Introduction to Thyroplasty
Thyroplasty is a surgical procedure that is designed to alter the structure of the thyroid cartilage or the framework of the larynx (voice box), which can help improve vocal cord function, address airway problems, or restore normal vocal cord movement. This surgery is often recommended for patients who have voice-related issues caused by structural problems with the vocal cords, such as vocal cord paralysis, weakness, or dysfunction, leading to voice hoarseness, difficulty speaking, or airway obstruction.
The thyroid cartilage, which is located in the larynx (voice box), plays a crucial role in protecting the vocal cords and enabling voice production. When the vocal cords become paralyzed or weakened due to injury, surgery, or other medical conditions, thyroplasty may be recommended to improve vocal fold closure and restore voice quality.
Thyroplasty can be performed for a variety of reasons, including vocal cord paralysis (either unilateral or bilateral), functional voice disorders, glottic insufficiency, and even for aesthetic purposes such as voice feminization or pitch modification. There are various types of thyroplasty surgeries depending on the specific needs of the patient, including medialization thyroplasty, lateralization thyroplasty, and relaxation thyroplasty. The goal is to improve the alignment of the vocal cords and restore proper voice production.
While thyroplasty is an effective procedure, it is important to note that it is usually recommended only after other conservative treatments, such as voice therapy or injections, have failed or when structural corrections are necessary for optimal voice production.
Causes and Risk Factors for Thyroplasty
Thyroplasty is typically performed to treat vocal cord paralysis, glottic insufficiency, or other voice disorders that arise from the dysfunction of the vocal cords. Understanding the causes and risk factors behind these conditions is crucial for determining when thyroplasty is necessary.
Causes of Vocal Cord Dysfunction:
-
Vocal Cord Paralysis/Paresis:
One of the leading causes of vocal cord dysfunction is paralysis or paresis (weakness) of one or both vocal cords. This condition may result from damage to the recurrent laryngeal nerve, which controls the muscles responsible for vocal cord movement. Causes of nerve damage include:-
Neck or thyroid surgery: Surgical procedures in the neck region can inadvertently damage the recurrent laryngeal nerve.
-
Trauma or injury: Accidents or injuries to the neck area can lead to nerve damage or direct injury to the vocal cords.
-
Viral infections: Viral infections such as the flu or viral laryngitis can cause inflammation and damage to the vocal cords or the nerves.
-
Stroke or neurological conditions: Conditions like stroke or Parkinson’s disease can lead to weakness or paralysis of the vocal cords.
-
-
Glottic Insufficiency:
Glottic insufficiency occurs when the vocal cords do not come together properly, preventing full closure of the glottis during speech or swallowing. This condition can lead to a weak or breathy voice and is often seen in:-
Aging (Presbylaryngitis): As people age, the vocal cords can lose elasticity, tone, and strength, leading to voice changes.
-
Vocal Cord Atrophy: The thinning and weakening of the vocal cord tissues can prevent the cords from meeting fully during phonation, resulting in a breathy, weak voice.
-
-
Cancer and Tumors in the Larynx:
Thyroid cancer or other cancers in the head and neck region can cause paralysis or dysfunction of the vocal cords. Surgery or radiation therapy used to treat these cancers may also damage the vocal cords or the nerves controlling them. -
Structural Abnormalities or Congenital Conditions:
Some people are born with anatomical abnormalities in their larynx that affect the function of their vocal cords. This can include conditions like congenital vocal cord paralysis, where one or both vocal cords are immobile from birth.
Risk Factors for Vocal Cord Dysfunction:
-
Surgical History:
Previous surgeries on the neck, such as thyroidectomy, can result in damage to the recurrent laryngeal nerve, leading to vocal cord paralysis or dysfunction. -
Radiation Therapy:
Individuals who have undergone radiation therapy for head and neck cancers are at increased risk for damage to the vocal cords and the recurrent laryngeal nerve. -
Neurological Disorders:
Certain neurological conditions, such as stroke, Parkinson’s disease, or multiple sclerosis, can increase the risk of vocal cord dysfunction. -
Age:
As people age, the structures of the larynx and vocal cords naturally weaken, leading to conditions like presbylaryngitis, where the voice becomes weaker and more difficult to produce. -
Trauma or Injury:
Direct trauma to the neck or head, including accidents or physical abuse, can cause damage to the vocal cords or the nerves responsible for their movement.
Symptoms and Signs of Thyroplasty
Thyroplasty is typically considered when individuals experience significant symptoms that affect their voice, swallowing, or breathing. The most common symptoms and signs that may indicate the need for thyroplasty include:
Voice-Related Symptoms:
-
Hoarseness or Breathy Voice:
One of the primary symptoms that prompt individuals to seek medical help is a hoarse or breathy voice. This can result from vocal cord paralysis or atrophy, where the cords fail to come together properly during phonation. -
Weak or Limited Vocal Strength:
People with vocal cord dysfunction may find that their voice lacks power and they tire quickly when speaking, especially during prolonged conversations or vocal exertion. -
Voice Fatigue:
Prolonged speaking or vocal use can result in voice fatigue, where the person feels their voice is “tiring out” quickly. This is common in individuals with incomplete vocal cord closure.
Swallowing and Breathing Difficulties:
-
Difficulty Swallowing (Dysphagia):
Swallowing difficulties may occur when the vocal cords cannot fully close during swallowing, increasing the risk of food or liquid entering the windpipe and causing aspiration. This is particularly problematic in individuals with vocal cord paralysis. -
Frequent Choking or Aspiration:
Aspiration occurs when food or liquids enter the lungs instead of the stomach. People with vocal cord dysfunction may experience frequent choking episodes or aspiration, which can lead to recurrent lung infections and other complications. -
Breathing Difficulties:
If the vocal cords are not functioning properly, they may fail to fully open during inhalation, causing shortness of breath or stridor (a high-pitched wheezing sound). This is more common in individuals with bilateral vocal cord paralysis.
Physical Examination Findings:
-
Visible Swelling in the Neck:
A noticeable lump or swelling in the neck could be a sign of an enlarged thyroid or goiter, which can affect the function of the vocal cords. -
Change in Voice Pitch or Quality:
Patients may notice changes in their voice pitch or quality, such as a higher-pitched or strained voice, which can indicate dysfunction or weakness of the vocal cords.
Diagnosis of Thyroplasty
The diagnosis of the condition requiring thyroplasty involves several key steps, starting with a thorough medical evaluation and followed by specific diagnostic tests to assess the function of the vocal cords.
Medical History and Clinical Examination:
-
A complete medical history is taken to assess the onset of symptoms, any previous surgeries, trauma, or radiation therapy, and the impact on voice, swallowing, and breathing.
-
The doctor will also conduct a physical examination of the neck and larynx, checking for visible signs of swelling, growths, or abnormalities.
Laryngoscopy and Stroboscopy:
-
Flexible or Rigid Laryngoscopy: A camera is inserted into the throat to visually inspect the vocal cords during phonation and at rest. This allows the physician to assess the position, movement, and overall health of the vocal cords.
-
Stroboscopy: This technique uses a strobe light to visualize the vocal cords' vibration during speech. It helps assess the quality of the vocal cords’ movement and determine whether there is any abnormality in their function.
Voice Assessment:
-
A speech-language pathologist (SLP) may conduct a voice evaluation to measure the patient's vocal quality, pitch, loudness, and endurance. The results of this assessment will help determine the severity of the vocal dysfunction and whether thyroplasty is necessary.
Imaging Tests:
-
Ultrasound or CT/MRI Imaging: In cases where structural abnormalities or tumors are suspected, imaging tests such as ultrasound, CT scans, or MRI may be used to obtain detailed views of the thyroid, larynx, and surrounding structures.
Treatment Options of Thyroplasty
There are several different types of thyroplasty, each designed to address a specific vocal cord dysfunction. The type of surgery chosen depends on the condition being treated, the patient's overall health, and the surgeon's experience.
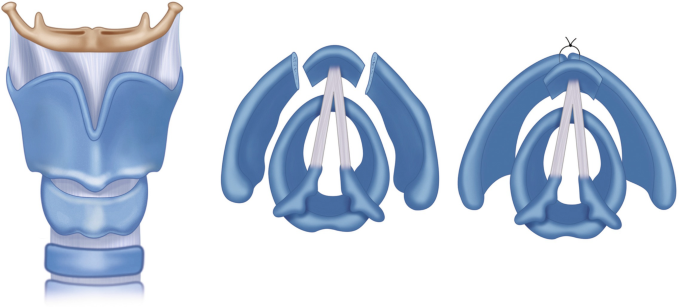
Types of Thyroplasty:
-
Type I (Medialization Thyroplasty): This is the most common type of thyroplasty and is used to treat vocal cord paralysis or glottic insufficiency. An implant is placed into the thyroid cartilage to push the paralyzed vocal cord towards the midline, allowing for better closure of the vocal cords during phonation.
-
Type II (Lateralization Thyroplasty): This is less common and is used to treat cases of airway insufficiency caused by a mispositioned vocal cord that is obstructing the airway. This procedure involves moving the vocal cords outward to widen the airway.
-
Type III (Relaxation Thyroplasty): This type of thyroplasty is used for pitch alteration, typically to deepen the voice. It is commonly used in cases of voice feminization or to treat individuals with an excessively high voice pitch due to vocal cord dysfunction.
-
Type IV (Cricothyroid Approximation): This type of thyroplasty is used to lengthen or tension the vocal cords, raising the pitch of the voice. It is often used in gender-affirming voice surgeries to achieve a higher-pitched voice in transgender women.
-
Combination Procedures: In some cases, multiple types of thyroplasty may be combined to address both voice and airway issues. For example, medialization thyroplasty may be combined with arytenoid adduction to improve posterior glottic closure.
Surgical Technique:
-
Procedure Overview: The procedure is typically performed under general anesthesia. A small incision is made in the neck, and the thyroid cartilage is carefully exposed. Depending on the type of thyroplasty, an implant is inserted into the thyroid cartilage to adjust the position of the vocal cords. The surgeon may also use sutures to secure the vocal cords in their new position.
-
Postoperative Care: After the surgery, patients are generally advised to rest their voice for a few days to promote healing. They may also be given antibiotics to prevent infection and pain medication to manage discomfort.
Prevention and Management of Thyroplasty
While thyroplasty is a surgical treatment, proper management before, during, and after the procedure is essential to ensure the best outcomes.
Before Thyroplasty:
-
Preoperative Counseling: Patients should be fully informed about the potential risks and benefits of the surgery. They should also have realistic expectations about the outcomes, including the potential for changes in voice quality, pitch, and breathing.
-
Voice Rest: Patients are typically advised to avoid vocal strain before the procedure to prevent further damage to the vocal cords.
-
Medical Optimization: Any underlying medical conditions, such as respiratory issues or heart disease, should be managed before surgery to reduce the risk of complications.
Postoperative Management:
-
Voice Rest: After surgery, patients are advised to rest their voice for several days to allow the vocal cords to heal properly. They should avoid whispering, yelling, or straining their voice during the recovery period.
-
Follow-up Care: Patients will need to have regular follow-up visits with their surgeon to monitor the progress of healing and ensure the implant is positioned correctly.
-
Voice Therapy: After the initial recovery period, voice therapy with a speech-language pathologist is often recommended to optimize voice function and prevent any compensatory voice patterns from forming.
Complications of Thyroplasty
As with any surgical procedure, thyroplasty carries certain risks. The most common complications include:
-
Infection: As with any surgery, there is a risk of infection at the incision site or within the larynx itself.
-
Bleeding: Although rare, bleeding can occur during surgery or in the immediate postoperative period, leading to the formation of a hematoma (blood collection) that may interfere with breathing or voice function.
-
Implant Displacement: In some cases, the implant used in medialization thyroplasty may shift or become displaced, requiring further surgery.
-
Vocal Cord Injury: There is a risk of damaging the vocal cords during surgery, which could result in worsening of voice quality or further dysfunction.
-
Breathing Problems: In rare cases, surgery may lead to worsening airway issues, particularly if the vocal cords are moved too far or not positioned correctly.
Living with the Condition of Thyroplasty
Following thyroplasty, patients can generally expect significant improvement in voice quality and function, though it is important to manage expectations and understand the long-term care requirements.
Recovery Timeline:
-
Short-Term Recovery: Most patients can return to normal activities within 1–2 weeks, although they may need to avoid strenuous activities and heavy voice use during the initial recovery period.
-
Voice Rehabilitation: After the healing process, voice therapy is typically recommended to help the patient adjust to any changes in voice quality or pitch.
-
Long-Term Management: Patients may need to continue voice therapy and regular follow-up visits to ensure that the implant remains in the correct position and that the vocal cords continue to function optimally.
Quality of Life:
-
Improved Voice Function: Most patients experience improved voice strength, clarity, and pitch. Those with vocal cord paralysis typically see a reduction in breathiness and an improvement in vocal endurance.
-
Better Swallowing and Breathing: For individuals who underwent thyroplasty to address swallowing or breathing issues, they will likely notice significant improvements in these functions.
-
Social and Professional Impact: Many individuals find that their quality of life improves significantly following the surgery, as they can communicate more effectively and comfortably, with less worry about aspiration or vocal fatigue.
Top 10 Frequently Asked Questions about Thyroplasty
1. What is thyroplasty?
Thyroplasty is a surgical procedure that is performed to correct vocal cord issues, particularly in cases where the vocal cords are not moving or functioning properly. This procedure is commonly used to treat hoarseness, vocal cord paralysis, or vocal cord atrophy. Thyroplasty involves the implantation of a material or adjusting the position of the thyroid cartilage to improve voice quality and ensure better airflow through the larynx.
2. Why is thyroplasty performed?
Thyroplasty is usually performed for individuals who have:
-
Vocal cord paralysis or paresis (partial paralysis of the vocal cords), often due to nerve damage (e.g., after surgery, injury, or neurological conditions).
-
Vocal cord atrophy (shrinkage or weakness of the vocal cords) that results in breathy voice, difficulty speaking, or difficulty breathing.
-
Breathing difficulties caused by the vocal cords not being able to open wide enough.
-
Voice quality improvement in patients who have poor vocal cord movement, leading to hoarseness or weak voice production.
The procedure is aimed at restoring normal voice function, improving breathing, and enhancing quality of life.
3. What are the different types of thyroplasty?
There are several types of thyroplasty, and the choice depends on the specific vocal cord issue:
-
Type I Thyroplasty (Medialization): This is the most common form, where an implant is placed to push the vocal cord toward the midline, improving voice quality and airflow.
-
Type II Thyroplasty (Lateralization): This procedure is used to move the vocal cord to the side, often used when a vocal cord is paralyzed in a position that restricts airflow.
-
Type III Thyroplasty (Abduction): This type helps open the vocal cords to allow better breathing when the cords are stuck in a closed position.
-
Type IV Thyroplasty (Arytenoid Adduction): A more complex procedure used for severe cases of vocal cord paralysis where the arytenoid cartilage (which controls vocal cord movement) is adjusted.
Each type of thyroplasty is tailored to address specific functional and anatomical issues with the vocal cords.
4. How is thyroplasty performed?
Thyroplasty is typically performed under local anesthesia with sedation, though general anesthesia may be used in some cases. A small incision is made in the neck to access the thyroid cartilage and vocal cords. The surgeon will insert an implant (usually made of a synthetic material or cartilage) into the thyroid cartilage to either push or move the vocal cords into a more favorable position for improved function. The procedure generally takes between 30 to 90 minutes, depending on the complexity of the case.
5. What are the risks and complications of thyroplasty?
As with any surgical procedure, thyroplasty carries certain risks, including:
-
Infection at the incision site.
-
Bleeding or hematoma formation in the neck.
-
Voice changes (although the goal is to improve voice quality, in some cases, the voice may be altered or may worsen temporarily after surgery).
-
Damage to surrounding structures, including the vocal cords or nerves that control the voice.
-
Implant displacement or failure, where the implant may move or cause discomfort.
-
Breathing difficulties due to swelling or other complications affecting the airway.
While the risks are generally low, it is important for patients to discuss potential complications with their surgeon before undergoing the procedure.
6. How long does it take to recover from thyroplasty?
Recovery time for thyroplasty can vary from patient to patient, but most individuals can expect:
-
Short-term recovery: Swelling and discomfort around the neck may last a few days. Pain medication is prescribed for managing discomfort, and many patients can return home the same day or after one night in the hospital.
-
Voice rest: Voice rest is typically required for the first few days to allow the vocal cords to heal. Patients are advised to avoid excessive talking, whispering, or shouting.
-
Follow-up care: Regular follow-up appointments are needed to monitor the healing process, evaluate voice quality, and assess any signs of complications.
-
Full recovery: Most patients experience significant improvement in their voice and breathing within 1-2 months, though complete recovery may take several months for optimal results.
7. Are there any lifestyle changes required after thyroplasty?
After thyroplasty, patients are typically advised to follow specific post-operative instructions:
-
Voice rest: It is crucial to avoid overuse of the voice in the initial recovery phase. Speaking too much or too loudly may cause strain on the healing vocal cords.
-
Avoid strenuous activities: Heavy lifting and vigorous physical activities should be avoided for at least 2 weeks to reduce the risk of complications.
-
Hydration and humidification: Staying hydrated and using a humidifier can help keep the vocal cords moist, aiding in the healing process.
-
Follow-up appointments: Regular check-ups with the surgeon are important to ensure the voice is improving as expected and to monitor for any potential issues such as implant displacement.
8. How successful is thyroplasty?
Thyroplasty has a high success rate, particularly for improving voice quality and addressing breathing difficulties caused by vocal cord paralysis or dysfunction. Success rates can vary depending on the underlying condition, the type of thyroplasty performed, and the patient’s overall health. In general, most patients experience significant improvement in voice clarity, volume, and breath control. However, some patients may need additional procedures or adjustments if they do not achieve the desired result.
9. What are the alternatives to thyroplasty?
For individuals who are not candidates for thyroplasty or prefer non-surgical options, there are several alternatives:
-
Voice therapy: This is often the first step in treating vocal cord issues. A speech-language pathologist (SLP) can guide exercises to strengthen the vocal cords and improve function.
-
Vocal cord injections: In cases of vocal cord paralysis, injections of gel, collagen, or fat can be used to bulk up the affected vocal cord, helping it come into better contact with the other cord for improved voice production.
-
Surgical alternatives: Other surgeries, such as laryngeal framework surgery or recurrent laryngeal nerve surgery, may be considered depending on the condition.
10. What should I expect during the consultation for thyroplasty?
During the consultation, the surgeon will:
-
Review your medical history and any past treatments related to voice or breathing issues.
-
Conduct a physical examination of your neck and throat, and evaluate the function of your vocal cords.
-
Discuss symptoms: You’ll be asked about any issues with your voice, such as hoarseness, breathiness, or difficulty speaking.
-
Diagnostic tests: The surgeon may recommend tests like a laryngoscopy or voice assessment to assess the condition of your vocal cords and determine if thyroplasty is appropriate.
-
Discuss treatment options: The surgeon will explain the potential benefits, risks, and alternatives to thyroplasty, helping you make an informed decision about your treatment.


