical impulses to the spinal cord or nearby nerve structures through thin wires called leads. These electrical pulses alter how pain signals are transmitted and perceived by the brain, thereby reducing the sensation of pain.
SCS is most commonly used for chronic neuropathic pain, such as pain after spine surgery (often called Failed Back Surgery Syndrome), complex regional pain syndrome (CRPS), painful diabetic neuropathy, radicular leg pain (sciatica-type symptoms), and certain types of nerve injury-related pain. Many patients who receive SCS have already tried medications, physical therapy, injections, and sometimes multiple surgeries with limited or temporary relief.
Modern spinal cord stimulators have evolved significantly. Earlier systems produced a tingling sensation called paresthesia that "overlapped" and masked the pain. Newer systems can work with or without paresthesia using different waveforms such as high-frequency stimulation, burst stimulation, and dorsal root ganglion (DRG) stimulation, providing more targeted and often more comfortable pain relief. Battery technology has also improved, with rechargeable and non-rechargeable options and devices that can last many years.
The SCS process typically involves a trial phase and, if successful, a permanent implantation. This stepwise approach allows both the patient and pain specialist to assess whether SCS provides meaningful pain relief and functional improvement before committing to a long-term implant. Overall, spinal cord stimulation is not a cure for the underlying disease, but for carefully selected patients it can significantly decrease pain, reduce reliance on pain medications (including opioids), and improve quality of life.
Causes and Risk Factors Related to Spinal Cord Stimulation (SCS)
Spinal Cord Stimulation itself is a treatment, not a disease. However, there are underlying causes and risk factors that lead to conditions where SCS becomes a recommended therapy, and there are also risks associated with the SCS procedure and device.
1. Causes and Conditions Leading to SCS
SCS is most often considered when chronic pain has persisted for months or years and other conservative or surgical treatments have failed. Common underlying causes include:
-
Failed Back Surgery Syndrome (FBSS)
Persistent or recurrent back and/or leg pain after one or more spine surgeries, often due to scar tissue, nerve damage, residual disc disease, or spinal instability. -
Radicular Pain and Neuropathic Leg Pain
Chronic nerve root compression or irritation from disc herniation, spinal stenosis, or degenerative spine disease causing burning, shooting, or electric-like pain down the arms or legs. -
Complex Regional Pain Syndrome (CRPS)
A chronic pain condition usually affecting an arm or leg after injury, surgery, or even minor trauma. It is characterized by severe burning pain, sensitivity to touch, color and temperature changes, and swelling. -
Peripheral Neuropathies
Conditions like painful diabetic neuropathy or nerve damage after trauma, surgery, or infection, especially when pain is localized to a specific region and refractory to medication. -
Ischemic Pain
In select cases, SCS may be used for chronic pain due to poor blood flow, such as refractory angina pectoris or peripheral vascular disease-related limb pain, when revascularization is not possible.
2. Risk Factors for Needing SCS
Risk factors that may lead to chronic pain requiring advanced treatments such as SCS include:
-
Multiple or complex spine surgeries
-
Long-standing degenerative spine disease or severe disc degeneration
-
Poorly controlled diabetes leading to neuropathy
-
High-impact trauma causing nerve injury
-
Smoking and sedentary lifestyle, which can worsen spine and vascular health
-
Psychological factors like anxiety, depression, and catastrophizing, which can amplify pain perception (these do not "cause" pain but can make pain more persistent and disabling)
3. Risks Associated with SCS Therapy Itself
While generally considered safe and reversible, SCS involves certain procedural and device-related risks:
-
Infection at the implant site
-
Bleeding or hematoma formation
-
Lead movement (migration) leading to loss of effectiveness
-
Hardware malfunction or breakage
-
Rare risk of nerve injury or spinal cord damage
-
Need for revision or removal surgery if complications arise or pain relief is inadequate
Understanding both the causes that lead to chronic pain and the risks of therapy helps patients make informed decisions about whether SCS is a suitable option for them.
Symptoms and Signs Indicating the Need for Spinal Cord Stimulation (SCS)
Because SCS is a treatment, the "symptoms and signs" relate to the pain condition and its impact on daily life. Patients who are candidates for SCS typically exhibit the following features:
1. Chronic, Refractory Pain
-
Pain lasting longer than 3-6 months despite appropriate treatment
-
Pain that persists after spine surgery, injections, or other interventions
-
Pain that is moderate to severe and significantly affects daily activities, sleep, work, or mood
2. Neuropathic Pain Characteristics
SCS works best for neuropathic pain, which may present as:
-
Burning, shooting, stabbing, or electric-shock-like sensations
-
Tingling, pins-and-needles, or "crawling" feelings
-
Hypersensitivity to touch or mild pressure (allodynia)
-
Pain disproportionate to the original injury
3. Regional and Well-Defined Pain Pattern
Ideal candidates often have pain that:
-
Is localized to a specific region such as back and legs, neck and arms, or a single limb
-
Follows a nerve distribution (radicular pattern) or is confined to one or two limbs
4. Functional Impairment and Reduced Quality of Life
Patients considering SCS commonly experience:
-
Difficulty walking, standing, or sitting for long periods
-
Limitations in working, household chores, or social activities
-
Sleep interruptions due to pain
-
Emotional distress, depression, or anxiety linked to chronic pain
5. Limited Response or Intolerance to Medications
Many candidates have:
-
Tried multiple pain medications (NSAIDs, neuropathic agents, opioids) with limited benefit
-
Experienced significant side effects (sedation, confusion, constipation, organ toxicity)
-
Desire to reduce reliance on long-term pain medication, especially opioids
When these symptoms persist despite optimal conventional care, a pain specialist may evaluate the patient for SCS as a next-level intervention.
Diagnosis and Evaluation Before Spinal Cord Stimulation (SCS)
Before recommending SCS, healthcare providers conduct a comprehensive evaluation to confirm the underlying diagnosis, assess the nature of pain, and determine if SCS is appropriate.
1. Clinical Assessment
-
Detailed History
Onset, duration, nature, and distribution of pain; prior surgeries; treatments tried; response to medications; impact on daily life. -
Physical and Neurological Examination
Muscle strength, reflexes, sensory changes, gait, spinal alignment, and range of motion. The aim is to identify areas of nerve dysfunction, spinal pathology, or muscle imbalance.
2. Imaging and Diagnostic Tests
-
MRI or CT Scans of the Spine
To evaluate disc herniations, stenosis, scar tissue, nerve root compression, spinal instability, or previous hardware. -
X-rays
To assess alignment, degenerative changes, and previous fusions or implants. -
Nerve Conduction Studies / EMG (if needed)
To evaluate the integrity and function of peripheral nerves and nerve roots.
3. Psychological / Behavioral Evaluation
Because chronic pain is influenced by emotional and psychological factors, many centers include:
-
Screening for depression, anxiety, substance misuse, or unmanaged psychological conditions
-
Evaluation of patient expectations, coping strategies, and support system
-
Identifying any factors that might reduce the success of SCS (e.g., untreated severe depression, unrealistic expectations)
4. Treatment History and Response Review
Doctors carefully review:
-
Which medications have been used and at what doses
-
Response to physical therapy, injections, nerve blocks, or prior surgeries
-
Whether the pain is predominantly neuropathic and regional, which predicts better response to SCS
5. SCS Trial as a Diagnostic-Therapeutic Step
A key part of "diagnosis" in SCS is the temporary trial:
-
Temporary leads are placed into the epidural space through a needle.
-
The external stimulator is programmed, and the patient goes home with it for a few days (typically 3-7 days).
-
The patient tracks pain relief, changes in activity levels, sleep quality, and medication use.
If the trial results in substantial pain reduction (commonly defined as ≥50% improvement) and better function, the patient is considered a good candidate for permanent implantation.
Treatment Options: Spinal Cord Stimulation (SCS) Procedure and Variations
Spinal cord stimulation (SCS) is a two-stage interventional pain therapy: a temporary trial followed by permanent implantation if the trial provides meaningful pain and function improvement. There are several procedural approaches and device/waveform variations that can be tailored to the pain condition, anatomy, and patient preference.
1. Non-Surgical Treatment Options Before SCS
Before proceeding to SCS, most patients will have tried:
-
Medications: NSAIDs, antidepressants, anticonvulsants, muscle relaxants, opioids
-
Physical and Occupational Therapy: stretching, strengthening, posture training
-
Interventional Procedures: epidural steroid injections, nerve blocks, radiofrequency ablation
-
Psychological Interventions: cognitive-behavioral therapy, pain coping strategies, stress management
SCS is usually considered when these options fail to provide adequate relief or when long-term medication use becomes problematic.
2. Components of an SCS System
A typical SCS system includes:
-
Leads (electrodes): Thin, flexible wires with multiple contact points placed in the epidural space near the spinal cord or dorsal root ganglion.
-
Implantable Pulse Generator (IPG): A small battery-powered device placed under the skin (usually abdomen or buttock) that generates electrical impulses.
-
Extension Cables (if used): Connect leads to the IPG.
-
External Programmer: A remote control used by the patient and clinician to adjust stimulation settings, intensity, and programs.
3. Types of Stimulation
Modern SCS systems offer different stimulation patterns:
-
Traditional (Tonic) Stimulation: Produces a tingling sensation (paresthesia) in the area of pain.
-
High-Frequency Stimulation: Delivers pulses at very high frequencies, often without perceivable tingling, yet providing pain relief.
-
Burst Stimulation: Delivers groups ("bursts") of pulses designed to more closely mimic natural neural firing patterns and may be comfortable with or without paresthesia.
-
Dorsal Root Ganglion (DRG) Stimulation: Targets specific nerve roots for highly localized pain (e.g., foot, knee, groin, CRPS areas).
4. The SCS Trial Procedure
-
Usually performed under local anesthesia with or without sedation.
-
Leads are inserted through a needle into the epidural space and positioned under X-ray guidance.
-
External cables connect leads to an external stimulator.
-
The patient goes home, uses the device, and records pain levels and activity changes.
5. Permanent SCS Implantation
If the trial is successful:
-
Surgical Implantation
-
The leads are repositioned or confirmed in the best location.
-
The IPG is implanted in a small pocket under the skin.
-
Leads are tunneled under the skin and connected to the IPG.
-
-
Programming and Adjustment
-
After wound healing, the SCS is carefully programmed to achieve optimal pain coverage.
-
Patients receive instructions on how to use the external controller to adjust settings within prescribed ranges.
-
-
Follow-Up Care
-
Regular follow-ups to evaluate pain relief, adjust programming, check battery level, and monitor for any complications.
-
SCS can be turned on and off and reprogrammed as needed, and if necessary, it can be revised or removed, making it a reversible form of pain management.
Prevention and Management in the Context of Spinal Cord Stimulation (SCS)
Prevention and management in spinal cord stimulation (SCS) focus on: choosing the right patient, minimizing perioperative complications (especially infection and hardware issues), and providing structured long-term follow-up and patient education. When these elements are in place, SCS can offer durable pain relief, functional gains, and reduced medication use for carefully selected patients.
1. Preventing Progression to Severe Chronic Pain
While not all chronic pain is preventable, certain measures can reduce the risk:
-
Early and Appropriate Treatment of acute back or limb injuries
-
Good Control of Underlying Diseases like diabetes, which can lead to neuropathy
-
Lifestyle Measures: maintaining healthy weight, regular physical activity, avoiding smoking, and using proper body mechanics at work and home
-
Ergonomic Adjustments at workplace to reduce repetitive strain or poor posture
2. Pre-Implant Preparation
For patients moving toward SCS:
-
Optimize Medical Conditions (diabetes, blood pressure, heart disease)
-
Stop Smoking, as it impairs wound healing and may worsen pain
-
Review Medications, including blood thinners, which may need adjustment around surgery
-
Set Realistic Expectations: SCS aims to reduce pain and improve function, not completely eliminate all pain.
3. Post-Implant Management
After SCS implantation, effective management includes:
-
Wound Care and Activity Restrictions: Avoid heavy lifting, bending, twisting in the first weeks; follow surgeon’s instructions for incision care.
-
Gradual Return to Activities: Under guidance, patients progressively increase walking and daily activities.
-
Regular Device Checks and Reprogramming: Fine-tuning the device can significantly improve pain relief and comfort over time.
-
Medication Review: As pain improves, doctors may reduce or adjust pain medications safely.
4. Long-Term Pain Self-Management
-
Maintain an active lifestyle within safe limits.
-
Continue physical therapy or home exercises to keep muscles strong and flexible.
-
Use psychological coping strategies like relaxation techniques, mindfulness, and cognitive restructuring to handle flare-ups.
-
Attend follow-up appointments and report any new symptoms (sudden change in stimulation, loss of effect, new pain, or signs of infection).
Complications of Spinal Cord Stimulation (SCS)
Although many patients benefit significantly from SCS, it is important to understand potential complications:
1. Surgical Complications
-
Infection at the IPG or lead site, sometimes requiring antibiotics or removal of the system.
-
Bleeding or Hematoma around the implant site or in the epidural space.
-
Dural Puncture and possible spinal fluid leak, which may cause headache and require specific treatment.
2. Hardware-Related Complications
-
Lead Migration: The leads may move from their original position, reducing coverage of the painful area and requiring reprogramming or surgical repositioning.
-
Lead Fracture or Hardware Failure: Rarely, wires or connectors may break over time.
-
Battery Depletion: Non-rechargeable batteries will eventually need replacement; rechargeable systems require regular charging.
3. Neurological Complications
-
Very rare but serious events include nerve damage or spinal cord injury leading to new neurological deficits.
-
Abnormal or uncomfortable sensations, jolts, or shocks if settings or lead positions are suboptimal.
4. Stimulation-Related Issues
-
Loss of Effect Over Time: In some patients, pain relief may diminish, possibly due to disease progression, tolerance, or changes in the nervous system.
-
Unpleasant Paresthesia: Some people may find tingling sensations annoying or uncomfortable if traditional stimulation is used.
-
Interference with Other Devices or Procedures: Limited MRI compatibility in some older devices; patients must always inform healthcare providers and security personnel (e.g., at airports) about their implant.
While these complications are concerning, careful patient selection, meticulous surgical technique, regular follow-up, and up-to-date technology reduce risks significantly.
Living with the Condition and Treatment of Spinal Cord Stimulation (SCS)
Living with SCS means living with both chronic pain and a long-term implanted device. Most patients are able to adapt well and often experience a significant improvement in function and comfort.
1. Daily Life and Activities
-
Many patients report being able to walk longer, stand more comfortably, and participate in previously limited activities.
-
Certain restrictions (heavy lifting, extreme twisting, high-impact sports) may remain, especially in the early months, but most routine daily activities are encouraged once healing is complete.
-
Patients can usually drive, work, and travel, but should follow specific advice from their doctor.
2. Device Management
-
Patients learn to use a handheld programmer to adjust stimulation within safe limits.
-
Those with rechargeable systems must regularly charge their IPG, which typically involves wearing an external belt or pad over the implant for a set period.
-
Battery status is monitored during regular follow-ups.
3. Emotional and Psychosocial Aspects
-
Chronic pain often causes frustration, anxiety, or depression. With improved pain relief, many patients experience better mood and outlook.
-
Some may still benefit from counseling, support groups, or psychological therapy to manage residual pain and emotional impact.
-
Patients should be encouraged to maintain strong social connections, engage in hobbies, and gradually rebuild confidence in their bodies.
4. Travel, Work, and Security Considerations
-
Most SCS systems are safe for flying and traveling, but patients should carry an implant identification card.
-
Airport and security scanners may detect the device; patients can inform security staff in advance.
-
Many jobs and professions remain possible, but work involving heavy physical labor may require special planning or role modification.
5. Long-Term Follow-Up
-
Regular follow-up visits with the pain specialist or neurosurgeon are essential to monitor device function, pain levels, and overall health.
-
Over time, adjustments in programming, medications, or lifestyle may be needed.
-
If pain patterns change (for example, pain moving to a new area), the system may need reprogramming or reassessment.
Top 10 Frequently Asked Questions about Spinal Cord Stimulation (SCS)
1. What is Spinal Cord Stimulation (SCS), and how does it work?
Spinal Cord Stimulation (SCS) is an advanced pain-management therapy that uses a small, implanted device to deliver mild electrical signals to the spinal cord. These electrical impulses modify pain signals before they reach the brain, reducing the sensation of pain. Instead of feeling sharp or chronic pain, patients often experience a tingling sensation, reduced discomfort, or in newer systems, no sensation at all while still achieving pain relief. SCS is typically recommended for people with chronic back, leg, or nerve-related pain, especially when other treatments such as medications, injections, or physical therapy have failed. The goal is not to remove the cause of pain but to manage and reduce pain sufficiently, enabling better daily function, mobility, and quality of life.
2. Who is a suitable candidate for Spinal Cord Stimulation?
Ideal candidates for SCS are individuals suffering from chronic, intractable pain that has persisted for more than six months and has not responded adequately to conservative treatments. Conditions that benefit from SCS include Failed Back Surgery Syndrome, Complex Regional Pain Syndrome (CRPS), chronic radiculopathy, neuropathic pain, spinal stenosis, and nerve damage resulting from injuries or prior surgery. Suitable candidates are those who are medically stable, have realistic expectations regarding outcomes, and are willing to participate in both the trial phase and follow-up adjustments. SCS is not suitable for individuals with severe psychiatric illnesses, untreated infections, bleeding disorders, or those unable to comply with post-implantation care and lifestyle recommendations.
3. What types of Spinal Cord Stimulators are available?
There are multiple types of SCS systems, each offering different benefits:
-
Traditional (Tonic) SCS: Produces a mild tingling sensation (paresthesia) that replaces pain signals.
-
Burst SCS: Sends intermittent pulses to mimic natural nerve firing, often reducing pain without noticeable tingling.
-
High-Frequency SCS: Delivers rapid pulses at higher frequencies, providing pain relief without paresthesia and often better coverage for back pain.
-
Adaptive/Closed-Loop SCS: Adjusts stimulation levels automatically in real-time based on spinal movement, maintaining consistent pain relief throughout the day.
-
Rechargeable vs. Non-Rechargeable Systems: Some devices require periodic charging, while others are simpler, with batteries lasting several years before replacement.
The choice depends on the patient's pain type, lifestyle, body structure, and desired level of control.
4. How is the Spinal Cord Stimulation procedure performed?
SCS implantation typically happens in two stages:
1. Trial Phase:
A temporary stimulator lead is placed through a needle into the epidural space near the spinal cord. It is connected to an external battery pack worn outside the body. This trial lasts several days to a week, allowing the patient to test whether SCS provides meaningful pain relief—generally defined as at least 50% reduction in pain.
If the trial is successful, a permanent system is implanted. The surgeon makes small incisions to insert the stimulation leads and place the battery (pulse generator) under the skin, usually in the upper buttock or abdomen. The entire system is internalized, and patients can control the stimulation using a handheld remote or mobile app, depending on the model. The procedure usually takes 1-2 hours and is minimally invasive compared to open spinal surgeries.
5. What conditions can Spinal Cord Stimulation successfully treat?
SCS is highly effective for managing chronic neuropathic and spine-related pain conditions, including:
-
Failed Back Surgery Syndrome (FBSS)
-
Chronic low-back and leg pain
-
Sciatica and nerve root compression pain
-
Complex Regional Pain Syndrome (CRPS)
-
Peripheral neuropathy
-
Post-surgical nerve pain
-
Spinal stenosis-related pain
-
Pain after herniated disc surgery
-
Ischemic pain (in selected cases)
Although SCS does not cure these underlying conditions, it allows patients to return to daily activities, reduce reliance on pain medications, and in some cases, resume work or physical activity.
6. What are the risks and complications associated with SCS?
Like any surgical procedure or implantable device, SCS carries potential risks. Common complications include:
-
Infection at the site of implantation.
-
Device migration, where leads shift position and reduce effectiveness.
-
Hardware issues such as battery or lead malfunction.
-
Pain at the implant site, usually temporary.
-
Nerve damage, though rare, may occur during lead placement.
-
Scar tissue formation, which can interfere with stimulation.
-
Allergic reactions to device materials.
-
Loss of therapeutic effect over time if the pain condition progresses or the device position changes.
Most risks are manageable and minimized when the surgery is performed by an experienced spine or pain specialist.
7. What is recovery like after SCS surgery?
Recovery from SCS implantation is generally quicker than traditional spine surgery. Most patients can go home the same day or within 24 hours. During the first few weeks, patients are advised to:
-
Avoid bending, twisting, or heavy lifting.
-
Avoid raising arms above shoulder level.
-
Keep the incision area clean and dry.
-
Walk regularly to maintain circulation and mobility.
Mild discomfort or swelling at the incision site is normal and usually resolves within days. Over the next 6-8 weeks, as scar tissue forms around the leads, patients gradually resume daily activities. Full recovery and stabilization of stimulation settings may take up to three months, during which the device may be fine-tuned based on feedback.
8. How effective is Spinal Cord Stimulation for long-term pain relief?
SCS is considered highly effective for many chronic pain conditions. Studies have shown that 60-80% of patients experience significant, long-lasting pain relief. Many patients reduce or discontinue opioid-based medications after implantation. The effectiveness often depends on correct patient selection, device programming, and addressing any underlying issues that contribute to chronic pain. While SCS does not cure the root cause of pain, it allows individuals to regain mobility, improve sleep quality, and engage in daily activities with greater comfort.
9. Will I feel the stimulation, and can I control the device?
This depends on the type of stimulator used.
-
Traditional SCS produces a tingling or buzzing sensation that replaces pain.
-
Burst and high-frequency SCS typically provide pain relief without sensations and are often preferred by patients who find paresthesia distracting.
Patients can adjust stimulation intensity, switch between programs, or turn the system on/off using a small remote control or smartphone-connected controller. The device can be customized based on posture, activity level, and daily routine. Advanced "smart" systems even adjust the stimulation automatically.
10. How long does the Spinal Cord Stimulator last, and what happens afterward?
The lifespan of an SCS system depends on the type of battery used:
-
Rechargeable batteries can last 10-15 years with regular charging.
-
Non-rechargeable batteries last 3-7 years and require surgical replacement once depleted.
The leads (wires) and electrodes often last much longer unless they malfunction or shift position. Follow-up appointments are essential to monitor device performance, check battery health, adjust settings, and ensure continued pain relief. Replacement surgeries for battery changes are typically minor and much simpler than the initial implantation.


