Introduction to Total Shoulder Endoprosthesis
The shoulder joint is one of the most mobile - but also one of the most complex - joints in the human body. It is a "ball-and-socket" joint: the head of the upper arm bone (humerus) fits into a shallow socket (the glenoid) of the shoulder blade (scapula). The articulation is cushioned and stabilized by articular cartilage, a synovial lining and the surrounding soft tissues (rotator cuff muscles, tendons, ligaments).
When the protective cartilage is worn out, damaged, or the joint surfaces are destroyed - due to arthritis, trauma, or rotator-cuff related degeneration - the bones may begin to rub against each other, causing pain, stiffness, weakness and loss of function.
Total shoulder endoprosthesis (or total shoulder arthroplasty, TSA) refers to a surgical procedure in which both the "ball" (humeral head) and the "socket" (glenoid) of the shoulder joint are removed and replaced with artificial components (prosthesis), typically made of metal (for the humeral head and stem) and polyethylene/plastic (for the socket lining).
The goal is to relieve pain, restore or improve shoulder mobility and function (range of motion, strength), and enable the patient to perform daily activities that were previously limited by joint damage. Given improvements in surgical techniques and implant design over decades, total shoulder endoprosthesis has become a well-established, effective treatment for end-stage shoulder joint disease.
Depending on the underlying joint condition and soft-tissue status, different prosthetic options may be chosen - standard anatomic total shoulder arthroplasty (when soft tissues like rotator cuff are functional), or alternative designs (e.g. reverse prosthesis) when rotator-cuff muscles are severely damaged.
In this article, we explore in detail why total shoulder endoprosthesis may be recommended; how diagnosis and decision-making proceed; surgical treatment options; risks & complications; postoperative care; and what life looks like after such a surgery.
Causes and Risk Indications for Total Shoulder Endoprosthesis
There are several conditions and risk scenarios which lead to deterioration of the shoulder joint, making total shoulder replacement necessary. Key causes/indications include:
Degenerative (Wear-and-Tear) Arthritis (Osteoarthritis)
-
With aging (or repeated stress), the cartilage lining the ball and socket may gradually wear away, causing bone-on-bone contact, pain, stiffness, reduced motion.
-
Over time, bone spurs, deformity of the joint surfaces and joint space narrowing worsen the mechanical damage and symptoms.
Inflammatory or Rheumatoid Arthritis
-
In conditions where the joint's synovial membrane becomes chronically inflamed (e.g. rheumatoid arthritis), cartilage and bone destruction can occur, eventually damaging both humeral head and glenoid - prompting need for prosthetic replacement.
Post-Traumatic Arthritis / Fractures / Bone Damage
-
Severe fractures of the proximal humerus (upper part of arm bone) - especially ones that are comminuted (multiple fragments) or where bone healing failed - may damage joint surfaces irreparably. In such cases, replacement rather than repair may be indicated.
-
Previous shoulder surgeries, malunions (wrongly healed fractures), or other trauma may cause joint degeneration over time, leading to end-stage disease requiring full replacement.
Rotator Cuff Tear Arthropathy (Ruptured or Irreparable Rotator Cuff)
-
The rotator cuff - a group of muscles/tendons that stabilize the shoulder - is vital for joint mechanics. When these tendons are irreparably torn or degenerated, the joint may become unstable, leading to wear, joint surface damage and arthritis (so-called cuff tear arthropathy).
-
In such scenarios, the shoulder loses its natural stability and normal motion - making conventional TSA less favorable; often surgeons may choose alternative prosthesis (e.g. reverse design) when soft-tissue support is insufficient.
Avascular Necrosis (Osteonecrosis)
-
Conditions that impair blood supply to the humeral head (e.g. steroid use, trauma, certain systemic diseases) can cause bone tissue death; over time, this can collapse the head and lead to joint degeneration - total endoprosthesis may be needed.
Failed Prior Shoulder Surgery or Prosthesis / Revision Cases
-
In some patients, previous shoulder arthroplasty or fracture repair may
fail (implant loosening, wear, infection, deformity), leading to chronic
pain, dysfunction or structural compromise. In those cases, revision
surgery - sometimes full shoulder endoprosthesis - may be
indicated.
When Conservative Treatments Fail
-
Prior to surgery, patients may have undergone non-surgical treatments:
physiotherapy, activity modification, anti-inflammatory drugs, steroid
injections, etc. If these fail to relieve pain or restore function - and
quality of life is severely affected - total shoulder endoprosthesis
becomes a valid option.
In some patients, previous shoulder arthroplasty or fracture repair may fail (implant loosening, wear, infection, deformity), leading to chronic pain, dysfunction or structural compromise. In those cases, revision surgery - sometimes full shoulder endoprosthesis - may be indicated.
Prior to surgery, patients may have undergone non-surgical treatments: physiotherapy, activity modification, anti-inflammatory drugs, steroid injections, etc. If these fail to relieve pain or restore function - and quality of life is severely affected - total shoulder endoprosthesis becomes a valid option.
Key Risk & Indication Summary (when TSA may be considered): severe, persistent pain (often chronic), loss of motion, functional limitation in daily activities (reaching, lifting, dressing), joint damage visible on imaging, failure of non-surgical treatments, and structural joint destruction (cartilage loss, bone damage).
Symptoms and Signs Indicating the Need for Total Shoulder Endoprosthesis
Patients who eventually undergo total shoulder endoprosthesis commonly present with the following signs and symptoms:
-
Chronic shoulder pain, which may worsen with movement, activity, or even at rest / night - interfering with sleep or daily functioning.
-
Stiffness and loss of range of motion - difficulty raising the arm overhead, reaching behind, lifting objects, or performing routine tasks like dressing, combing hair, or carrying items.
-
Weakness or instability - inability to perform strength-demanding arm tasks, or feeling of shoulder "giving way," especially in rotator cuff disease or after prior injuries.
-
Functional impairment affecting quality of life - when the shoulder dysfunction begins to impact daily living, work, sleep, recreation or overall well-being, despite conservative therapies.
-
Visible or radiological changes in joint - imaging (X-ray, MRI) may show cartilage loss, bone spurs, joint space narrowing, humeral head collapse (in avascular necrosis), deformity or deterioration of bone surfaces. These structural changes correlate with symptoms and help confirm severity.
When such signs are persistent and significantly impacting life - and when non-surgical treatments (physiotherapy, medications, injections, rest) have failed - the orthopedic surgeon may recommend total shoulder endoprosthesis as the next step.
Diagnosis and Pre-operative Evaluation for Total Shoulder Endoprosthesis
Deciding on a total shoulder endoprosthesis is a multi-step process involving careful evaluation of the patient's condition, imaging, soft tissue assessment, and overall health. Key aspects include:
Clinical Assessment and History
-
Detailed medical history: duration of symptoms, prior shoulder injuries or surgeries, previous treatments (physiotherapy, medications, injections), general health status, comorbidities (e.g. osteoporosis, inflammatory diseases).
-
Physical examination: assessing shoulder range of motion, strength, stability; checking for pain on movement, rotator cuff integrity, muscle wasting, deformity.
-
Functional assessment: evaluating how shoulder dysfunction affects daily living - e.g. ability to lift, reach, dress, perform household or occupational tasks, sleep quality, pain at rest.
Imaging and Diagnostic Tests
-
X-rays: to check for joint space narrowing, bone spurs, humeral head collapse, glenoid wear, bone deformity - essential to visualize structural joint damage.
-
MRI / CT scan: to assess soft tissue structures (rotator cuff tendons, muscles), bone quality, glenoid bone stock, presence of bone defects - helps decide type of prosthesis (anatomic vs reverse) and surgical plan.
-
Bone quality assessment: especially in older patients or those with osteopenia/osteoporosis - to ensure bone is robust enough for prosthesis fixation (either cemented or press-fit).
-
Soft tissue evaluation: rotator cuff integrity is particularly important. If the rotator cuff is intact (or reparable), anatomic total shoulder arthroplasty may be feasible. If the cuff is irreparable or severely damaged, alternative prosthesis designs (e.g. reverse) may be considered.
Patient Counselling and Shared Decision-Making
Because joint replacement is a major surgery, the surgeon must counsel the patient (and family) about benefits (pain relief, improved mobility), limitations (not full "normal" shoulder in all cases), potential complications (loosening, implant wear, infection), need for rehabilitation, and long-term care.
Preoperative planning includes deciding on prosthesis type (anatomic vs reverse vs hemi vs resurfacing), fixation method (cemented vs uncemented), component size and alignment to match patient's anatomy, and assessment of soft tissue condition - all crucial for long-term success.
Treatment Options & Surgical Techniques: Total Shoulder Endoprosthesis and Variants
Total shoulder endoprosthesis is not a one-size-fits-all; surgeons choose among different prosthetic designs depending on the patient's anatomy, joint damage, and soft-tissue condition. Here are the main options and what they involve:
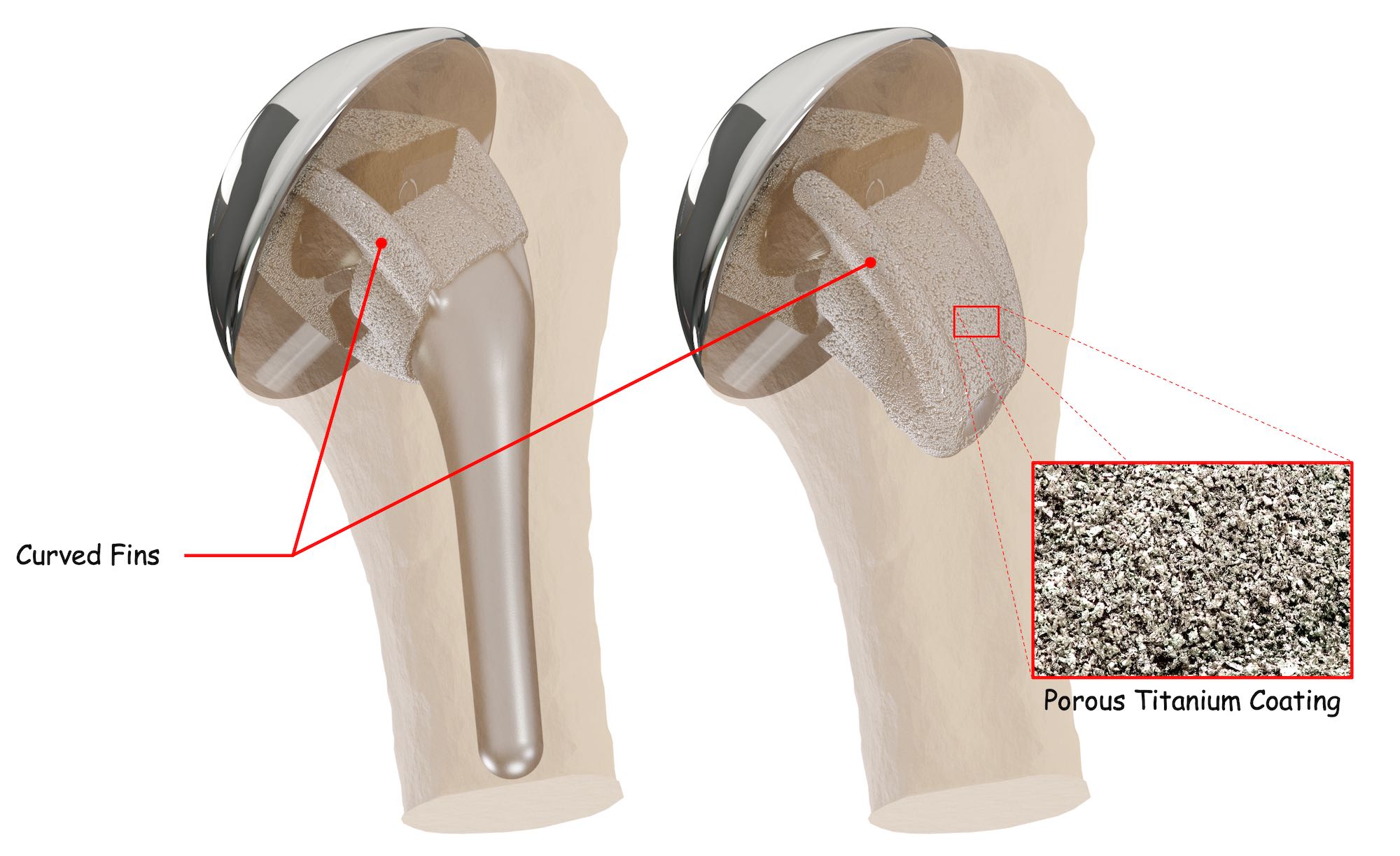
Anatomic Total Shoulder Arthroplasty (TSA)
-
In this "classic" version, both the humeral head ("ball") and the glenoid surface ("socket") are replaced with prosthetic components designed to mimic the natural anatomy. The goal is to replicate normal shoulder mechanics as much as possible.
-
This option typically works best when the rotator cuff is intact or reparable, the glenoid bone stock is adequate, and soft tissues around the shoulder are functional.
-
The humeral component can be cemented or press-fit (uncemented) depending on bone quality; glenoid component often uses a polyethylene liner (plastic) for articulation.
Reverse Total Shoulder Arthroplasty (RTSA)
-
In shoulders where the rotator cuff is irreparably damaged (massive tear, cuff-tear arthropathy), traditional TSA may fail because the joint cannot be stabilized. In such cases, a "reverse" prosthesis is used - the socket and ball are reversed: a "ball" is attached to the scapula (glenoid side) and a "socket" to the humeral side. This design allows the larger deltoid muscle (instead of rotator cuff) to power shoulder movements, restoring functionality and reducing pain.
-
RTSA is especially useful in older patients, patients with complex fractures, rotator-cuff arthropathy, or failed prior shoulder surgery.
Partial Replacement / Hemiarthroplasty / Resurfacing (less commonly "endoprosthesis," but part of spectrum)
-
When only the humeral head is damaged, and the glenoid is relatively preserved, hemiarthroplasty (replacing only the ball) may suffice. However, for end-stage glenoid damage or cartilage loss, hemiarthroplasty may not relieve pain or restore full function - so total replacement remains preferred.
-
Resurfacing techniques (capping the humeral head) are less common, but may be appropriate in certain early or limited disease, especially in younger patients with good bone stock, as a bone-preserving alternative.
Choosing the Right Option
The choice depends on several factors: underlying diagnosis (arthritis, fracture, rotator cuff status), bone quality, patient age, activity level, general health, and patient expectations. Surgeons balance the goals - pain relief, motion, durability - against risks such as prosthesis loosening, glenoid wear, soft-tissue failure, or complication in cuff-deficient shoulders.
In summary: total shoulder endoprosthesis (anatomic TSA) remains a gold standard for degenerative or inflammatory arthritis with intact soft tissues; reverse prosthesis is the go-to for rotator-cuff deficient, complex, or revision cases.
Prevention, Management & Pre-/Post-operative Care for Shoulder Endoprosthesis
While some causes of shoulder joint damage are not preventable (e.g. genetic arthritis, age-related degeneration), certain preventive and management strategies may delay joint deterioration. Moreover, careful peri-operative care and rehabilitation are crucial for successful long-term outcomes after prosthesis.
Pre-operative Management / Preparation
-
Medical/physical evaluation: Assess overall health, bone quality (osteoporosis screening), coexisting conditions (diabetes, infections), nutritional status. Optimize health pre-surgery.
-
Soft tissue and rotator cuff assessment: Imaging (MRI/CT) to evaluate cuff integrity, glenoid bone stock, joint alignment - essential for choosing correct prosthesis design.
-
Patient counselling: Explain surgical options (anatomic vs reverse), expected benefits (pain relief, function), limitations (range of motion, lifting heavy loads), risks (loosening, infection, soft-tissue failure), and rehabilitation timeline.
-
Plan rehabilitation: Arrange physiotherapy post-surgery; patient should understand importance of gradual mobilization, exercises, muscle strengthening, and joint care.
Post-operative Care and Rehabilitation
-
Hospital stay & immediate care: After the surgery, early pain management, wound care, immobilization for some time, monitoring for complications (infection, bleeding, neurovascular status).
-
Physiotherapy & gradual mobilization: Under guidance, start passive motion, then active-assisted exercises, gradually restoring range of motion, strengthening deltoid and periscapular muscles, preserving joint stability, avoiding stress on prosthesis.
-
Activity modification during early healing: Avoid heavy lifting, overhead strenuous activity, sudden jerks, or high-impact sports for a few months - to allow soft tissue healing, prosthesis fixation, and adaptation.
-
Long-term joint care: Maintain sensible load on shoulder; avoid repetitive heavy overhead work; regular follow-up with the orthopedic surgeon to monitor for loosening, wear, or complications.
-
Healthy lifestyle: Good bone health (nutrition, exercise, avoid smoking), muscle strengthening, posture correction, avoiding falls/trauma - all help prolong prosthesis life and maintain function.
Prevention: while full prevention of degenerative shoulder conditions is not always possible, early attention to shoulder pain, rotator cuff tears, injuries, and appropriate management may delay progression to end-stage disease and need for replacement.
Complications and Risks of Total Shoulder Endoprosthesis
As with any major joint replacement, total shoulder endoprosthesis carries potential risks and complications - immediate, early postoperative, and long-term. Important complications include:
Perioperative / Early Risks
-
Infection: As with any implant surgery, risk of surgical-site infection - may necessitate antibiotics, implant removal or revision if severe.
-
Bleeding or hematoma formation - care is needed during surgery and early recovery.
-
Neurovascular injury: Rare, but possible damage to nerves or blood vessels around the shoulder during implant insertion or manipulation.
-
Dislocation or instability: Especially with reverse prosthesis - the altered biomechanics can make dislocation or subluxation more likely than anatomical TSA.
Mid- to Long-Term Complications
-
Prosthesis loosening or wear: Over time, the glenoid (socket) component may loosen or wear out under mechanical stress - earlier designs were more prone to this, though modern implants and cementing techniques have improved longevity.
-
Glenoid bone loss or erosion: In patients with poor bone stock, glenoid component may sink or erode, leading to pain, instability, and need for revision.
-
Soft tissue failure / rotator cuff issues: If rotator cuff is borderline or deteriorates after surgery, motion and stability may be compromised; reverse prosthesis may partly compensate, but limitations in strength or range remain.
-
Periprosthetic fracture: Bone around the prosthesis (humeral stem or socket) may fracture due to trauma, stress, or osteoporosis.
-
Stiffness / restricted range of motion: Especially if post-op physiotherapy is inadequate, or if soft tissues are not flexible, patients may have lingering stiffness despite prosthesis.
-
Need for revision surgery: In some cases - loosening, wear, instability, infection - another surgery may be required to revise or replace the prosthesis.
Thus, while many patients benefit significantly from total shoulder endoprosthesis, success depends on careful patient selection, surgical technique, prosthetic design, and diligent postoperative care.
Living with Total Shoulder Endoprosthesis - Recovery, Rehabilitation & Long-Term Outlook
Undergoing a total shoulder endoprosthesis is life-changing, but with proper management, many patients regain substantial shoulder function, pain relief, and improved quality of life. Here's what to expect in short- and long-term, and how to live with the prosthesis.
Short-Term Recovery Phase (First 3-6 Months)
-
Hospital stay and early healing: Usually a few days post-op, followed by gradual transition to home; initial immobilization and supervised wound care.
-
Physiotherapy and rehabilitation: Gentle passive and assisted movements begin early (as per surgeon/therapist); gradually progress to active exercises; aim to restore range, strength, flexibility, and avoid stiffness or scar contracture.
-
Pain management and comfort: Pain usually decreases over weeks; pain at rest or night often improves markedly compared to pre-surgery; analgesics, ice/heat, gentle movement, and compliance with rehab help.
Medium to Long-Term Functional Outcome
-
Pain relief and daily function: Many patients report dramatic reduction in pain and significant improvement in ability to perform daily tasks - reaching overhead, lifting objects, dressing, grooming, carrying - which had been impossible earlier.
-
Improved mobility and quality of life: Shoulder motion (forward elevation, rotation) often substantially improves; may not reach "pre-disease normal," but enough to enhance independence and comfort.
-
Activity and lifestyle adaptation: Patients need to avoid high-impact sports or heavy overhead labor to preserve implant longevity; gentle to moderate activity, muscle-strengthening, and joint-friendly exercises are encouraged.
Prosthesis Longevity & Follow-Up
-
Modern shoulder prostheses - with improved design and materials - often have good longevity. Long-term studies report favorable outcomes in pain relief and function for many patients with TSA.
-
Regular follow-up (clinical + radiographic) is important to monitor implant integrity, detect early loosening or wear, assess bone quality, and address any soft-tissue issues (rotator cuff, deltoid, etc.).
-
Patient education and compliance - proper posture, safe shoulder use, gradual strengthening, avoiding undue stress - are critical to maintain prosthesis function and avoid complications.
Top 10 Frequently Asked Questions about Total Shoulder Endoprosthesis
1. What is Total Shoulder Endoprosthesis?
Total Shoulder Endoprosthesis, also referred to as Total Shoulder Replacement, is a surgical procedure in which a damaged or diseased shoulder joint is replaced with an artificial implant (prosthesis). The shoulder is a ball-and-socket joint, with the ball (head of the upper arm bone or humerus) fitting into the socket (glenoid part of the shoulder blade). In patients suffering from arthritis, injury, or degeneration of the joint, the cartilage that cushions the bones wears out, leading to pain, stiffness, and loss of function. The procedure involves removing the damaged parts of the shoulder and replacing them with metal and plastic components to restore function, alleviate pain, and improve the range of motion.
2. Why is shoulder endoprosthesis needed - what conditions indicate it?
Shoulder endoprosthesis is typically recommended when other non-surgical treatments like medication, physical therapy, or injections fail to alleviate pain, and the shoulder's function is significantly compromised. Common conditions that indicate the need for total shoulder replacement include:
-
Osteoarthritis: Degenerative joint disease causing wear and tear of the cartilage.
-
Rheumatoid arthritis: An inflammatory disease that causes pain and swelling in the shoulder joint.
-
Post-traumatic arthritis: Arthritis that develops after a shoulder injury or fracture.
-
Severe shoulder fractures: Where the bones are shattered, or the joint is severely damaged.
-
Rotator cuff tears: If the rotator cuff (group of muscles and tendons that stabilize the shoulder) is severely torn and cannot be repaired.
The procedure is often recommended when these conditions cause persistent pain, reduce the ability to perform everyday activities, or affect sleep.
3. How is the surgery performed? What does the procedure involve?
Total shoulder endoprosthesis surgery is typically performed under general anesthesia, ensuring the patient is fully asleep during the procedure. The surgeon makes an incision in the shoulder area to access the joint. The damaged ball (humeral head) and socket (glenoid) are removed. The humeral head is replaced with a metal ball, and the glenoid is replaced with a plastic socket. The surgeon may use cement or a press-fit technique to secure the implants in place, depending on the patient's bone quality. The incision is then closed with sutures, and the shoulder is usually placed in a sling to immobilize it and facilitate healing.
4. What is the expected recovery time and what does rehabilitation look like?
The recovery from total shoulder replacement varies, but generally, patients can expect the following:
-
Hospital Stay: Most patients stay in the hospital for 1-2 days post-surgery for pain management and initial recovery.
-
Pain Management: Pain is typically managed through medication, including analgesics and anti-inflammatory drugs. Cold therapy (ice packs) may be used to reduce swelling and discomfort.
-
Physical Therapy: Rehabilitation begins soon after surgery. In the early stages, passive range-of-motion exercises are performed under the guidance of a physical therapist. As recovery progresses, strengthening exercises are added to help rebuild muscle strength around the shoulder.
-
Return to Normal Activities: Most patients can return to light daily activities within 4-6 weeks, but it may take up to 3-6 months to return to full range of motion and strength. Strenuous physical activities should be avoided for up to 6 months or as advised by the surgeon.
5. What improvements can a patient expect after shoulder replacement?
After recovering from total shoulder replacement, most patients experience significant improvement in their ability to perform daily activities and a reduction in pain. Some of the expected benefits include:
-
Pain Relief: Most patients experience a dramatic reduction in pain, especially if shoulder pain had previously interfered with daily activities, sleep, or work.
-
Increased Mobility: The range of motion of the shoulder improves, allowing patients to resume activities such as reaching overhead, dressing, driving, or lifting.
-
Improved Function: Tasks that were once difficult or impossible, such as lifting objects or combing hair, can become easier.
-
Enhanced Quality of Life: Overall, shoulder replacement can lead to a significantly improved quality of life by reducing pain and enhancing function.
6. What are the risks and possible complications of total shoulder endoprosthesis?
While total shoulder replacement is a generally safe procedure, it comes with potential risks and complications:
-
Infection: Infections can occur at the surgical site, and antibiotics are administered to reduce this risk. Any signs of infection (such as increased redness, swelling, or fever) should be reported to the surgeon immediately.
-
Bleeding: Some bleeding is normal, but excessive bleeding can lead to complications and may require medical attention.
-
Implant Wear or Loosening: Over time, the shoulder implant may loosen or wear out, which could require revision surgery.
-
Nerve or Blood Vessel Injury: During the procedure, there is a small risk of damage to nearby nerves or blood vessels, which could affect shoulder function or cause numbness.
-
Stiffness or Reduced Mobility: While most patients regain significant mobility, some may experience stiffness or limited range of motion, which can be improved through physical therapy.
-
Blood Clots: Deep vein thrombosis (DVT) or other blood clots may develop post-surgery, but this risk is minimized with preventive measures like early movement and blood thinners.
7. Who is a good candidate for total shoulder endoprosthesis - and who is not?
The ideal candidate for total shoulder replacement is someone who:
-
Suffers from severe pain and limited function due to arthritis or joint degeneration.
-
Has tried non-surgical treatments (like physical therapy, medications) with little or no relief.
-
Is in generally good health and able to undergo surgery and rehabilitation.
Patients who may not be ideal candidates include: -
Those with significant rotator cuff damage or muscle dysfunction around the shoulder, as this can affect the stability and function of the implant.
-
Individuals with poor bone quality, such as those with osteoporosis, who may not provide sufficient support for the implant.
-
Patients who have systemic health issues (like uncontrolled diabetes or active infections) that could complicate the healing process.
8. How long does the shoulder prosthesis last - will I need another surgery in future?
The lifespan of a shoulder prosthesis depends on factors such as the patient's age, activity level, and overall health. In general, modern shoulder implants last between 15-20 years, but younger, more active individuals may require a revision surgery sooner. Regular follow-up visits with your orthopedic surgeon are essential to monitor the health of the prosthesis and ensure it remains secure. If the implant wears out or loosens over time, a revision surgery may be necessary to replace or adjust the implant.
9. What should patients expect immediately after surgery (hospital stay and early post-op care)?
Immediately following surgery:
-
Patients are typically monitored in the hospital for 1-2 days to ensure proper pain management, monitor for complications, and start basic physical therapy exercises.
-
The shoulder will be placed in a sling for protection, and the patient will be given instructions for pain relief and care of the surgical site.
-
Antibiotics may be administered to prevent infection.
-
Initial rehabilitation starts with gentle motion exercises to prevent stiffness.
-
A follow-up appointment is scheduled within 1-2 weeks to check the incision site and assess progress.
10. What lifestyle changes and precautions will I need after total shoulder endoprosthesis?
After surgery, it is important to:
-
Follow physical therapy: Regular physical therapy is crucial for restoring mobility, strength, and function to the shoulder. The patient should adhere to prescribed exercises and attend all therapy sessions.
-
Avoid heavy lifting: For the first few months after surgery, patients should avoid lifting heavy objects or performing activities that may put excessive strain on the shoulder.
-
Maintain a healthy weight: Being overweight can place additional stress on the shoulder joint and impact the longevity of the implant.
-
Protect the shoulder: Patients should be cautious during physical activities and avoid actions that might result in falls or injury to the shoulder.
-
Attend follow-up visits: Regular follow-ups with the surgeon are important for monitoring the implant and ensuring the shoulder is healing properly.


