Introduction to Splenectomy
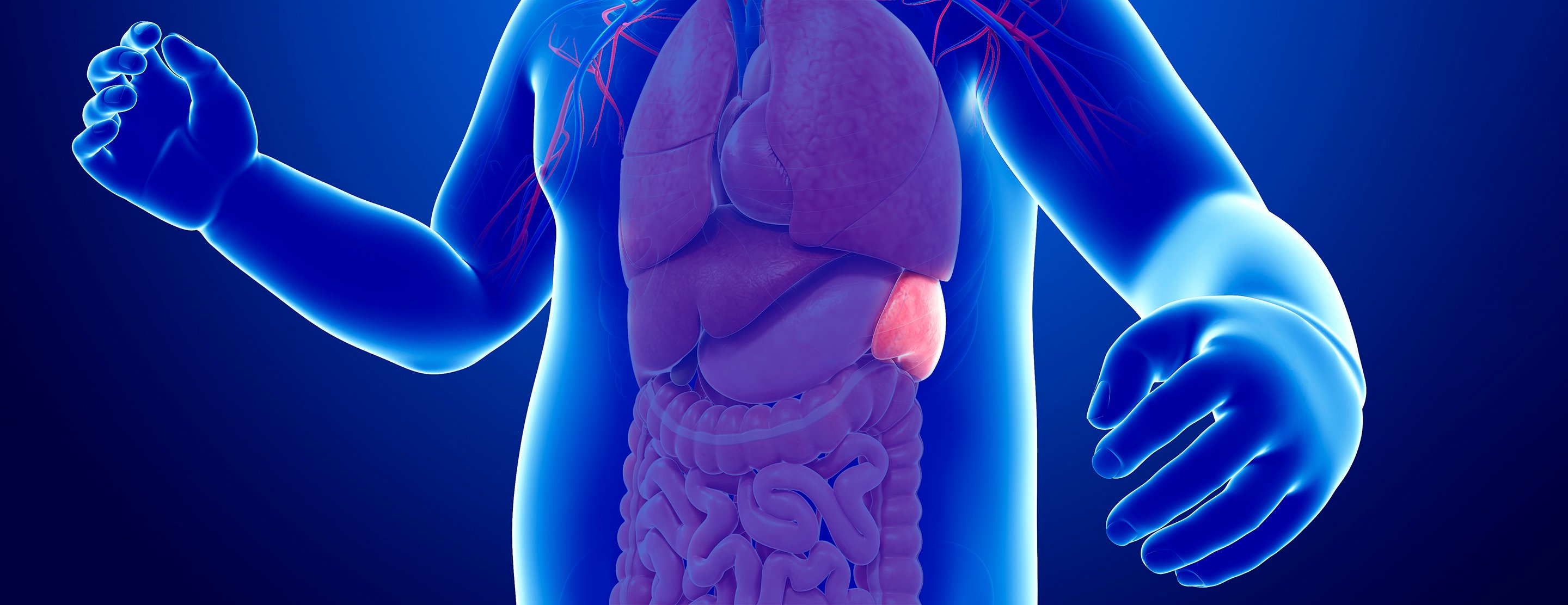
The spleen is a small but vital organ located beneath the left ribs, playing a critical role in filtering blood, removing old or damaged blood cells, storing platelets and red blood cells, and contributing to immune defense by helping destroy bacteria and other pathogens. While many of the spleen's functions can be taken over by other organs (like the liver and bone marrow), there are circumstances when the spleen itself becomes diseased, enlarged, injured or dysfunctional - necessitating its removal. This surgical procedure to remove the spleen, either partially or completely, is known as splenectomy.
Splenectomy may be lifesaving (for example, after trauma or rupture), or a therapeutic necessity (for certain blood disorders, tumors, or hypersplenism). With modern surgical techniques - especially minimally invasive (laparoscopic) approaches - splenectomy has become safer, and recovery times shorter, than older open-surgery methods. Nonetheless, removing the spleen permanently alters the body's immune and blood-filtering dynamics, and requires lifelong awareness, preventive care, and sometimes lifestyle adjustments.
In this guide, we'll explore what prompts a splenectomy, how it's diagnosed and performed, what patients should expect during recovery, and how to live healthily after spleen removal.
Causes and Risk Factors for Splenectomy
There are several broad categories of conditions and risks that may lead to the need for a splenectomy. Some of the most common include:
-
Traumatic Injury / Rupture: A blow to the abdomen - from accidents, falls, or sports injuries - may cause spleen rupture or severe internal bleeding. In many such cases, prompt splenectomy is life-saving.
-
Enlarged Spleen (Splenomegaly) & Hypersplenism: Diseases, infections, liver disorders, blood disorders, or chronic conditions can cause the spleen to enlarge and become overactive - destroying excessive blood cells (red blood cells, platelets, white blood cells). When this overactivity causes symptoms such as anemia, low platelet counts, or significant discomfort/fullness in the abdomen, removal may be indicated.
-
Blood Disorders: Certain hematologic conditions - for example hereditary hemolytic anemias, immune-mediated cytopenias (where the spleen destroys blood cells), some chronic leukemias or lymphomas - may not respond adequately to medical therapy. In such cases, splenectomy can help improve blood counts and reduce disease symptoms.
-
Splenic Tumors, Cysts, Abscesses or Other Splenic Diseases: Benign or malignant tumors of the spleen; cysts or abscesses; other focal diseases may make removal of the spleen the safest or only viable option.
-
Failed Conservative/Medical Treatment of Splenic Conditions: When medications or non-surgical treatments do not control hypersplenism, blood disorders, or splenic enlargement - and symptoms persist or worsen.
In deciding for splenectomy, medical teams consider not only the underlying disease or injury, but also the patient's overall health, immune status, ability to tolerate surgery, and long-term risks - since removal of the spleen carries implications for infection risk, blood/platelet dynamics, and more.
Symptoms and Signs That May Indicate Need for Splenectomy
Because the spleen lies deep within the abdomen, some problems only become evident once significant enlargement or dysfunction occurs. Common signs and symptoms that may lead to consideration of spleen removal include:
-
Pain or tenderness in the upper left side of the abdomen, often under the ribs; this may radiate to the left shoulder or upper back - especially when the spleen is enlarged or in cases of rupture/bleeding.
-
A sense of fullness or early satiety (feeling full quickly) after eating - an enlarged spleen may press on the stomach, reducing capacity.
-
Unexplained fatigue, pallor or jaundice, along with low red blood cell or platelet counts - indicating excessive destruction of blood cells (hemolysis or hypersplenism).
-
Frequent infections or poor immunity, recurrent infections, or unusual severity of infections - which may suggest splenic dysfunction or risk of rupture.
-
Bleeding tendencies or easy bruising, due to destruction of platelets or abnormal blood cell dynamics in conditions like hypersplenism.
-
Blood disorders symptoms - such as those seen in congenital hemolytic anemias, immune cytopenias, blood cancers, where spleen overactivity or splenic disease worsens systemic health.
-
Evidence of splenic mass, cyst, abscess or enlargement on imaging or physical exam - prompting further evaluation for possible tumor, infection, or structural disorder.
Because symptoms vary widely depending on underlying cause (trauma, blood disorder, infection, malignancy), diagnosing the need for splenectomy often requires careful evaluation, imaging, and blood work.
Diagnosis and Preoperative Evaluation for Splenectomy
Before performing a splenectomy, physicians undertake a thorough diagnostic and preparatory process to ensure correct indication, surgical safety, and optimal postoperative management. Key elements include:
-
Medical History & Physical Examination: Review of symptoms (abdominal pain, fullness, fatigue, infections), past illnesses, trauma history, bleeding or blood disorders. On physical exam, a doctor may palpate the abdomen to detect spleen enlargement (splenomegaly).
-
Blood Tests: Complete blood count (to check red cells, white cells, platelets), reticulocyte count (if hemolysis suspected), markers of hemolysis, liver and kidney function, coagulation profile, and any disease-specific labs (for suspected blood disorders, cancers).
-
Imaging Studies:
-
Ultrasound - to assess spleen size, structure, presence of masses or cysts, and to detect enlargement or structural abnormalities.
-
CT scan or MRI - when detailed imaging is needed (e.g. suspected tumor, cyst, abscess, or vascular involvement), or when spleen size is very large or anatomical relationships are unclear.
-
-
Functional & Immunological Assessment: Given spleen's role in immunity and blood filtration, preoperative evaluation often includes immunization history, vaccination planning (especially against bacteria for which the spleen provides immunity), and planning for prophylactic measures.
-
Risk Assessment & Optimization: Assess patient's overall health, comorbidities (especially if spleen removal is elective, not emergent), nutritional status, and prepare for surgery (blood transfusion if needed, stabilization in trauma cases, anesthesia evaluation).
-
Patient Counseling & Consent: Informing patient about benefits, risks (both short-term surgical risk and long-term infection/thrombosis risk), need for vaccinations, precautions post-splenectomy, and lifestyle implications. This ensures patient is fully aware and prepared.
This careful preoperative preparation helps ensure the surgery is justified, reduces surgical risks, and readies the patient for life after spleen removal.
Treatment Options - Performing Splenectomy & Aftercare
When a decision is made to remove the spleen, there are two primary surgical approaches - each chosen based on the clinical situation, spleen size, and patient condition.
Surgical Approaches
-
Laparoscopic Splenectomy:
-
A minimally invasive method using small incisions and a laparoscope (camera) to visualize and remove the spleen.
-
Preferred in elective cases (non-emergency), for smaller spleens or benign conditions.
-
Benefits include less postoperative pain, shorter hospital stay, faster recovery, fewer complications compared to open surgery.
-
-
Open Splenectomy:
-
Traditional method involving a larger incision in the abdomen, usually necessary when the spleen is very enlarged (massive splenomegaly), when there is active bleeding (trauma/rupture), or when complex anatomy or other organs' involvement exist.
-
Pre- and Postoperative Care
-
Vaccination & Prophylactic Measures: Because removal of the spleen reduces the body's ability to fight certain bacteria (especially encapsulated bacteria like Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis), patients are typically given recommended vaccines (pneumococcal, meningococcal, Hib, influenza) either before elective surgery or soon after recovery.
-
Antibiotic Prophylaxis (if indicated): Some patients - particularly children, immunocompromised, or those at higher risk - may be advised short-term or long-term prophylactic antibiotics, or to keep an “on-hand” course of antibiotics to begin immediately if signs of infection (fever, chills) appear.
-
Postoperative Recovery: After laparoscopic splenectomy, many patients recover in about 4-8 weeks before resuming normal activity. Post-surgery, patients may experience incision pain, some fatigue, and need gradual return to activity (walking, light chores), while avoiding heavy lifting or strenuous work until cleared.
-
Long-term Monitoring: Regular follow-up to monitor blood counts, immunization status, and general health. Patients are also advised to inform all healthcare providers (especially in emergencies or before other surgeries) that they are asplenic.
When Splenectomy Is Combined With Other Treatments
In case of blood disorders or cancers, splenectomy might be one part of a broader treatment plan - which could include chemotherapy, bone marrow therapy, or ongoing medications. In trauma or rupture cases, splenectomy might be performed with other abdominal surgeries depending on associated injuries.
Prevention and Management After Splenectomy
Since splenectomy removes a key immune organ, prevention and lifelong management become crucial. Key aspects include:
-
Ensuring Complete Vaccination: Patients should receive vaccines against pneumococcus, meningococcus, Haemophilus influenzae type b, and annual influenza; in some regions or situations additional vaccines (e.g. COVID-19) may be advised.
-
Promptness in Addressing Infections: Any sign of fever, chills, sore throat, respiratory infection, or other signs of infection must be taken seriously - even trivial symptoms can progress rapidly in asplenic individuals. Medical evaluation should be sought without delay.
-
Carrying Medical Alert / Asplenia Identification: Many physicians recommend that asplenic patients carry an alert card/bracelet stating their asplenic status - useful in emergencies, for other doctors or hospitals to know.
-
Education & Awareness: Patients should be educated about risks, preventive measures, and the need for vigilance. They should understand the importance of immunizations, hygiene, and timely reporting of signs of infection.
-
Healthy Lifestyle & Regular Health Checkups: Maintain balanced diet, avoid habits that may compromise immunity, and attend periodic follow-ups. In cases where splenectomy was done for blood disorders or hematologic diseases - continue with long-term disease management as advised by hematologist/physician.
With these measures, many asplenic individuals live healthy lives with minimal complications and significantly reduced risk of serious infections.
Complications and Risks of Splenectomy
Although splenectomy can be necessary and even life-saving, it is not without short-term and long-term risks. Understanding these helps in pre-surgical counseling and postoperative care:
Short-term / Surgical Risks
-
Bleeding/Hemorrhage: Because the spleen is highly vascular, splenectomy - especially in trauma or massive spleen - involves risk of significant blood loss, requiring careful surgical technique and sometimes transfusions.
-
Injury to Nearby Organs: During surgery, adjacent organs - pancreas, stomach, colon - may be inadvertently injured. Postoperative complications could include pancreatitis, leaks, or abscess formation.
-
Post-operative Complications: These include wound infections, pulmonary complications (atelectasis, pneumonia), abdominal discomfort, delayed healing, or thrombosis (blood clots) especially if platelet counts rise.
Long-Term Risks & Medical Consequences
-
Increased Risk of Serious Infections: Without a spleen, the body's ability to clear certain bacteria - especially encapsulated bacteria - is diminished. Patients have a lifelong increased risk of severe and sometimes rapidly progressing infections, including sepsis.
-
Overwhelming Post-Splenectomy Infection (OPSI): A rare but life-threatening condition where infections become overwhelming and can lead to sepsis. Requires immediate medical intervention.
-
Blood / Clotting Changes: After spleen removal, platelet counts can rise (thrombocytosis), increasing risk of blood clots (deep vein thrombosis, pulmonary embolism). Long-term risk of thromboembolic events is elevated.
-
Possible Long-Term Health Risks: Some studies suggest increased long-term risk of vascular diseases (e.g. pulmonary hypertension), and potential elevated risk of certain cancers and other comorbidities in asplenic patients.
-
Reduced Immune Surveillance & Altered Blood Filtering: Without the spleen's filtering function, damaged or old blood cells, debris, and some pathogens may remain in circulation - potentially affecting long-term blood health.
Given these risks, splenectomy is performed only when clearly indicated, and always with a plan for long-term preventive care, immunizations, and patient education.
Living with Splenectomy - Life After Spleen Removal
Removal of the spleen marks a significant change in the body's physiology, but many patients go on to lead healthy lives with proper care, awareness, and precautions. Key considerations for post-splenectomy living include:
Medical & Preventive Care
-
Keep vaccinations up to date (pneumococcal, meningococcal, Hib, influenza, and any other recommended by physicians).
-
Be alert to signs of infection - even minor symptoms can escalate quickly; seek prompt medical attention if fever, chills, sore throat, unexplained fatigue or aches arise.
-
Have a “medical alert” card/bracelet indicating asplenia, to inform health providers in emergencies.
-
Follow doctor's recommendations regarding prophylactic antibiotics (if advised), especially in early years after surgery or during high-risk periods (travel, other illnesses).
Lifestyle Modifications
-
Maintain a healthy, balanced lifestyle: good nutrition, regular exercise, avoiding smoking or excessive alcohol, and managing other comorbidities (e.g. diabetes, cardiovascular health).
-
Practice good hygiene and safe habits - especially when traveling, around crowded places, or areas with high infection risk.
-
Inform all healthcare providers (dentists, surgeons, other specialists) about history of splenectomy - so preventive antibiotics or other precautions can be taken before procedures.
Long-Term Monitoring and Support
-
Regular medical checkups to monitor blood counts, immune status, and general health.
-
Educate patients (and caretakers) about lifelong risks, so they remain vigilant and informed.
-
Encourage vaccination boosters as per medical guidance, and smooth access to prompt care if infection is suspected.
Many long-term studies indicate that with proper preventive care, patients without spleen can maintain good quality of life, similar physical and mental health outcomes to those with spleens - though they must remain more cautious about infections and blood health.
Top 10 Frequently Asked Questions about Splenectomy
1. What is a Splenectomy, and why is it performed?
A splenectomy is a surgical procedure in which the spleen-an organ located in the upper left part of the abdomen-is removed partially or completely. The spleen plays a major role in filtering blood, fighting infections, and storing red blood cells and platelets. A splenectomy is performed when the spleen becomes damaged, enlarged, infected, overactive, or cancerous, putting the patient at risk. It is commonly recommended for conditions such as traumatic spleen rupture, blood disorders, certain cancers, autoimmune conditions, and chronic infections. In many cases, removing the spleen is necessary to prevent life-threatening internal bleeding or to correct a condition in which the spleen destroys blood cells excessively, leading to severe anemia or low platelet counts.
2. What conditions commonly require a Splenectomy?
A splenectomy may be required to treat various medical conditions, including:
-
Traumatic injury from accidents causing spleen rupture
-
Idiopathic thrombocytopenic purpura (ITP) causing dangerously low platelets
-
Hereditary spherocytosis and other hemolytic anemias
-
Hypersplenism, in which the spleen destroys blood cells excessively
-
Cancers like lymphoma, leukemia, or metastatic tumors affecting the spleen
-
Chronic splenic infections or abscesses that fail antibiotic treatment
-
Cysts or benign tumors causing pain or risk of rupture
-
Portal hypertension with significant splenic enlargement
Depending on the cause, the surgeon will determine whether a partial or total splenectomy is appropriate.
3. How is Splenectomy surgery performed?
A splenectomy can be performed using two main approaches:
Laparoscopic Splenectomy:
This minimally invasive method uses small incisions, a camera, and surgical instruments. The surgeon separates the spleen from surrounding tissues and removes it through a small opening. This procedure offers reduced pain, faster recovery, and smaller scars.
Open Splenectomy:
Used when the spleen is very large, ruptured, or when complications are present. A larger incision is made in the abdomen to access and remove the spleen. This approach allows greater visibility when dealing with severe trauma or internal bleeding.
During the surgery, blood vessels supplying the spleen are clipped and sealed, and the organ is carefully separated from nearby structures like the stomach, pancreas, and colon.
4. What are the risks and complications of Splenectomy?
Although splenectomy is generally safe, it carries certain risks due to the spleen's role in immune function. Common complications include:
-
Infection, particularly serious infections due to loss of splenic immune activity
-
Bleeding during or after surgery
-
Pancreatic injury since the pancreas lies close to the spleen
-
Blood clots in the portal or splenic veins
-
Pneumonia or lung-related complications
-
Overwhelming Post-Splenectomy Infection (OPSI) - a rare but life-threatening infection
-
Abscess formation at the surgical site
The risk of severe infection persists lifelong, making preventive vaccinations and early treatment of fevers extremely important.
5. What is the recovery process like after a Splenectomy?
Recovery depends on whether the splenectomy was laparoscopic or open:
-
Laparoscopic: Patients may return home within 1-2 days and resume normal activities within 2-4 weeks.
-
Open surgery: Recovery takes longer, often 4-6 weeks, because of the larger incision and deeper tissue healing.
During recovery, patients may experience fatigue, abdominal soreness, mild constipation, or decreased appetite. Regular follow-ups are important to monitor blood counts, wound healing, and early signs of infection. Patients should avoid strenuous activity and heavy lifting until fully healed.
6. How does removing the spleen affect the immune system?
The spleen is essential for producing antibodies and filtering bacteria from the bloodstream. After splenectomy, the body becomes more vulnerable to infections, especially from certain bacteria like Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis. Because of this:
-
Vaccinations are crucial before and after surgery
-
Preventive antibiotics may be recommended, especially for children
-
Patients must seek immediate medical attention if they develop fever or signs of infection
Although other organs like the liver and lymph nodes partially take over spleen functions, the immune system will never fully regain the same capability.
7. What vaccinations are needed before and after Splenectomy?
To reduce infection risks, patients should receive several vaccinations, ideally 2 weeks before elective splenectomy or as soon as possible after emergency splenectomy. These include:
-
Pneumococcal vaccine
-
Haemophilus influenzae type b (Hib) vaccine
-
Meningococcal vaccines
-
Influenza vaccine annually
Some patients may require booster doses every 5-10 years. These vaccines significantly reduce the risk of overwhelming post-splenectomy infection (OPSI).
8. Will I need to take antibiotics or medications after Splenectomy?
Yes, depending on age and risk factors. Many surgeons recommend:
-
Daily prophylactic antibiotics, especially for children and immunocompromised adults
-
Emergency antibiotics to take immediately if fever develops before reaching a hospital
-
Blood-thinning medications, in some cases, to prevent post-operative clot formation
These measures help protect the patient from serious infections and vascular complications.
9. Are there long-term lifestyle changes after Splenectomy?
Patients without a spleen must adopt lifelong preventive health habits, including:
-
Immediate evaluation of fevers, as infections progress faster without a spleen
-
Strict adherence to vaccinations and recommended booster doses
-
Avoiding exposure to animal bites, as certain infections are more common
-
Wearing medical alert bracelets indicating “No Spleen” in emergencies
-
Carrying emergency antibiotics when traveling to remote areas
-
Practicing good hygiene and avoiding contact with sick individuals
Most people can live normal, active lives, but consistent preventive care is essential.
10. How successful is Splenectomy, and what is the long-term outlook?
Splenectomy is highly successful in treating many conditions, especially ITP,
hereditary blood disorders, splenic rupture, and
hypersplenism. For trauma patients, it is lifesaving. For blood
disorders, it often improves red blood cell or platelet counts significantly.
Long-term outlook is excellent if patients follow preventive measures, complete all
recommended vaccinations, take antibiotics when needed, and seek prompt care for
infections. With proper management, most individuals lead full, healthy lives without a
spleen.


