Introduction to Stapedectomy
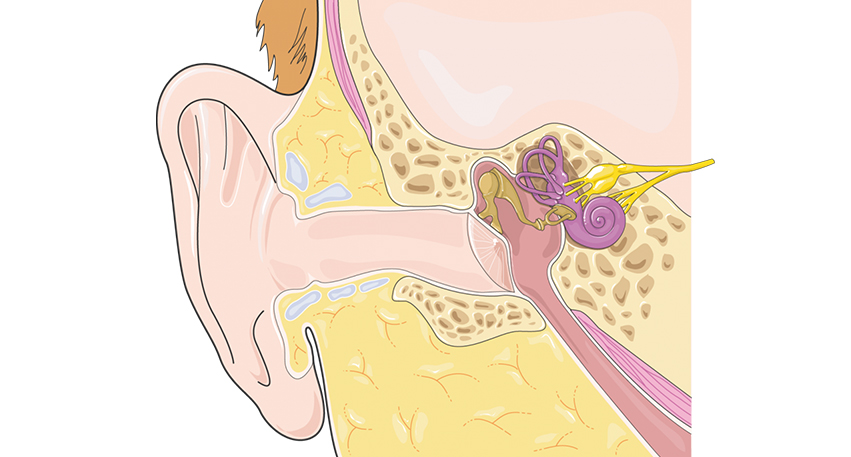
Stapedectomy is a delicate and highly specialized ear surgery performed to restore hearing in patients suffering from conductive hearing loss, usually caused by a condition known as otosclerosis. This surgery focuses on one of the three tiny bones in the middle ear - the stapes (also called the “stirrup bone”). The stapes is responsible for transmitting sound vibrations from the middle ear to the inner ear (cochlea), where these vibrations are converted into electrical signals that the brain interprets as sound.
In certain individuals, the stapes becomes fixed or immobile due to abnormal bone growth, preventing it from vibrating properly. This disruption in sound transmission leads to hearing impairment, which cannot be corrected by medications alone. The stapedectomy procedure involves removing part or all of the immobile stapes bone and replacing it with a micro-prosthesis - a small, piston-shaped artificial implant that restores the chain of vibration between the middle and inner ear.
This surgery is considered one of the most successful microsurgical interventions in otology, with very high success rates in improving hearing. It has evolved significantly over the decades, incorporating refined surgical instruments, laser technology, and biocompatible prosthetic materials that enhance safety, precision, and outcomes. For patients who have struggled with hearing aids or progressive hearing loss due to stapes fixation, stapedectomy offers a long-term and often life-changing solution.
Causes and Risk Factors for Stapedectomy
The main underlying cause that necessitates a stapedectomy is otosclerosis - a disease that affects the bony capsule of the inner ear. Otosclerosis leads to abnormal bone remodeling around the oval window and stapes footplate, gradually fusing the stapes bone and rendering it immobile. When the stapes cannot move freely, sound waves cannot pass effectively into the cochlea, resulting in conductive hearing loss.
Key Causes and Contributing Factors:
-
Genetic Inheritance: Otosclerosis often runs in families. If one or both parents have the condition, their children have a higher likelihood of developing it.
-
Hormonal Factors: Hormonal fluctuations - such as during pregnancy, menopause, or hormone therapy - can accelerate the progression of otosclerosis, particularly in women.
-
Viral Triggers: Certain viral infections, especially measles, have been linked to abnormal bone remodeling in the middle ear.
-
Metabolic or Autoimmune Causes: Calcium metabolism disorders and autoimmune responses may play a role in the onset or progression of abnormal bone growth around the stapes.
-
Congenital Abnormalities: Rarely, congenital fusion or malformation of the ossicular chain (ear bones) can mimic otosclerosis and require surgical correction through a stapedectomy.
Risk Factors:
-
Family history of hearing loss or otosclerosis
-
Female gender (more commonly affected)
-
Early adult onset of progressive hearing impairment
-
Multiple pregnancies or hormonal changes
-
Exposure to repeated loud noises or chronic ear infections
When these factors lead to significant hearing impairment that cannot be adequately managed with hearing aids, stapedectomy becomes a definitive treatment option.
Symptoms and Signs Suggesting Stapedectomy May Be Needed
Patients with stapes fixation or otosclerosis typically experience gradual, painless, and progressive hearing loss that worsens over months or years. Because the condition affects sound transmission rather than nerve function, the initial loss is conductive in nature - meaning sounds are soft or muffled but speech remains clear when made louder.
Common Symptoms Include:
-
Progressive Hearing Loss: The earliest and most prominent symptom. The person may notice that sounds seem distant or muted and may struggle to follow conversations, particularly in noisy environments.
-
Tinnitus (Ringing in the Ear): A high-pitched or buzzing sound that often accompanies otosclerosis and may intensify as hearing deteriorates.
-
Paracusis Willisii: A curious symptom where patients hear better in noisy environments because others speak louder - a classic hallmark of conductive hearing loss.
-
Imbalance or Mild Vertigo: Occasionally, patients may feel brief dizziness or unsteadiness due to changes in middle-ear pressure or fluid transmission.
-
Family History of Hearing Problems: Relatives, particularly women, may report similar hearing loss or surgeries for otosclerosis.
If these symptoms appear - especially progressive hearing loss in one or both ears without ear infection or trauma - it is essential to consult an ENT specialist for evaluation. Early detection allows for timely surgical correction before severe hearing decline occurs.
Diagnosis and Preoperative Evaluation
Accurate diagnosis is crucial for determining if a patient is a suitable candidate for stapedectomy. The goal of the evaluation is to confirm that the hearing loss is conductive (mechanical) rather than sensorineural (nerve-related), and that the middle ear's anatomy is favorable for surgical reconstruction.
Diagnostic Steps Include:
-
Audiometry (Hearing Test): The main test to measure air and bone conduction. Conductive hearing loss presents as a distinct gap between air and bone conduction thresholds, while bone conduction remains near normal.
-
Speech Audiometry: Evaluates how well patients recognize words and speech at different sound levels, helping assess functional impact of hearing loss.
-
Tympanometry and Acoustic Reflex Testing: Determines middle-ear compliance and stapes mobility. An absent stapedial reflex is a common indicator of stapes fixation.
-
High-Resolution CT Scan: In selected cases, imaging of the temporal bone helps visualize ossicular anatomy, confirm stapes fixation, and rule out other causes of hearing loss.
-
Physical Examination (Otoscopy): The eardrum typically appears normal, distinguishing otosclerosis from conditions such as chronic otitis media or eardrum perforation.
-
Preoperative Counseling: Once confirmed, the patient is counseled about surgical options, expected outcomes, risks, and the recovery process.
Only patients with a well-defined conductive loss, healthy inner ear function, and no active infection or fluid in the middle ear are considered suitable for surgery.
Treatment and Surgical Procedure of Stapedectomy
Stapedectomy is typically performed under local or general anesthesia, depending on patient comfort and surgical preference. It is carried out under a microscope through the ear canal - meaning there are no external incisions or visible scars.
Step-by-Step Surgical Process:
-
Accessing the Middle Ear: The eardrum is carefully lifted to expose the ossicles.
-
Assessing the Ossicular Chain: The surgeon confirms the immobility of the stapes and checks the integrity of the other bones (malleus and incus).
-
Removal of the Stapes: The fixed stapes superstructure (its upper part) is delicately removed, leaving the footplate intact.
-
Creating an Opening (Fenestration): A small hole is made in the stapes footplate to provide access to the inner ear fluid chamber.
-
Prosthesis Insertion: A micro-prosthesis made of titanium, Teflon, or platinum is attached to the incus and inserted into the created opening, re-establishing the sound conduction pathway.
-
Sealing and Reconstruction: A tissue graft (often from the patient's own ear lining) is placed to seal the area and prevent fluid leakage.
-
Closure: The eardrum is gently repositioned, and the ear canal is packed with a soft dressing for support during healing.
The entire procedure usually takes 60-90 minutes. Most patients can go home the same day or after an overnight stay. Hearing improvement often begins within a few weeks, and optimal results are achieved within 6-8 weeks as healing completes.
Prevention and Postoperative Management
Since otosclerosis and stapes fixation are largely hereditary and not preventable, the emphasis lies on early detection and postoperative management to ensure long-term success.
Key Management Steps:
-
Post-Surgical Care: Patients are advised to avoid straining, sneezing with a closed mouth, flying, or swimming for several weeks to prevent pressure changes in the middle ear.
-
Protect the Ear: Keep the ear dry and avoid inserting objects or earphones during recovery.
-
Follow-Up Visits: Regular follow-ups at 1 week, 1 month, and 3 months are essential to monitor healing, perform hearing tests, and check prosthesis stability.
-
Medication: Short courses of antibiotics and anti-inflammatory drugs are prescribed to prevent infection and control swelling.
-
Lifestyle and Hearing Protection: Avoid loud noises and environments that may strain the ear. Proper ear care and overall health maintenance promote sustained results.
With diligent adherence to medical advice and gentle ear care, stapedectomy results can last for decades, providing durable hearing restoration.
Complications and Risks of Stapedectomy
Although stapedectomy is a safe and effective operation, it remains a microsurgical procedure near delicate structures, and a few risks exist. The complication rate is low, especially with experienced surgeons, but patient awareness is important.
Possible Complications Include:
-
Dizziness or Vertigo: Mild imbalance or spinning sensation is common in the first few days due to inner-ear irritation but typically subsides quickly.
-
Taste Alteration: The chorda tympani nerve, responsible for taste on part of the tongue, runs near the surgical field and may be temporarily affected, causing altered taste or dryness.
-
Tinnitus Persistence: While many patients notice an improvement in tinnitus, some may experience persistence or temporary worsening after surgery.
-
Infection: Rare, but can occur if the ear is exposed to water or if postoperative care is neglected.
-
Hearing Deterioration: A small percentage of patients may experience sensorineural hearing loss if inner-ear trauma or prosthesis displacement occurs.
-
Prosthesis Displacement: In rare cases, the implant may shift from its position, leading to recurrence of hearing loss. Revision surgery may be necessary to restore hearing.
-
Perilymph Leak: Leakage of inner-ear fluid during or after surgery can cause dizziness or hearing changes but is preventable with careful sealing techniques.
Fortunately, with modern surgical precision, success rates exceed 90%, and serious complications are exceedingly rare.
Living with the Condition After Stapedectomy
Life after stapedectomy is generally fulfilling, as most patients regain a level of hearing close to normal and can participate in social, professional, and family activities with renewed confidence.
What to Expect After Surgery:
-
Gradual Hearing Recovery: Some improvement may be noticed within days, but maximum hearing gain often appears over several weeks.
-
Return to Daily Life: Light activities can usually resume after a week, but strenuous exercise and heavy lifting should be avoided for a few weeks.
-
Follow-Up Audiometry: A repeat hearing test is conducted after 6-8 weeks to evaluate results and compare hearing improvement to preoperative levels.
-
Long-Term Outlook: Most patients enjoy decades of improved hearing with minimal maintenance. If mild recurrence occurs years later, adjustments or minor revision procedures can help.
Emotional and Social Benefits:
-
Enhanced communication and confidence
-
Improved work performance and relationships
-
Reduced dependence on hearing aids
-
Relief from frustration and social isolation caused by hearing impairment
With responsible ear care, periodic hearing assessments, and adherence to medical guidance, the benefits of a stapedectomy can last a lifetime.
Top 10 Frequently Asked Questions about Stapedectomy
1. What is a Stapedectomy, and why is it performed?
A stapedectomy is a delicate ear surgery performed to treat otosclerosis, a condition in which the stapes bone (one of the three small bones in the middle ear) becomes fixed and unable to vibrate properly. This fixation prevents sound waves from passing from the middle ear to the inner ear, leading to conductive hearing loss. During a stapedectomy, the surgeon removes all or part of the immobilized stapes bone and replaces it with a tiny prosthetic device. This prosthesis restores the transmission of sound vibrations, thereby significantly improving hearing and reducing symptoms such as tinnitus.
2. What conditions typically require Stapedectomy?
Stapedectomy is most commonly recommended for:
-
Otosclerosis, where abnormal bone growth immobilizes the stapes
-
Congenital abnormalities of the stapes bone
-
Trauma-related fixation or degeneration of middle ear bones
-
Progressive conductive hearing loss despite using hearing aids
Patients with stable sensorineural hearing and healthy inner ear function usually benefit greatly from this surgery.
3. How is the Stapedectomy procedure performed?
The surgery is typically performed under local anesthesia with sedation, or sometimes general anesthesia. The main steps include:
-
Ear canal access: The surgeon works through the ear canal without external incisions.
-
Lifting the eardrum: The eardrum is gently moved aside to access the stapes bone.
-
Removing the stapes: The fixed stapes is removed either entirely or partially.
-
Creating a micro-hole: A tiny hole is made in the footplate of the stapes (if it's left in place).
-
Inserting a prosthesis: A small metallic or plastic piston-like prosthesis is placed between the incus and the opening in the inner ear.
-
Repositioning the eardrum: The eardrum is placed back in position and the ear is packed for healing.
The surgery usually takes 60-90 minutes, and most patients return home the same day.
4. What is the difference between Stapedectomy and Stapedotomy?
While both surgeries treat otosclerosis, the main difference lies in how much of the stapes bone is removed:
-
Stapedectomy: The entire stapes bone or a major portion is removed before inserting the prosthesis.
-
Stapedotomy: Only a small hole is made in the footplate of the stapes; the bone is not fully removed.
Stapedotomy is often preferred today because it is less invasive, offers quicker healing, and carries a lower risk of inner ear trauma. However, stapedectomy remains effective, especially in certain anatomical situations.
5. What are the risks and complications of Stapedectomy?
Stapedectomy has a high success rate, but potential complications include:
-
Temporary or permanent dizziness
-
Taste disturbances due to nerve involvement
-
Persistent or worsening tinnitus
-
Eardrum perforation
-
Infection or inflammation
-
Prosthesis displacement requiring revision surgery
-
Sensorineural hearing loss, which is rare but serious
-
Facial nerve injury (extremely rare due to modern techniques)
Most risks can be minimized with skilled surgical technique and proper post-operative care.
6. What does recovery look like after Stapedectomy?
Recovery is generally smooth and well tolerated. Patients may experience:
-
Mild dizziness for a few days
-
A feeling of fullness or pressure in the ear
-
Slight pain or tenderness
-
Temporary hearing fluctuations
Patients are advised to avoid water entering the ear, vigorous nose blowing, heavy lifting, and air travel for a few weeks. Packing inside the ear is removed within 1-2 weeks, and most patients return to normal routines within 7-14 days. Full recovery may take up to 6 weeks, with hearing improvement becoming more noticeable as healing progresses.
7. How effective is Stapedectomy in improving hearing?
Stapedectomy has an extremely high success rate, with 80-95% of patients experiencing significant hearing improvement. Many regain near-normal hearing, while others notice enhanced sound clarity and speech understanding. The procedure often reduces or eliminates conductive hearing loss, allowing individuals to rely less on hearing aids or stop using them entirely.
8. Will I experience any pain or discomfort after the surgery?
Most patients report minimal pain after surgery. Common symptoms include:
-
Mild earache
-
Slight dizziness
-
Sensitivity to loud sounds
-
Temporary taste changes
These usually resolve within a few days. Pain medication and home care instructions provided by the surgeon help ensure a smooth recovery.
9. Are there any long-term precautions after undergoing Stapedectomy?
While most people resume normal activities soon after surgery, certain long-term precautions may be advised:
-
Avoiding extreme pressure changes such as scuba diving
-
Preventing water from entering the ear during early healing
-
Avoiding sudden, forceful nose-blowing
-
Protecting the ear from trauma
-
Regular follow-up checkups to monitor the prosthesis
Most people return to daily life without permanent restrictions, but individual recommendations may vary based on anatomy and healing.
10. Can hearing loss return after Stapedectomy?
While the results of stapedectomy are long-lasting, hearing loss may recur in some cases due to:
-
Progressive otosclerosis affecting other structures
-
Prosthesis displacement or loosening
-
Age-related hearing loss
-
Middle ear infections or fluid buildup
If hearing worsens, evaluation by an ENT specialist is recommended. Revision surgery or hearing aids may be considered depending on the cause.


