Introduction to Surgical Treatment of Cancer
Surgical treatment for cancer remains one of the most widely used and effective treatments in modern oncology. Cancer surgery, a specialized branch of surgery called surgical oncology, involves the removal of tumors and surrounding tissue in order to treat cancer. Surgery can be used as a curative treatment, as well as a diagnostic, preventive, and palliative measure depending on the type and stage of cancer.
Cancer surgery is often the most direct method to remove a tumor from the body, providing patients with the best chances for survival, especially when the tumor is localized and has not spread. It plays a significant role in reducing the size of tumors and providing relief from symptoms. Surgical procedures can vary widely from simple excisions to complex multi-stage operations.
Surgical oncology combines expertise in surgery with knowledge of cancer biology, anatomy, and the patient's unique clinical situation. Surgery can be used not only to remove the tumor but also to take biopsies for diagnostic confirmation, remove surrounding tissue that may be at risk, and improve a patient's quality of life by reducing pain or obstruction caused by the cancer.
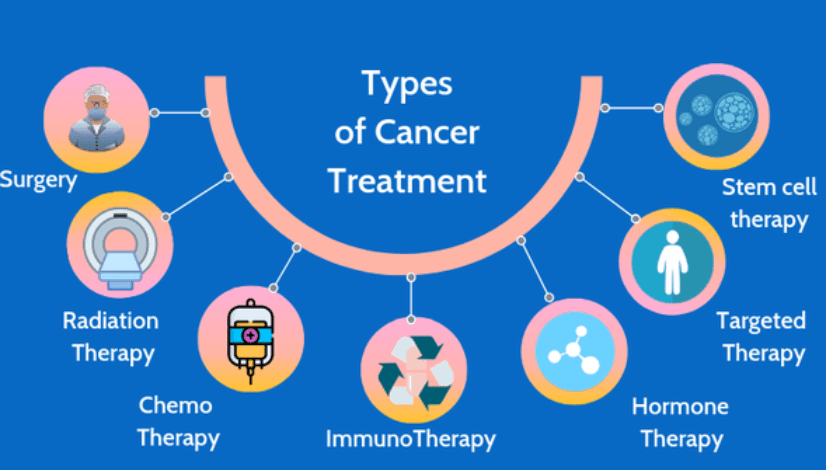
However, surgery is rarely the only option. Most cancers are treated with a combination of surgery, chemotherapy, radiation therapy, and immunotherapy. Surgery is particularly effective when the cancer is diagnosed in its early stages, before it has spread (metastasized) to other parts of the body. Despite its benefits, surgery carries risks and requires careful consideration by the medical team.
Causes and Risk Factors for Surgical Treatment of Cancer
While cancer itself does not have a single cause, certain risk factors increase the likelihood of developing cancer and influence the decision to undergo surgery. Surgery is more commonly recommended when a cancer is localized and has not spread to distant organs. Understanding the causes and risk factors for cancer surgery can help determine the most appropriate approach for treatment.
Genetic Factors
Some cancers are linked to genetic mutations, which are inherited and predispose individuals to developing certain types of cancer. For example, mutations in the BRCA1 and BRCA2 genes significantly increase the risk of breast and ovarian cancers. Individuals with inherited mutations may consider preventive surgery (such as prophylactic mastectomy or oophorectomy) to reduce the risk of cancer. Additionally, certain inherited conditions like Lynch syndrome predispose people to colorectal cancer, making them potential candidates for early surgical intervention to remove at-risk tissues before cancer develops.
Age and Gender
Age is one of the most significant factors in determining cancer risk. As people age, their cells accumulate genetic mutations that increase the risk of cancer. The likelihood of developing cancer rises significantly after age 50, making older adults more likely to undergo cancer surgery. Gender also plays a role in risk factors: for example, breast cancer predominantly affects women, while prostate cancer is more common in men.
Lifestyle and Environmental Factors
Cigarette smoking is the most common cause of lung cancer and increases the risk for several other cancers, including throat, mouth, bladder, and pancreas cancers. Excessive alcohol consumption has been linked to cancers of the liver, esophagus, and mouth. Exposure to carcinogens like asbestos or certain chemicals in the workplace can increase the risk of developing mesothelioma or other cancers.
Sun exposure is a significant risk factor for skin cancer. A history of frequent sunburns or tanning bed use can increase the risk of melanoma. Poor diet, obesity, and lack of physical activity also raise the risk of certain cancers, including colorectal, kidney, and uterine cancers.
Other Factors
Other conditions, such as chronic inflammation, autoimmune diseases, or previous cancer treatments (like radiation), can increase the risk of developing a second malignancy. The presence of precancerous lesions, such as polyps in the colon, or actinic keratosis (a precancerous skin condition), may lead to surgical removal to prevent cancer development.
Surgical treatment is usually considered when the cancer is localized or can be surgically resected. The size and location of the tumor play a significant role in determining whether surgery is the right treatment. Tumors that are deeply embedded in critical areas or that have spread to multiple organs may not be operable. In such cases, other treatments such as chemotherapy or radiation are preferred.
Symptoms and Signs of Cancer Requiring Surgical Intervention
Cancer often develops silently, with no obvious signs or symptoms until it has progressed significantly. Therefore, recognizing symptoms early can increase the likelihood of successful treatment. Symptoms that suggest cancer may require surgical intervention vary depending on the cancer's location, type, and progression. Some general symptoms include:
Lumps or Masses
A lump or mass that appears unexpectedly, particularly in the breast, neck, abdomen, or limbs, can be a warning sign of cancer. In breast cancer, this is often the first sign, and the tumor may be palpable during a self-exam or physical examination by a healthcare professional. Similarly, swelling or a mass in the lymph nodes, especially in the neck or armpits, may indicate lymphoma or other cancers.
Pain
Cancer can cause persistent pain, which may worsen over time as the tumor grows and presses against surrounding tissues, organs, or nerves. Bone pain is common in cancers like osteosarcoma or metastatic breast cancer. Pain in the abdomen can indicate tumors in the liver, pancreas, or gastrointestinal tract.
Weight Loss and Fatigue
Unexplained weight loss, often accompanied by loss of appetite, is a classic symptom of cancer. This can occur in cancers like pancreatic cancer, colon cancer, and lung cancer. Fatigue, which is persistent and unexplained, can also be a sign of cancer and is often seen in leukemia, lymphoma, and other blood cancers.
Bleeding or Discharge
Bleeding or unusual discharge may be a symptom of cancers like colorectal cancer, bladder cancer, or uterine cancer. For instance, rectal bleeding, blood in the stool, or changes in bowel movements can indicate colon cancer, while abnormal vaginal bleeding can be a sign of uterine or ovarian cancer.
Changes in Organ Function
Cancer can affect organ function, leading to symptoms like difficulty swallowing (in esophageal or throat cancers), shortness of breath (in lung cancer), or jaundice (in liver cancer). Changes in bowel or urinary habits, such as frequent urination or constipation, may indicate bladder or colorectal cancer.
Visible Skin Changes
Skin cancer may manifest as a new mole or a change in an existing mole, such as in melanoma. Non-healing sores, skin discoloration, or abnormal growths on the skin can also signal the presence of skin cancer, particularly basal cell carcinoma or squamous cell carcinoma.
If any of these symptoms occur, it is essential to seek medical evaluation to rule out cancer and other conditions. Early diagnosis often allows for surgical intervention, especially if the cancer is confined to one area.
Diagnosis (Pre-Surgical Assessment and Staging)
The first step in determining whether surgery is appropriate is confirming the diagnosis of cancer through a variety of diagnostic tools. After a cancer diagnosis, staging is performed to determine how far the disease has spread. Staging is essential to decide whether surgery alone can treat the cancer or if additional treatments like chemotherapy or radiation are necessary.
Imaging Studies
Several imaging techniques are used to assess the size, location, and spread of the tumor. Common imaging studies include:
-
X-rays: A traditional imaging technique used to identify abnormalities in bones and organs.
-
CT scans (Computed Tomography): Detailed cross-sectional images that help assess the tumor's size, location, and spread to nearby structures.
-
MRI (Magnetic Resonance Imaging): Provides high-resolution images of soft tissues, helpful in detecting tumors in the brain, spinal cord, and pelvic organs.
-
PET scans (Positron Emission Tomography): Used to detect cancer spread throughout the body by highlighting areas of high metabolic activity typical of cancer cells.
Biopsy
A biopsy is the gold standard for confirming cancer. During a biopsy, a sample of the tumor or suspicious tissue is removed and examined under a microscope. Biopsy can be done in several ways, including:
-
Needle biopsy: A thin needle is inserted into the tumor to extract tissue samples.
-
Endoscopic biopsy: A flexible tube is used to view and collect tissue from the tumor.
-
Surgical biopsy: Performed when the tumor is inaccessible using other methods.
Staging Surgery
For some cancers, the surgeon may perform staging surgery to check for cancer spread to nearby lymph nodes or organs. This may involve removing lymph nodes for examination or exploring the abdomen or chest to determine the extent of cancer. Staging helps determine if surgery can remove all cancerous tissue or if additional treatments are necessary.
Blood Tests
Blood tests are often used to assess a patient's overall health and the presence of certain cancer markers. For example, elevated levels of PSA (prostate-specific antigen) may indicate prostate cancer, and CA-125 levels may suggest ovarian cancer. Blood tests also help evaluate liver and kidney function, vital for deciding if the patient is fit for surgery.
General Health Evaluation
Before surgery, a comprehensive health evaluation is conducted, which includes a physical examination, organ function tests, and a review of any pre-existing medical conditions. This assessment ensures that the patient can tolerate anesthesia and the stress of surgery.
Treatment Options for Surgical Cancer Treatment
Surgical treatment for cancer can be broadly categorized based on the cancer type, stage, and whether the surgery is curative, preventive, diagnostic, or palliative. Some of the main types of cancer surgery include:
Curative Surgery
Curative surgery aims to remove the entire tumor and surrounding tissue, potentially curing the cancer. This is most effective when the tumor is localized and has not spread to other parts of the body. Examples include:
-
Lumpectomy or mastectomy for breast cancer.
-
Colectomy for colon cancer.
-
Prostatectomy for prostate cancer.
Preventive Surgery
Preventive surgery, or prophylactic surgery, is recommended for individuals at high risk of developing cancer. This is often performed when precancerous changes are detected or if an individual carries a genetic predisposition to certain cancers. Examples include:
-
Prophylactic mastectomy in individuals with a high risk of breast cancer due to a genetic mutation (e.g., BRCA1).
-
Oophorectomy for women at high risk of ovarian cancer.
Diagnostic Surgery
Diagnostic surgery is performed to confirm cancer or to provide a tissue sample for biopsy. This is essential for making an accurate diagnosis and determining the cancer's type and grade. A diagnostic surgery may involve removing a portion of a tumor for biopsy or conducting exploratory surgery to identify the extent of cancer.
Debulking (Cytoreductive) Surgery
When it is not possible to remove the entire tumor, debulking surgery aims to reduce the size of the tumor to make other treatments, such as chemotherapy or radiation therapy, more effective. This type of surgery is often used in advanced cancers, such as ovarian cancer or pancreatic cancer, where complete removal is not possible.
Palliative Surgery
Palliative surgery is performed when cancer is at an advanced stage and cannot be cured. The goal is to alleviate symptoms and improve quality of life. This might include removing tumors that are obstructing organs (such as the colon or intestines), draining fluid buildup, or relieving pressure caused by a tumor.
Reconstructive Surgery
After the removal of cancerous tissue, reconstructive surgery can restore function or appearance, especially when the cancer affects visible or functional areas of the body. For example, after a mastectomy, a woman may undergo breast reconstruction, or after skin cancer removal, reconstructive surgery may help restore facial appearance.
Minimally Invasive Surgery
In recent years, minimally invasive surgery has become more common in cancer treatment. Techniques like laparoscopic surgery and robotic-assisted surgery use small incisions and specialized instruments to remove tumors. These approaches result in shorter hospital stays, faster recovery times, and reduced scarring.
Prevention and Management of Surgical Treatment of Cancer
After surgery, long-term prevention and management are essential for ensuring that cancer does not return and that the patient recovers fully. The steps taken after surgery depend on the type of cancer, the surgery performed, and the patient's overall health.
Post-Surgery Recovery
Recovery after cancer surgery varies depending on the extent of the surgery. Patients are monitored closely in the hospital for complications such as bleeding, infection, and pain management. After being discharged, recovery at home may include rest, limited physical activity, and wound care. Physical therapy may be necessary to regain function, especially if the surgery involved removing or reconstructing a body part, such as a limb or organ.
Follow-Up Care
Patients must undergo regular follow-up appointments after surgery to monitor for signs of recurrence. This may involve physical exams, imaging tests, blood tests, and biopsies. The frequency of these appointments will decrease over time, but patients should remain vigilant for any new symptoms.
Adjuvant Therapies
After surgery, many patients will undergo adjuvant therapies such as chemotherapy, radiation therapy, or immunotherapy to eliminate any remaining cancer cells. These treatments can help reduce the risk of recurrence and improve long-term survival.
Lifestyle Changes
Patients are often encouraged to adopt healthy lifestyle changes to improve recovery and prevent cancer recurrence. This includes eating a balanced diet, engaging in regular physical activity, and avoiding known carcinogens such as smoking and excessive alcohol consumption.
Complications of Surgical Treatment for Cancer
Like any major surgery, cancer surgery carries risks, and patients should be aware of the potential complications. Some common complications include:
-
Infection: Any surgical procedure carries the risk of infection at the incision site or internally.
-
Blood Clots: Surgery increases the risk of blood clots, which can be dangerous if they travel to the lungs, heart, or brain.
-
Organ Dysfunction: Depending on the location of the surgery, patients may experience temporary or permanent loss of organ function.
-
Lymphedema: Removal of lymph nodes during surgery can cause fluid buildup, leading to swelling in the arms or legs.
-
Chronic Pain: Post-surgical pain can persist long after the procedure, especially if nerves were damaged during surgery.
-
Scarring: Significant scarring may result, particularly with larger incisions, potentially impacting body image.
Living with the Condition of Surgical Treatment for Cancer
After cancer surgery, patients face a new normal. The transition from active treatment to recovery and survivorship can be difficult but is also a time for regaining strength, adjusting to lifestyle changes, and focusing on long-term health.
Rehabilitation and Recovery
Rehabilitation programs, including physical therapy, occupational therapy, and speech therapy, may be necessary depending on the type of surgery performed. This helps the patient regain mobility, strength, and independence. For example, after a mastectomy, breast reconstruction and physical therapy may help restore appearance and function.
Emotional Support and Mental Health
Living with cancer and adjusting to life after surgery can take an emotional toll. Patients may experience feelings of depression, anxiety, or survivor's guilt. Mental health counseling, support groups, and family support can be invaluable in helping patients cope with these feelings.
Regular Monitoring and Lifestyle Adjustments
Patients must maintain regular follow-up care to monitor for signs of recurrence. In addition to medical follow-up, lifestyle changes, including a balanced diet, regular exercise, and avoiding cancer-causing substances, are key to long-term health.
Top 10 Frequently Asked Questions about Surgical Treatment of Cancer
1. What is the role of surgery in cancer treatment?
Surgery plays a pivotal role in cancer treatment, primarily when a tumor is localized and accessible. It can be used for diagnostic purposes (biopsy), to confirm the presence of cancer, or to stage the disease and assess its extent. In some cases, surgery is performed with the intent to cure cancer by completely removing a tumor or cancerous tissue. Surgical intervention is also employed to debulk large tumors, reducing their size to ease the effectiveness of other treatments like chemotherapy or radiation. In more advanced stages, surgery may serve a palliative role, offering symptom relief and improving the quality of life, for example, by removing blockages caused by tumors. In short, surgery is often part of a multimodal treatment approach, combining with other therapies to provide the best possible outcomes.
2. What are the different types of cancer surgery?
Cancer surgeries are categorized based on their intent and purpose:
-
Curative Surgery: This aims to completely remove cancerous tumors and tissue. It's most commonly done when the tumor is localized, and it's feasible to remove it entirely without causing harm to vital organs.
-
Preventive Surgery: This surgery is performed to remove precancerous tissue or organs that may have a high likelihood of developing cancer in the future (e.g., removal of ovaries in women with BRCA mutations).
-
Diagnostic Surgery: Involves obtaining a tissue sample (biopsy) to confirm whether cancer is present.
-
Debulking Surgery: In some cases, when a tumor cannot be completely removed, surgeons may opt to remove as much as possible to alleviate symptoms and make subsequent treatments more effective.
-
Palliative Surgery: This type of surgery does not cure cancer but aims to ease symptoms, such as relieving pain, pressure, or obstruction caused by a tumor, thus improving the patient's comfort.
3. How is cancer surgery performed — open surgery, minimally invasive, or other methods?
Cancer surgery can be performed through various methods, depending on the location of the cancer, its size, and the general health of the patient:
-
Open Surgery: Traditional surgery involving a large incision to access the tumor. It's necessary for tumors located in deep or hard-to-reach areas.
-
Minimally Invasive Surgery: Techniques such as laparoscopy or thoracoscopy use small incisions and a camera to guide the surgical tools. This approach generally results in less pain, shorter recovery times, and smaller scars.
-
Robotic Surgery: In robotic-assisted surgery, the surgeon controls robotic arms for increased precision, often used in delicate or complex procedures. The precision allows for quicker recovery and better cosmetic results.
4. Who decides if I need surgery for cancer — and when is surgery recommended?
The decision to undergo surgery is a team decision made by various medical specialists. A surgeon, oncologist, and often other specialists will assess the situation, considering factors such as the type of cancer, its location, stage, and the patient's overall health. Surgery is recommended if the cancer is localized and can be safely removed. It's often the first line of defense for cancers like breast cancer, colon cancer, and melanoma. In more advanced stages, surgery may be combined with chemotherapy or radiation to increase the likelihood of success. In some cases, surgery may be done first to reduce tumor size before other treatments begin.
5. What tests or preparation are needed before cancer surgery?
Before undergoing surgery, the patient will typically undergo a series of preoperative tests to evaluate their overall health. These may include blood tests, imaging (such as CT scans, MRIs, or X-rays) to assess the size and spread of the tumor, and cardiological or pulmonary tests if needed. These tests help the surgeon understand the extent of the cancer and also ensure the patient is fit for surgery. Additionally, patients are usually advised to avoid eating or drinking for several hours before surgery, and some medications may need to be paused. A discussion with the surgical team will also cover post-surgery care, including pain management, recovery expectations, and lifestyle changes.
6. What are the risks and possible complications of cancer surgery?
As with any major surgery, cancer surgery carries risks such as infection, bleeding, blood clots, and anesthesia complications. Specific complications depend on the type of surgery and the area operated on. For example, surgeries that involve the removal of lymph nodes may lead to lymphedema (swelling due to fluid buildup), while surgeries near the abdomen or pelvis may affect digestion and bowel movements. In some cases, if a tumor is close to critical organs, surgery might affect the function of those organs. Recovery times vary, and some patients may experience temporary fatigue or mobility issues. Therefore, a thorough discussion with the surgeon about these risks is essential.
7. Will I need other treatments (chemotherapy, radiation) along with surgery?
Surgery is often only one part of a broader treatment plan. For many cancers, especially if the cancer has spread beyond the initial site, surgery is followed by chemotherapy and/or radiation therapy to ensure that any remaining cancer cells are destroyed. This is referred to as adjuvant therapy. In some cases, chemotherapy or radiation may even be given before surgery to shrink the tumor and make it easier to remove (called neoadjuvant therapy). The need for these additional treatments is determined by the type and stage of cancer.
8. What happens after surgery — what should I expect during recovery and follow-up?
Post-surgery recovery varies based on the type of surgery and the patient's overall health. Some common recovery steps include managing pain, avoiding heavy lifting, following wound care instructions, and gradually returning to normal activities. The first few weeks after surgery may involve fatigue, swelling, or discomfort, which should improve over time. Regular follow-up appointments are crucial to monitor for any signs of recurrence, manage any ongoing side effects, and assess the patient's physical and emotional recovery. Depending on the type of surgery, follow-up might include imaging tests, lab tests, or physical therapy.
9. What if the surgeon cannot remove all cancer — what does “debulking” or “incomplete removal” mean?
Sometimes, due to the location of the tumor or its size, it may not be possible to remove it entirely. In such cases, the surgeon will perform a debulking procedure, where as much of the tumor as possible is removed to reduce its size and improve symptoms. This may not cure the cancer but can enhance the effectiveness of other treatments such as chemotherapy or radiation. If the tumor is inoperable, doctors will discuss alternative treatments aimed at managing the disease and improving the patient's quality of life.
10. How to discuss with my doctor — what important questions should I ask before undergoing cancer surgery?
Before deciding to undergo cancer surgery, it's important to have a thorough discussion with the surgical team. Key questions include:
-
What type of surgery is recommended and why?
-
What are the expected benefits and risks of this surgery?
-
How long will the recovery take, and what should I expect during the recovery process?
-
Will I need additional treatments (chemotherapy or radiation) after surgery?
-
What kind of side effects or complications can I expect, and how are they managed?
By having these questions answered, patients can make a well-informed decision about their surgical treatment and feel more confident in their care plan.


