Introduction to Spine Surgery
Spine surgery is a specialized branch of orthopaedic and neurosurgery that focuses on correcting structural problems of the vertebral column when they cause significant pain, deformity, neurological deficit, or loss of function. The spine is a highly complex pillar made up of vertebrae, intervertebral discs, facet joints, ligaments, muscles, and the delicate spinal cord and nerve roots travelling through the spinal canal. When this finely tuned structure is damaged by degeneration, trauma, tumors, infections, or congenital deformities, patients may develop severe back or neck pain, radiating limb pain, weakness, numbness, impaired balance, and even bowel or bladder problems. Most spinal conditions can initially be treated with non-surgical options such as medications, physiotherapy, lifestyle modification, injections, and bracing. However, when these measures fail, or when the problem is advanced or rapidly worsening, spine surgery becomes an important option to decompress nerves, stabilize the spine, and restore alignment.
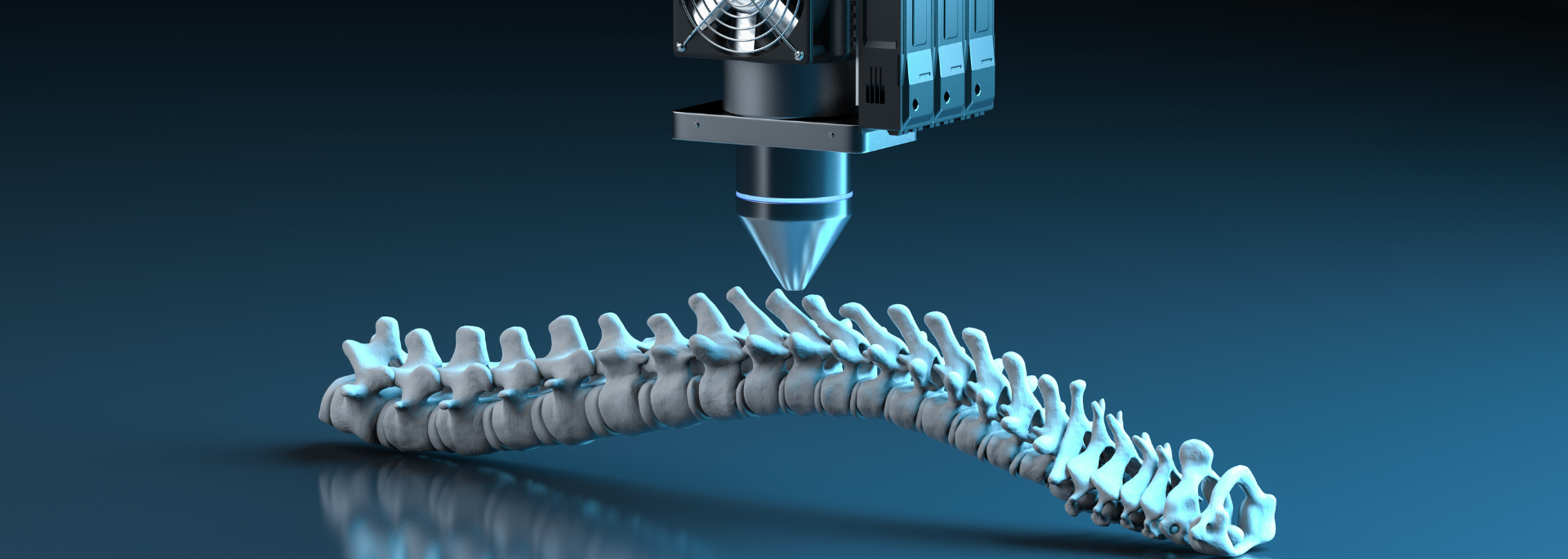
Spine surgery is not one single procedure but a spectrum of operations that range from small, minimally invasive decompressions and discectomies to complex reconstructive deformity surgeries and spinal osteotomies, where parts of the vertebra are cut and reshaped to correct severe curvature and imbalance. Modern spine surgery aims not only to relieve pain but also to achieve spinal balance, protect the nervous system, and improve quality of life. With advances in imaging, anaesthesia, intra-operative neuromonitoring, computer navigation, robotics, and improved implants, outcomes have improved significantly, especially when patients are carefully selected and surgery is performed in experienced centres.
Causes and Risk of Spine Surgery
Spine surgery is usually a last-line or advanced treatment, chosen when the underlying cause of spinal disease is severe, progressive, or refractory to conservative care. Understanding the conditions that commonly lead to surgery and the risk factors that predispose to them is essential.
2.1 Common Conditions Leading to Spine Surgery
-
Degenerative Disc Disease and Spondylosis
With age or repetitive strain, the intervertebral discs lose water and height, and the facet joints and surrounding ligaments undergo arthritic changes. This can cause chronic back or neck pain, stiffness, and sometimes instability or spinal canal narrowing (stenosis). In advanced cases with persistent symptoms or neurological compromise, decompression and fusion may be required. -
Disc Herniation (Slipped Disc)
The soft center of the disc can protrude or rupture through the outer ring, compressing nearby nerve roots. This classically causes sciatica (radiating leg pain) or arm pain, numbness, and weakness. When severe or persistent despite non-surgical therapy, surgery such as microdiscectomy or discectomy with fusion may be indicated. -
Spinal Stenosis
Degenerative overgrowth of bone and ligaments, disc bulges, and joint enlargement can narrow the spinal canal and foramina, compressing nerve roots. Patients often develop leg pain and heaviness while walking (neurogenic claudication), relieved by sitting or bending forward. Persistent disability or progressive neurological deficit may require decompressive surgery, sometimes with fusion if there is instability. -
Spinal Deformities (Scoliosis, Kyphosis, Flatback)
Curvatures of the spine may be present from adolescence or develop later due to degeneration, fractures, or previous surgery. Severe, rigid deformities that cause cosmetic concern, pain, imbalance, or breathing difficulty can require complex reconstruction with spinal osteotomies and long-segment fusion. -
Trauma and Fractures
High-energy injuries (falls, road accidents) or osteoporotic fractures may collapse or displace vertebrae, compressing the spinal cord or nerves and causing instability. Surgical fixation with screws, rods, cages, and sometimes vertebral reconstruction may be necessary to protect the nervous system and allow early mobilization. -
Tumors and Infections
Primary or metastatic tumours and spinal infections (osteomyelitis, discitis, epidural abscess) can destroy bone, deform the spine, and compress neural structures. Surgical goals include decompression, tumour or infected tissue removal, and reconstruction of the spinal column. -
Failed Back / Persistent Spinal Pain After Surgery
Some patients continue to have significant pain even after prior spine surgery due to scarring, residual compression, instability, or adjacent-segment disease. These cases may require revision surgery or more extensive reconstruction.
2.2 Risk Factors for Needing Spine Surgery
-
Increasing age and long-standing mechanical wear and tear
-
Sedentary lifestyle, poor core strength, and deconditioning
-
Obesity and heavy manual labour
-
Smoking (impairs bone quality and healing)
-
Osteoporosis or osteopenia
-
Congenital spinal deformities or connective tissue disorders
-
Systemic diseases such as rheumatoid arthritis, malignancy, or chronic infections
These factors do not guarantee that surgery will be required but make serious spinal problems more likely.
Symptoms and Signs of Spine Conditions that May Require Surgery
Spine surgery is generally considered when symptoms are severe, persistent, or progressive, and clearly linked to structural abnormalities seen on imaging.
3.1 Pain Symptoms
-
Chronic back or neck pain that lasts for months, interferes with sleep, work, and daily activities, and fails to respond adequately to medications, physiotherapy, and injections.
-
Radicular pain - sharp, burning, or electric-shock-like pain radiating along a nerve path into the arm (cervical radiculopathy) or leg (sciatica).
-
Claudication-type pain - leg pain, heaviness, cramping, or weakness on walking or standing, relieved by sitting or bending forward, typical of spinal stenosis.
3.2 Neurological Signs
-
Numbness or tingling in hands, arms, legs, or feet.
-
Weakness - difficulty lifting the foot (foot drop), gripping objects, or climbing stairs.
-
Loss of fine motor control - clumsy hands, dropping items, difficulty fastening buttons (often due to cervical myelopathy).
-
Reflex changes on examination.
Red-flag neurological signs include:
-
Loss of bladder or bowel control, saddle anaesthesia, and severe leg symptoms suggesting cauda equina syndrome - a true emergency needing urgent decompression.
3.3 Deformity and Balance
-
Visible curvature of the spine, uneven shoulders or hips, prominent rib hump, or forward stooping.
-
Difficulty standing upright, tendency to lean forward, or feeling “off balance” when walking.
-
Progressive height loss.
3.4 Functional Impairment
-
Inability to walk reasonable distances without pain or weakness.
-
Dependence on strong painkillers, affecting alertness and quality of life.
-
Inability to work or perform basic daily activities.
When these symptoms and signs correlate with imaging findings and fail to improve after a structured course of conservative care, surgery is considered.
Diagnosis of Spine Conditions Before Surgery
Accurate diagnosis and detailed planning are critical to safe and effective spine surgery.
4.1 Clinical Assessment
-
History - onset, duration, nature, and distribution of pain; aggravating and relieving factors; prior injuries or surgeries; impact on daily life and work.
-
Physical Examination - posture, spinal range of motion, muscle strength, reflexes, sensory changes, gait and balance.
-
Assessment of General Health - cardiac, respiratory, metabolic status, medications, and risk factors for anaesthesia and healing.
4.2 Imaging
-
X-Rays
-
Show bony alignment, curvature, disc height, spondylolisthesis, and overall spinal balance.
-
Standing full-length films are crucial in deformity surgery planning to assess sagittal and coronal balance.
-
-
MRI (Magnetic Resonance Imaging)
-
Visualizes discs, spinal cord, nerve roots, ligaments, and soft tissues.
-
Essential for evaluating disc herniations, spinal stenosis, infections, and tumours.
-
-
CT (Computed Tomography)
-
Provides detailed images of bone; valuable in trauma, revision surgery, assessing fusion, and planning osteotomies and instrumentation.
-
-
CT Myelography (select cases)
-
Combines contrast dye with CT when MRI is contraindicated or inconclusive.
-
4.3 Additional Tests
-
Nerve Conduction Studies / EMG - help distinguish spinal from peripheral nerve problems.
-
Bone Density (DEXA) - especially important in older adults and deformity surgery to gauge osteoporosis and risk of hardware failure.
-
Blood Tests - infection markers, metabolic profile, vitamin D and calcium for bone health.
4.4 Pre-Operative Planning (Especially for Spinal Osteotomies)
For complex deformity corrections:
-
Detailed measurement of curves, pelvic incidence, lumbar lordosis, and global sagittal balance.
-
Selection of appropriate osteotomy level and type (Smith-Petersen osteotomy, pedicle subtraction osteotomy, vertebral column resection) depending on rigidity and magnitude of deformity.
-
Use of 3D planning, navigation, or templates in complex cases.
-
Pre-operative neuromonitoring strategy and blood management plan.
Treatment Options of Spine Surgery
Spine surgery includes a wide range of operative strategies tailored to the underlying pathology, patient's symptoms, and general health.
5.1 Decompression Procedures
These operations relieve pressure on the spinal cord and nerves:
-
Laminectomy or Laminotomy - removal of part/all of the vertebral arch to widen the spinal canal, commonly used for spinal stenosis.
-
Foraminotomy - enlargement of the nerve root canal to relieve compression by bone spurs or disc material.
-
Discectomy / Microdiscectomy - removal of herniated disc fragments compressing a nerve, often via small incisions and microscopic assistance.
5.2 Stabilization and Fusion
Fusion surgery stops abnormal motion between vertebrae and restores stability:
-
Posterior Fusion - screws and rods placed from the back; bone grafts encourage fusion.
-
Anterior / Lateral Fusion - cages or grafts placed from the front or side to restore disc height and correct alignment.
-
Interbody Fusion Techniques - PLIF, TLIF, ALIF, LLIF, depending on approach. Fusion is particularly used in instability, deformity, and advanced degeneration, though indications must be carefully weighed to avoid overuse.
5.3 Motion-Preserving Procedures
In selected patients:
-
Total Disc Replacement (Arthroplasty) - replacement of a degenerated disc with an artificial one, preserving motion and possibly reducing adjacent-segment stress.
5.4 Spinal Osteotomies and Deformity Reconstruction
Spinal osteotomies are powerful tools for correcting fixed, rigid deformities:
-
Smith-Petersen Osteotomy (SPO) / Ponte Osteotomy - posterior column osteotomy achieved by removing facets and posterior ligaments, allowing controlled closing of the posterior column and opening of the anterior disc space; gives about 10° of correction per level and is useful for smooth kyphosis correction.
-
Pedicle Subtraction Osteotomy (PSO) - removal of a wedge of bone from the posterior elements and vertebral body through a posterior approach, allowing about 30° of segmental correction; used for severe, rigid sagittal imbalance.
-
Vertebral Column Resection (VCR) - removal of an entire vertebral segment for extreme deformities, allowing dramatic correction in both sagittal and coronal planes but with higher risk; reserved for very severe, complex cases.
These procedures are typically combined with long-segment instrumentation and fusion to maintain the correction.
5.5 Minimally Invasive Spine Surgery (MISS)
For selected patients and pathologies:
-
Uses small incisions, tubular retractors, and endoscopic or microscopic visualization.
-
Can be applied to discectomy, decompression, and some fusion procedures.
-
Offers potential benefits like reduced muscle damage, less blood loss, shorter hospital stay, and faster early recovery, although it may not be suitable for very complex deformities.
Prevention and Management of Spine Conditions Around Surgery
6.1 Preventing or Delaying Spine Problems
While not all spine diseases can be avoided, many risk factors can be modified:
-
Maintain ideal body weight to reduce mechanical load on the spine.
-
Regular exercise and core strengthening to support spinal structures.
-
Ergonomics at work and home (correct sitting posture, proper lifting techniques, avoiding prolonged bending or twisting).
-
Avoid smoking and excessive alcohol, which impair bone quality and healing.
-
Bone health management - adequate calcium and vitamin D, treatment of osteoporosis where necessary.
6.2 Pre-Operative Management
Before surgery:
-
Optimize control of chronic conditions (diabetes, hypertension, heart disease).
-
Encourage smoking cessation and weight loss where possible.
-
Pre-operative physiotherapy (“pre-hab”) to build strength and respiratory capacity.
-
Detailed explanation of the procedure, benefits, risks, and realistic expectations to improve cooperation and satisfaction.
6.3 Post-Operative Management and Rehabilitation
After spine surgery:
-
Pain control with carefully managed medications.
-
Early mobilization - sitting, standing, and walking as soon as permitted to reduce risk of blood clots and lung complications.
-
Physiotherapy - progressive exercises to restore strength, flexibility, and balance; gait training and posture correction.
-
Bracing in selected patients to support the spine during early healing.
-
Regular wound checks to detect any signs of infection or healing problems early.
6.4 Long-Term Management
-
Ongoing exercise and weight control to maintain results and protect adjacent segments.
-
Avoidance of heavy repetitive lifting and high-impact sports, especially after fusion or osteotomies.
-
Periodic follow-up and imaging to monitor fusion, hardware, and spinal alignment.
Complications of Spine Surgery
Spine surgery, particularly large deformity corrections and spinal osteotomies, carries important risks which must be clearly discussed.
7.1 General Surgical Risks
-
Infection at the surgical site
-
Excessive bleeding or need for transfusion
-
Blood clots (deep vein thrombosis, pulmonary embolism)
-
Anaesthetic complications
7.2 Spine-Specific Complications
-
Dural Tear and Cerebrospinal Fluid (CSF) Leak - may cause headaches and require repair or special post-operative positioning.
-
Nerve Root or Spinal Cord Injury - can result in new weakness, numbness, or, rarely, paralysis; neuromonitoring during complex osteotomies helps reduce this risk.
-
Residual or Recurrent Symptoms - pain or neurological symptoms may not completely resolve, or may recur with time.
7.3 Fusion and Hardware Complications
-
Non-union (Pseudoarthrosis) - failure of vertebrae to fuse, leading to persistent pain or instability; may require revision surgery.
-
Hardware Loosening or Breakage - screws or rods may loosen, especially in osteoporotic bone, or break if fusion is incomplete.
-
Adjacent Segment Disease - increased stress on levels above and below a fusion can lead to accelerated degeneration and new symptoms over time.
7.4 Specific Risks of Spinal Osteotomies
-
Greater blood loss and longer operative time.
-
Higher risk of neurologic deficit due to large angular corrections.
-
Need for intensive post-operative monitoring and prolonged rehabilitation.
Despite these potential complications, in carefully selected patients the benefits—pain relief, deformity correction, improved function and posture—often outweigh the risks.
Living with the Condition After Spine Surgery
Spine surgery is not the end of the story; it is the starting point of a new phase in how the patient lives with their spine condition.
8.1 Early Recovery
-
Focus on pain control, safe movements, and wound care.
-
Gradual increase in walking and light activities under guidance.
-
Avoid bending, twisting, and lifting heavy objects during the early weeks.
8.2 Medium-Term Recovery
-
Participation in structured physiotherapy to rebuild strength, flexibility, and endurance.
-
Return to office-type work often occurs within weeks to a few months (depending on procedure and individual recovery), while heavy labour may require a longer break or permanent modification.
8.3 Long-Term Lifestyle
-
Some loss of spinal flexibility is expected after fusion or osteotomies, particularly when multiple levels are involved, but this is often compensated by improved alignment and reduced pain.
-
Patients are encouraged to maintain an active lifestyle with low-impact exercises like walking, swimming, or cycling, and regular core strengthening to support the spine.
-
Long-term avoidance of smoking and maintenance of healthy body weight are critical for protecting bone and implant integrity.
8.4 Psychological and Social Adaptation
-
Chronic pain and disability before surgery can affect mood, relationships, and confidence. Surgical improvement often enhances emotional well-being, but residual symptoms or lifestyle changes may still require adjustment.
-
Some patients benefit from psychological support or pain management programmes to develop coping strategies and manage expectations.
-
Family support and clear communication with the healthcare team are important for a smooth transition back to normal life.
8.5 Follow-Up and Lifelong Spine Care
-
Regular follow-up visits and periodic imaging help detect hardware or alignment issues early.
-
New or progressive symptoms—such as worsening pain, new numbness, or weakness—should always be reported promptly.
-
Patients must understand that even after successful surgery, lifelong spine care—through healthy habits, exercise, and ergonomics—is essential.
Top 10 Frequently Asked Questions about Spine Surgery
1. What is spine surgery, and why is it performed?
Spine surgery is a specialized surgical approach used to treat various conditions that affect the vertebrae, spinal cord, nerves, and surrounding structures. It is performed when conservative treatments such as medications, physical therapy, injections, or lifestyle modifications fail to relieve symptoms. Spine surgery aims to stabilize the spine, decompress nerves, correct deformities, restore alignment, and improve mobility or quality of life. In advanced cases such as spinal deformities, fractures, tumors, instability, or severe stenosis, spine surgery becomes essential to prevent neurological decline and restore structural balance.
2. What are spinal osteotomies, and when are they necessary?
A spinal osteotomy is a complex spine surgery in which controlled cuts are made in the vertebrae to correct severe spinal deformities. These procedures are often used to treat conditions like kyphosis, flat-back syndrome, ankylosing spondylitis, post-traumatic deformity, and fixed sagittal imbalance. Osteotomies allow the surgeon to reshape or remove segments of bone to restore proper alignment. They are generally reserved for cases where the spinal curve is rigid, advanced, or unresponsive to less invasive correction methods.
3. What are the common types of spine surgeries performed?
Spine surgery includes a wide range of procedures based on the underlying condition:
-
Spinal decompression surgeries (e.g., laminectomy, discectomy) to relieve pressure on nerves.
-
Spinal fusion to stabilize unstable segments by joining vertebrae.
-
Spinal osteotomies (e.g., Smith-Petersen Osteotomy, Pedicle Subtraction Osteotomy) for major deformity correction.
-
Minimally invasive spine surgery to treat small herniated discs or stenosis.
-
Disc replacement surgery using artificial discs for mobility preservation.
-
Tumor resection surgery for spinal cancers or metastatic lesions.
-
Fracture stabilization using screws, rods, or cages after trauma.
Each procedure is tailored to the severity, location, and nature of the spinal condition.
4. Why might a patient require spine surgery instead of non-surgical treatments?
Spine surgery is recommended when chronic pain, nerve compression, spinal instability, or deformity significantly affects daily life and does not respond to conservative treatments. Surgery becomes essential if:
-
The spinal curve continues to worsen.
-
There is nerve damage causing numbness, weakness, or loss of function.
-
There is structural collapse from infections, tumors, or degeneration.
-
Pain is severe, persistent, and limiting quality of life.
In deformity cases like scoliosis or kyphosis, surgery is often the only way to restore proper alignment and prevent spinal cord compromise.
5. What are the risks and complications associated with spine surgery?
Spine surgery—especially complex procedures like spinal osteotomies—carries certain risks. Potential complications include:
-
Bleeding or need for transfusion
-
Infection at the surgical site
-
Nerve or spinal cord injury, causing weakness or sensory loss
-
Hardware failure, including broken screws or rods
-
Pseudoarthrosis (failed fusion)
-
Blood clots in legs or lungs
-
Spinal fluid leaks and associated headaches
-
Chronic pain or mobility limitations
Though risks exist, advances in surgical techniques and imaging guidance have significantly improved overall safety and outcomes.
6. How long is the recovery period after spine surgery?
Recovery varies greatly depending on the complexity of the procedure:
-
Minimally invasive surgeries: 4-6 weeks for most activities
-
Standard spinal fusion: 3-6 months for stabilization, up to one year for complete fusion
-
Major spinal osteotomies: 6-12 months for full recovery
During recovery, patients gradually regain mobility, strength, and confidence through rehabilitation. Avoiding strenuous activities, following posture guidelines, and adhering to prescribed medications are essential for proper healing.
7. Will spine surgery relieve my pain completely?
Many patients experience significant relief from chronic pain after spine surgery, especially when nerve compression, deformity, or instability is corrected. However, complete pain elimination is not always guaranteed. Relief varies depending on the severity of the condition, the presence of nerve damage before surgery, overall health, and adherence to postoperative care. Pain gradually decreases as healing progresses, and most patients are able to resume daily activities with greatly improved comfort and mobility.
8. What role does physical therapy play after spine surgery?
Physical therapy is essential to recovery after spine surgery. It helps patients:
-
Strengthen the muscles supporting the spine
-
Improve posture and body alignment
-
Restore flexibility and mobility
-
Reduce stiffness and muscle weakness
-
Learn safe techniques for walking, sitting, lifting, and bending
Rehabilitation typically begins a few days after surgery and continues for several months. A structured therapy program significantly enhances long-term outcomes and spine stability.
9. What lifestyle changes are recommended after spine surgery?
Patients are encouraged to adopt long-term lifestyle habits that support spine health, such as:
-
Maintaining a healthy weight to reduce pressure on the spine
-
Avoiding smoking, which impairs bone healing and increases fusion failure
-
Practicing good posture in daily activities
-
Engaging in low-impact exercises like walking, swimming, or yoga
-
Avoiding heavy lifting, twisting, or sudden movements that stress the spine
These changes help protect surgical outcomes and prevent future spine issues.
10. How successful is spine surgery, and what results should I expect?
Success rates for spine surgery are high when performed by skilled surgeons on well-selected patients. Many individuals experience:
-
Improved alignment and posture
-
Significant reduction in pain
-
Enhanced ability to stand, walk, or sit for longer durations
-
Correction of deformity (often dramatic in osteotomy patients)
-
Better quality of life and ability to return to normal activities
While fused parts of the spine will lose flexibility, overall function usually improves. Managing expectations and following postoperative guidelines are key to achieving the best outcome.


