Introduction to Surgery for Stroke Prevention
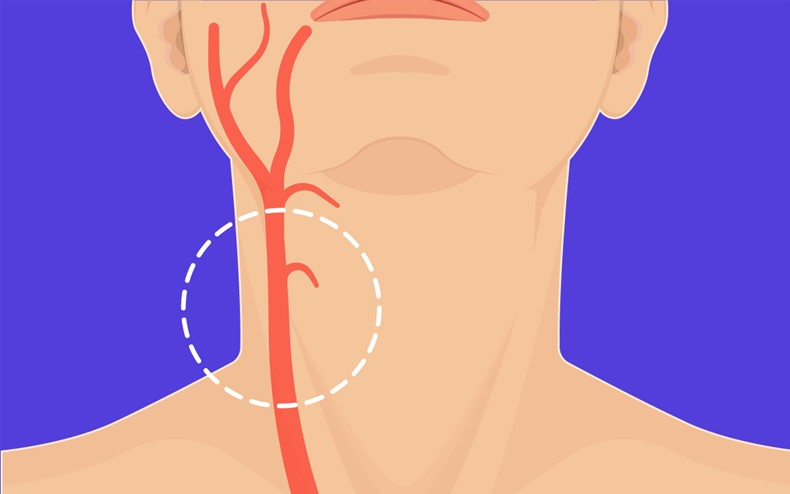
Stroke remains one of the leading causes of death and long-term disability worldwide. While many strokes result from a sudden clot blocking blood flow to the brain (ischemic stroke), a substantial portion are linked to narrowing (stenosis) or blockage of arteries supplying the brain - especially the carotid arteries. Over time, this narrowing (often from plaque buildup) can cause clots to form or plaque fragments to dislodge, traveling to cerebral vessels and triggering a stroke.
"Surgery for stroke prevention" refers to a set of procedures aimed at reducing the risk of future strokes by correcting underlying vascular problems before they lead to severe brain injury. Instead of waiting for a devastating event, these interventions proactively repair or open up arteries, remove or stabilize plaque, and restore adequate blood flow - thereby preventing clot formation or embolization that could lead to stroke.
The two main procedures used for this purpose are:
-
Carotid Endarterectomy (CEA) - a surgical operation to remove plaque from the carotid artery.
-
Carotid Artery Stenting (CAS) - a less invasive, catheter-based method where a stent is placed to widen the narrowed artery and stabilize plaque.
Thanks to decades of research, these approaches - along with optimized medical therapy - have become standard parts of stroke prevention strategies. Their use is guided by careful patient selection, degree of artery narrowing, and timing relative to symptoms.
Causes and Risk Factors Necessitating Surgery for Stroke Prevention
Stroke-preventive surgery is typically considered when there is a high risk that narrowing or disease of brain-supplying arteries will lead to a future stroke. Key causes and risk factors include:
-
Atherosclerosis (plaque build-up): Over years, fatty deposits, cholesterol, calcium and cellular debris accumulate in the artery wall, narrowing the lumen and making the artery prone to clot formation or plaque rupture.
-
High-grade carotid artery stenosis: When the narrowing in the internal carotid artery (ICA) reaches moderate to severe levels (e.g., 50%-99% depending on symptoms), blood flow becomes compromised and risk of embolism increases.
-
Symptomatic carotid disease: Patients who have already had a transient ischemic attack (TIA), "mini-stroke," temporary vision loss (amaurosis fugax), or minor stroke may have unstable plaque or high embolic potential - making preventive surgery more urgent.
-
Asymptomatic but severe stenosis with risk factors: Even in patients without symptoms, if imaging reveals severe stenosis and additional risk factors (like age, plaque characteristics, comorbidities), preventive surgery may offer stroke risk reduction.
-
Risk factors for atherosclerosis progression: These include high blood pressure, high cholesterol, diabetes, smoking, sedentary lifestyle, age, and other vascular risk factors. When plaque buildup is advanced, medical therapy alone might not suffice.
-
Plaque instability or ulceration: Some plaques are more "vulnerable" - soft, inflamed, prone to rupture. These are more likely to generate clots or debris that can travel to the brain.
In short: when the combination of artery narrowing, plaque characteristics, symptoms (or high-risk asymptomatic disease) and patient factors indicate a high stroke risk - surgery may be the recommended preventive measure.
Symptoms and Signs that Suggest Need for Stroke-Prevention Surgery
Because vascular disease can be silent or slowly progressive, not all patients scheduled for stroke-prevention surgery have dramatic symptoms. But there are common warning signs and clinical features that often trigger the diagnostic evaluation:
Common Symptoms
-
Transient Ischemic Attack (TIA) - temporary neurological symptoms (weakness, numbness, speech difficulty, vision problems) that resolve within minutes to hours. TIAs are often a red flag indicating unstable carotid stenosis.
-
Minor stroke or non-disabling cerebrovascular event - when a patient has had a mild stroke (without permanent severe disability) but imaging shows carotid artery stenosis.
-
Amaurosis fugax (temporary monocular vision loss) - caused by small emboli traveling to the eye's circulation, often a warning sign of carotid plaque.
-
"Whistling" or bruits over neck arteries - sometimes on physical exam, turbulence in a narrowed carotid artery can be heard (though not all narrowings produce bruit, and not all bruits mean high-grade stenosis).
Silent or Subclinical Signs
-
Severe carotid narrowing on routine imaging (ultrasound, CT angiography, MRI) even without symptoms.
-
High-risk plaque characteristics (ulceration, soft/inflammatory plaque) seen on imaging - may indicate elevated embolic risk even if patient is asymptomatic.
-
Repeated "near-miss" events - e.g. transient dizziness, transient weakness, sensory changes - even if they do not meet criteria for TIA.
Thus, not only acute strokes or TIAs, but also subtle or silent vascular changes can prompt evaluation and decision for preventive surgery.
Diagnosis Before Surgery for Stroke Prevention
Before recommending surgery, clinicians follow a detailed diagnostic pathway - to assess the extent of artery disease, plaque characteristics, overall stroke risk, and patient suitability for surgery or stenting. Key components include:
-
Vascular imaging: Duplex (ultrasound) of the carotid arteries, CT angiography (CTA), MR angiography (MRA) or conventional angiography. This helps measure the degree of stenosis (percentage narrowing), plaque morphology (soft vs calcified, ulcerated), and involvement (unilateral or bilateral carotids).
-
Neurological history and examination: Reviewing history of TIAs, strokes, transient visual symptoms, neurological deficits; neurological exam to establish baseline and rule out contraindications.
-
Assessment of comorbidities: Heart disease, lung disease, kidney function, prior neck surgeries or radiation (which may influence risk of surgery or stenting), and overall fitness for anesthesia.
-
Risk stratification and timing: Especially in symptomatic patients, timing is critical. Studies show best benefit when surgery is done early after symptoms (ideally within 2 weeks).
-
Multidisciplinary discussion: Vascular surgeons, neurologists/neuro-vascular specialists, anesthetists - to weigh benefits vs risks, decide between open surgery (endarterectomy) vs stenting, or medical therapy.
Only after careful evaluation and patient counselling, a decision is made whether to proceed with surgery, opt for stenting, or continue optimized medical therapy.
Treatment Options for Stroke Prevention
"Surgery for stroke prevention" today primarily involves two treatment paths - each with specific indications, advantages, and trade-offs. In many cases, the choice depends on patient risk, anatomy, comorbidities, and operator/surgeon experience.
Carotid Endarterectomy (CEA)
-
What it is: A surgical procedure where an experienced vascular surgeon opens the affected carotid artery in the neck and removes the atherosclerotic plaque along with the thickened inner lining, thereby restoring normal lumen diameter and blood flow.
-
When indicated: Especially recommended for symptomatic patients (those who had TIA, minor stroke, retinal ischemia) with stenosis typically ≥50-70%, depending on individual risk and guidelines. The greatest benefit is when the surgery is done soon after the ischemic event, ideally within 2 weeks. For selected asymptomatic patients with severe stenosis (e.g. 70-99%) and low surgical risk, CEA may also be considered.
-
Benefits: Significant reduction in future stroke risk (especially ipsilateral stroke), durable long-term results, well-established procedure with decades of outcome data.
Carotid Artery Stenting (CAS)
-
What it is: A minimally invasive, catheter-based procedure. Through a small puncture (usually in the groin or wrist), a thin catheter with a stent is guided up to the narrowed carotid artery, where the stent is deployed to widen the artery and stabilize the plaque against further rupture.
-
When indicated: CAS is often preferred in patients who are high-risk for open surgery - e.g. severe comorbidities (heart disease, lung disease), prior neck radiation or surgery, anatomic difficulties, or those with contralateral carotid occlusion. It may also be preferred in symptomatic patients under a certain age (some studies suggest benefit under 70 years).
-
Benefits: Less invasive, shorter recovery time, avoids neck incision, suitable for patients who cannot tolerate open surgery. Recent advances in stent design and procedural techniques have improved safety and efficacy.
Medical Therapy Alone (When Surgery/Stenting Not Indicated)
In patients with mild stenosis, low plaque risk, or high perioperative risk, optimized medical therapy remains a cornerstone. This includes antiplatelet drugs, statins, blood pressure and lipid control, diabetes management, lifestyle modification - sometimes combined with close surveillance imaging to periodically reassess the artery.
Prevention and Management: Before and After Surgery
Surgical intervention is only one part of a comprehensive stroke prevention strategy. Long-term success depends heavily on both pre-operative preparation and post-operative care.
Before Surgery
-
Risk factor control: Aggressive management of hypertension, diabetes, high cholesterol, smoking cessation, weight control.
-
Antiplatelet / statin therapy: Often started well before surgery when stenosis is identified, to stabilise plaque, reduce inflammation and lower risk of perioperative events.
-
Patient optimization: Ensuring good general health, controlling comorbidities, optimizing cardiac and respiratory status, evaluating anesthesia risk.
-
Patient education and informed consent: Making sure patients understand potential benefits and risks, need for follow-up, lifestyle changes, and possibilities (stenting vs surgery vs medical therapy).
After Surgery / Stenting
-
Post-procedure monitoring: Observation for perioperative complications (stroke, bleeding, cranial nerve injury), vital signs, neurological assessment.
-
Medications: Continued antiplatelet therapy (often aspirin or dual therapy as per protocols), statins, blood pressure and lipid control.
-
Lifestyle measures: Healthy diet, regular exercise, smoking cessation, controlling risk factors - essential to prevent further atherosclerosis and plaque formation.
-
Regular follow-up imaging: Periodic duplex/ultrasound or other vascular imaging to monitor for restenosis (re-narrowing), especially after stenting.
-
Long-term medical care: Management of comorbid conditions (diabetes, hypertension), adherence to medications, rehab if needed, and regular neurologic check-ups to detect new symptoms early.
This combined approach - surgery (if indicated) + medical therapy + lifestyle modification + vigilant follow-up - maximizes long-term stroke prevention and vascular health.
Complications and Risks of Stroke-Prevention Surgery
While carotid endarterectomy and stenting are proven stroke-prevention procedures, they carry inherent risks. Understanding these is essential for informed consent and risk-benefit assessment.
Risks of Carotid Endarterectomy (CEA)
-
Perioperative stroke or death - although rare when performed by experienced surgeons, it remains the most feared complication. Guidelines recommend that the combined stroke/death rate should be under 6%.
-
Heart attack, myocardial infarction - due to stress of surgery in patients with underlying heart disease.
-
Nerve injury - cranial or cervical nerves (e.g., hypoglossal, vagus, glossopharyngeal) may be affected, leading to temporary or rarely permanent swallowing, vocal, or sensory issues.
-
Bleeding, hematoma, wound complications - bleeding at surgical site, hematoma formation, neck swelling.
-
Risks related to general anesthesia - especially in older patients or those with comorbidities.
Risks of Carotid Artery Stenting (CAS)
-
Periprocedural stroke or transient ischemic attack - during stent deployment, manipulation of catheters may dislodge plaque or cause emboli to the brain. Historically, CAS had slightly higher periprocedural stroke risk compared to CEA, especially in older patients.
-
Restenosis (re-narrowing) - over time, the artery can re-narrow due to intimal hyperplasia or plaque re-accumulation, requiring surveillance and possibly re-intervention.
-
Stent-related complications - stent fracture, in-stent thrombosis, or in-stent restenosis; need for antiplatelet therapy long-term.
-
Access site complications - bleeding, hematoma at puncture site, arterial injury.
General Considerations
-
Patient selection is critical - benefits outweigh risks only in properly selected patients (degree of stenosis, symptoms, comorbidities, life expectancy).
-
Perioperative care and surgical expertise matter - outcomes are substantially better in experienced centers with low complication rates.
-
Need for long-term follow-up - because even after "successful" surgery/stenting, patients remain at risk for disease progression elsewhere, restenosis, new plaque formation, or stroke from other causes (cardiac embolism, small vessel disease).
Living with the Condition After Stroke-Prevention Surgery / Stenting
Undergoing surgery or stenting for stroke prevention is a life-changing intervention - but long-term health requires ongoing vigilance, lifestyle commitment, and medical follow-up. Key aspects of living well after the procedure:
-
Adherence to medications - antiplatelets, statins, blood pressure and diabetes medications must be continued as advised, to prevent new plaque formation and stabilize existing vessels.
-
Lifestyle modifications - healthy diet, exercise, smoking cessation, weight management, controlling cholesterol and blood pressure. These remain critical to prevent new vascular disease or recurrence.
-
Regular check-ups - periodic imaging (ultrasound, Doppler) to monitor for restenosis or new stenosis, especially after stenting; neurological evaluation if new symptoms arise.
-
Patient education and risk awareness - understanding that surgery reduces risk, but does not eliminate it; other factors (heart rhythm problems, small vessel disease, lifestyle) also contribute to stroke risk.
-
Multidisciplinary care - coordination between neurologist, vascular surgeon, primary physician, and possibly rehabilitation specialists to manage overall vascular health.
-
Quality-of-life and mental well-being - many patients feel relieved, but there can be anxiety about recurrence; patient support, counselling, and risk-factor control help maintain long-term confidence and health.
For many patients, successful carotid surgery or stenting - combined with good medical and lifestyle care - offers substantial reduction in future stroke risk, better vascular health, and peace of mind.
Top 10 Frequently Asked Questions about Surgery for Stroke Prevention
1. What is stroke prevention surgery, and why is it necessary?
Stroke prevention surgery refers to medical procedures designed to reduce the risk of stroke, particularly in patients at high risk due to conditions like carotid artery disease, atrial fibrillation, heart valve problems, and blockages in the arteries. These procedures aim to restore blood flow, prevent blood clots, or address the underlying causes of stroke. Stroke prevention surgery is often recommended for patients who are at high risk but cannot manage their condition through medication or lifestyle changes alone.
2. What are the common types of surgery for stroke prevention?
Several types of surgery may be performed to prevent strokes, including:
-
Carotid endarterectomy (CEA): A procedure to remove plaque buildup from the carotid arteries (the major blood vessels in the neck) to improve blood flow to the brain.
-
Carotid artery stenting: In this minimally invasive procedure, a stent (a small mesh tube) is placed in a narrowed or blocked carotid artery to keep it open.
-
Heart valve repair or replacement: In cases where valve disease contributes to blood clots, surgery to repair or replace the valve may be necessary.
-
Left atrial appendage closure (LAAC): A procedure to close off the left atrial appendage in patients with atrial fibrillation to prevent blood clots from forming.
-
Bypass surgery for blocked arteries in the brain or neck may be performed in rare cases of severe vascular disease.
The specific surgery depends on the cause of stroke risk and the patient's overall health.
3. How is a Carotid Endarterectomy (CEA) performed?
Carotid endarterectomy is performed to remove plaque from the carotid arteries to prevent stroke. The procedure is usually done under local anesthesia or general anesthesia and involves:
-
A small incision is made on the neck to access the carotid artery.
-
The artery is carefully opened to remove the plaque (fatty deposits and blood clots) causing the blockage.
-
The artery is then stitched back together, and blood flow is restored.
-
A bypass graft may be used if the artery is severely damaged.
This procedure is typically effective in reducing the risk of stroke, particularly when done early in the disease process.
4. What is carotid artery stenting, and how does it work?
Carotid artery stenting is a minimally invasive procedure used to treat narrowed or blocked carotid arteries, a major risk factor for stroke. In this procedure:
-
A catheter is inserted through the groin or wrist and guided to the carotid artery.
-
A balloon catheter is used to expand the narrowed artery, and a stent (small mesh tube) is placed to keep the artery open.
-
The catheter is removed, and the artery is now open, allowing improved blood flow to the brain.
Carotid artery stenting is typically recommended for patients who are not good candidates for carotid endarterectomy, especially those with high surgical risks.
5. What are the risks and complications associated with surgery for stroke prevention?
Like all surgeries, stroke prevention procedures carry some risks, including:
-
Stroke or transient ischemic attack (TIA) during or after surgery
-
Bleeding or hematoma at the incision site
-
Infection
-
Nerve injury, leading to temporary or permanent changes in sensation or function (e.g., difficulty swallowing)
-
Restenosis, or re-narrowing of the treated artery, requiring further treatment
-
Heart complications, especially in patients with underlying heart disease
-
Blood clot formation in the artery or around the surgical site
However, these complications are rare, especially when performed by an experienced vascular surgeon, and are usually managed effectively.
6. How long is the recovery period after surgery for stroke prevention?
Recovery time depends on the type of surgery performed:
-
Carotid Endarterectomy: Most patients stay in the hospital for 1-2 days and can return to normal activities within 2-3 weeks.
-
Carotid Artery Stenting: Recovery is typically quicker, with patients able to go home the same day or after a short hospital stay. Full recovery may take 1-2 weeks.
-
Heart valve surgery or LAAC: These procedures generally have a longer recovery time, with patients requiring 4-6 weeks to resume normal activities.
During recovery, patients are advised to avoid heavy lifting, strenuous exercise, and activities that could increase the risk of complications.
7. How effective are these surgeries in preventing stroke?
Both carotid endarterectomy and carotid artery stenting have been shown to significantly reduce the risk of stroke in patients with carotid artery disease. The effectiveness depends on factors like:
-
The severity of the blockage or plaque
-
How early the surgery is performed
-
The patient's overall health and comorbidities
In general, carotid endarterectomy can reduce stroke risk by up to 50% for patients with significant carotid artery narrowing. Stenting is also effective, though slightly less so than endarterectomy, and is typically used for patients who cannot tolerate surgery.
8. Who is a good candidate for surgery for stroke prevention?
Good candidates for surgery for stroke prevention include:
-
Patients with carotid artery disease causing significant narrowing (70% or more)
-
Individuals with a history of transient ischemic attacks (TIAs) or minor strokes
-
Patients with atrial fibrillation at risk for blood clots in the heart
-
Individuals with heart valve disease contributing to stroke risk
-
Patients with significant blockages in the brain's blood vessels that could lead to stroke
-
Individuals who are otherwise healthy enough to undergo surgery and anesthesia
A thorough evaluation by a vascular surgeon or cardiologist is required to determine whether surgery is the best option.
9. What lifestyle changes should be made after stroke prevention surgery?
After surgery, lifestyle changes are crucial to maximize the benefits of treatment and reduce the risk of future strokes. These include:
-
Taking prescribed medications, such as blood thinners, statins, or antihypertensive medications
-
Adopting a heart-healthy diet rich in fruits, vegetables, and whole grains, and low in saturated fats and cholesterol
-
Exercising regularly, such as walking or swimming, to improve cardiovascular health
-
Quitting smoking and reducing alcohol intake
-
Managing blood pressure, cholesterol, and diabetes
-
Regular follow-up appointments with healthcare providers to monitor progress
These lifestyle adjustments are essential in preventing further strokes and maintaining overall health.
10. What is the long-term outlook after stroke prevention surgery?
The long-term outlook after surgery is generally positive, especially when the
surgery is
performed early and combined with lifestyle changes. Most patients experience a
significant reduction in stroke risk and improved quality of life.
However, ongoing monitoring is essential to detect any issues, such as restenosis
(re-narrowing of the artery), or other cardiovascular concerns.
The key to long-term success includes:
-
Adhering to prescribed medications and lifestyle changes
-
Regular follow-up with healthcare providers
-
Maintaining a healthy weight and blood pressure
With proper care, most patients can expect a positive recovery and significantly reduced stroke risk.


