Introduction to Transurethral Resection of Bladder Tumor (TURBT)
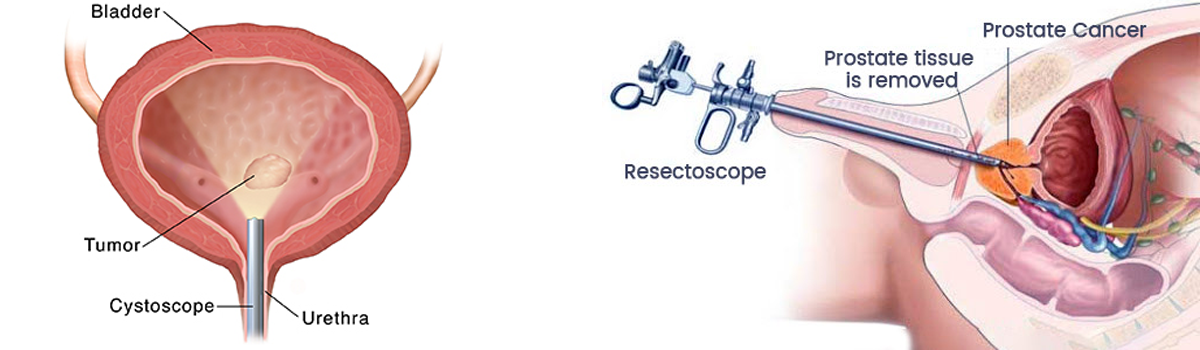
The bladder is a hollow, muscular organ that stores urine before it's passed out through the urethra. Sometimes, abnormal tissue growths or tumors develop on the inner lining of the bladder. When such growths are suspected - especially when tests indicate possible cancer - a procedure called Transurethral Resection of Bladder Tumor (TURBT) is used. TURBT is both a diagnostic and a therapeutic procedure.
In a TURBT, a surgeon inserts a slender, specialized instrument called a resectoscope (similar to a cystoscope) through the urethra - without any external incision. This scope has a light, camera, and a wire loop (or sometimes laser) at its tip. While visualizing the bladder interior, the surgeon uses the loop (or laser) to remove (resect) any visible tumors, or take biopsies for pathological analysis.
TURBT remains the cornerstone of bladder tumor management - especially for bladder cancers that are confined to the inner lining or superficial layers (non-muscle-invasive). It helps establish diagnosis (type and grade of tumor), determine extent (stage), and where suitable, remove the tumor entirely, offering a chance for cure while preserving the bladder.
Given its dual role - diagnosis and treatment - TURBT plays a critical role in the management pathway of bladder cancer, often as the first-line surgical intervention.
Causes and Indications for TURBT
TURBT isn't performed arbitrarily - it's indicated when there's a suspicion (or confirmation) of a bladder tumor. The main scenarios/causes that lead to TURBT include:
-
Detection of a bladder lesion or tumor on imaging or cystoscopy: Sometimes during evaluation for hematuria (blood in urine), urinary symptoms, or incidentally, a lesion is seen in the bladder. TURBT is indicated to biopsy or remove that lesion.
-
Suspected or confirmed non-muscle-invasive bladder cancer (NMIBC): For tumors confined to the inner lining or mucosal layer of bladder (not yet invaded muscle), TURBT is the mainstay treatment.
-
Biopsy to confirm tumor type and stage (diagnosis): TURBT enables obtaining sufficient tissue (including muscle if possible) so pathologists can assess grade, depth (stage), presence of carcinoma in situ (CIS), or aggressive variants. This is critical for planning further treatment.
-
Therapeutic removal of visible tumors: For small or superficial tumors, TURBT may completely excise them, offering a bladder-preserving treatment instead of more radical surgery.
-
Repeated TURBT (Second-look) in high-risk cases: In certain cases - e.g. high-grade tumors, incomplete first resection, or tumors with high risk of recurrence - a second TURBT may be done to ensure complete resection, accurate staging, and minimize recurrence.
Thus, TURBT is indicated whenever there is abnormal bladder lesion (benign or malignant), or bladder cancer suspected/diagnosed - especially when disease is non-muscle-invasive or limited and bladder preservation is possible.
Symptoms and Signs That May Lead to TURBT
Patients undergo evaluation leading to TURBT usually because of certain symptoms, signs or incidental findings that suggest bladder pathology. Common triggers include:
-
Hematuria (Blood in Urine): One of the most common presenting complaints. Blood may be visible (gross hematuria) or microscopic (found on urine tests). This prompts imaging or cystoscopy, and eventual TURBT if a lesion is found.
-
Lower urinary tract symptoms (LUTS): Irritative symptoms such as frequent urination, urgency, burning or pain during urination, or difficulty urinating may occur - especially if a tumor irritates bladder lining.
-
Recurrent urinary tract infections (UTIs): Especially if infections are unexplained or do not respond well to therapy - a bladder lesion/tumor may underlie recurrent infections.
-
Abnormal bladder imaging or incidentally found lesion: Sometimes during imaging for other reasons (ultrasound, CT scan), a mass or suspicious area in bladder may be detected. That will lead to cystoscopy and potentially TURBT.
-
Surveillance (In patients with history): In patients with prior bladder cancer (even after TURBT), routine follow-up cystoscopies may detect recurrence or new tumors. These lesions are managed again with TURBT, making repeat resections common in long-term management.
Because bladder cancer (especially early stages) may not produce severe symptoms, sometimes TURBT is performed based on microscopic hematuria or incidental findings - underscoring the importance of timely evaluation.
Diagnosis: How TURBT Helps Confirm Bladder Tumor and Stage Disease
Before TURBT, patients undergo a diagnostic work-up - imaging (ultrasound, CT scan), urine cytology, cystoscopy - that may suggest a bladder lesion. However, TURBT plays a crucial role in definitive diagnosis and staging of bladder tumors. Here's how:
-
Visual identification and removal/biopsy: Through a resectoscope inserted via urethra, the surgeon directly visualizes any bladder lesion(s). Suspicious tissue is resected or biopsied.
-
Histopathological examination: The resected tissue is sent to pathology to determine: tumor type (urothelial carcinoma or other), grade (how abnormal cells look), presence of carcinoma in situ (CIS), and whether muscle tissue was included. Inclusion of bladder muscle (detrusor) in biopsy is essential - absence may lead to under-staging.
-
Staging (depth of invasion): Pathology report after TURBT reveals whether tumor is limited to mucosa/submucosa (non-muscle-invasive) or has invaded muscle - which determines further treatment strategy (less aggressive vs more radical).
-
Guiding treatment and follow-up plan: Based on stage, grade, margins, and pathological features (e.g. CIS, lymphovascular involvement), oncologists / urologists decide whether TURBT alone suffices, or additional therapy (intravesical therapy, re-resection, cystectomy) is needed.
In short: TURBT is not just a removal procedure - it is the diagnostic foundation of bladder cancer management. Without TURBT (or equivalent), staging and planning any effective treatment is impossible.
Treatment Options During TURBT & Variants: How TURBT is Performed and What Comes Next
While TURBT refers broadly to transurethral resection of bladder tumor, there are variations in technique, technology, and follow-up strategies. Over time, these have evolved to improve effectiveness, reduce recurrence, and minimize complications.
Classic TURBT (Monopolar or Bipolar resection)
-
Using a resectoscope with a wire loop and electrocautery (monopolar or bipolar), the surgeon removes visible tumor tissue from bladder lining. The resection may include part of underlying tissue (submucosa, sometimes muscle) to ensure deep enough sampling.
-
After resection, a catheter may be placed to drain urine; often a single postoperative dose of intravesical chemotherapy (e.g. mitomycin) is given soon after TURBT to kill residual cancer cells and reduce recurrence risk.
Advanced / Improved Techniques: En Bloc Resection, Imaging-Assisted TURBT
Because conventional TURBT can sometimes remove tumors in pieces (fragmented), which may leave residual cells or make pathologic staging difficult, newer techniques have emerged:
-
En Bloc Resection of Bladder Tumor (ERBT): The entire tumor is removed in one piece rather than multiple fragments. This improves pathological assessment (tumor margins, depth), reduces tumor seeding risk, and may reduce recurrence rates.
-
Use of enhanced imaging (e.g. photodynamic diagnosis, narrow-band imaging, blue-light cystoscopy): These tools help detect flat lesions (like carcinoma in situ), small satellite tumors or residual disease that may be missed under white light. This enhances completeness of resection and lowers recurrence risk.
-
Laser resection or ablation techniques: In some centers, lasers (e.g. Holmium, Thulium) are used instead of electrocautery loops to resect tumors - these may offer better tissue preservation, less bleeding, and faster recovery in select cases.
Follow-Up and Further Treatment After TURBT
-
Intravesical therapy: After TURBT, many patients (depending on risk) receive intravesical therapies (chemotherapy or immunotherapy) to reduce recurrence - especially when tumors are high-grade or multiple.
-
Second (re-)TURBT (re-resection): For high-risk tumors or when initial resection is incomplete / lacks muscle in specimen, guidelines recommend a second TURBT within 4-6 weeks to ensure complete removal and accurate staging.
-
Surveillance (Cystoscopic follow-up): Since bladder cancer (even non-muscle-invasive) has significant risk of recurrence, lifelong follow-up with periodic cystoscopy and urine cytology is required after TURBT to detect and treat recurrences early.
Thus, TURBT is often the first step - but long-term management involves intravesical therapies, possible re-resections, and regular surveillance, especially for high-risk patients.
Prevention and Management: What Patients and Providers Should Know
Since bladder cancer - and thus TURBT - arises from multiple risk factors, prevention (primary and secondary) and good management are important. While not all bladder tumors can be prevented, certain strategies may reduce risk, improve outcomes, or reduce recurrence.
Risk Reduction & Prevention (Primary / Secondary)
-
Avoid known risk factors: Tobacco smoking is a major risk factor for bladder cancer; quitting smoking significantly reduces risk. Occupational exposure to certain chemicals or dyes is also linked - appropriate protective measures are essential.
-
Good hydration and urinary hygiene: Maintain adequate fluid intake to flush the urinary tract regularly.
-
Prompt evaluation of urinary symptoms: Hematuria (even microscopic), recurrent infections, irritative urinary symptoms - should be evaluated promptly. Early detection of bladder lesions increases chance of successful TURBT and bladder preservation.
-
Follow-up & surveillance after initial TURBT: Even after successful resection, because recurrence risk is high, regular cystoscopy and check-ups are essential to catch recurrence early.
Peri-Operative Management & Best Practices for TURBT
-
Ensure complete resection (quality TURBT): Surgeon's experience, inclusion of detrusor muscle in biopsy specimen, careful mapping of tumor base, use of enhanced imaging when needed - all contribute to high-quality TURBT, reducing recurrence and improving staging accuracy.
-
Use of modern techniques (ERBT, laser, imaging-assisted cystoscopy): Where available, these improve resection quality, minimize complications, and reduce recurrence risk.
-
Adjuvant intravesical therapy (when indicated): For high-risk tumors - use of intravesical chemotherapy or immunotherapy post-TURBT helps reduce recurrence and progression risk.
Complications and Risks of TURBT
Though TURBT is a relatively common urological procedure and often considered minimally invasive (since it avoids external incisions), it is not risk-free. Complications can arise, and patients must be counselled accordingly.
Common / Early Complications
-
Hematuria (blood in urine): This is the most frequent post-operative effect - many patients may see blood in urine for days after TURBT. In some cases, bleeding may be significant requiring bladder irrigation or re-intervention.
-
Urinary symptoms: Burning on urination, frequency, urgency, discomfort - transient irritative symptoms are common after TURBT.
-
Urinary tract infection (UTI): Because the bladder and urinary tract are instrumented, there is a risk of infection post-surgery, especially if catheterization is required.
Less Common / Serious Risks
-
Bladder perforation: During resection, especially with deep resection or for large tumors, there is risk of bladder wall perforation, leading to leakage of fluid (or urine), possible extravasation, peritonitis, or tumor seeding.
-
Need for repeat surgery / resection (re-TURBT): If initial resection incomplete, or pathologic specimen lacks muscle, a second TURBT may be required, increasing risk cumulatively.
-
Recurrence or progression of cancer: Even after TURBT, bladder cancer has a high recurrence rate; incomplete resection or aggressive tumor biology may lead to recurrence or progression (to muscle-invasive disease).
-
Clot retention / urinary obstruction: Blood clots in bladder may block urine flow; catheterization or irrigation may be needed.
-
Complications related to anesthesia or procedure - e.g. cardiovascular events, especially in high-risk patients: though uncommon, always a possibility.
Studies have reported that TURBT complication rates vary (somewhere around 5-20% depending on tumor size, patient factors, surgeon experience) for minor-to-moderate complications.
Given these risks, TURBT - though minimally invasive - must be done with care, and patients must receive good perioperative counselling, follow-up, and bladder care after surgery.
Living with the Condition After TURBT - Recovery, Follow-Up & Long-Term Outlook
Because TURBT is often part of a longer-term management plan for bladder cancer (not a one-time treatment), life after TURBT involves recovery, follow-up, surveillance, and possibly further treatments. Below is what patients can expect, and how to live with the “post-TURBT condition.”
Immediate Recovery
-
Many TURBTs are done as day-surgery or short-stay procedures. The patient may go home the same day or stay overnight depending on tumor size, bleeding risk, and overall status.
-
After surgery, a urinary catheter may be placed for a short period to allow bladder drainage and healing; once removed, patient starts normal urination gradually.
-
Expect blood in urine, discomfort/dysuria, mild urinary frequency or burning for few days - this is common. Adequate fluid intake, rest, mild pain relief, and avoidance of strenuous activity help recovery.
Short-term Follow-up and Bladder Care
-
Patient should avoid irritants: smoking, alcohol, certain foods/spicy diets, and ensure good hydration - helps healing and reduces bladder irritation.
-
Routine check-up with urologist to assess healing, check for complications (bleeding, infection), and discuss pathology results (tumor grade, depth, margins).
-
If intravesical therapy is recommended (e.g. chemotherapy, immunotherapy), patient will start as per protocol. This helps reduce recurrence risk.
Long-Term Management & Surveillance
-
Because bladder cancer - especially non-muscle-invasive - has high rates of recurrence, lifelong surveillance is often required. Periodic cystoscopy, urine cytology, imaging or biomarkers may be used to detect recurrence early.
-
If recurrence happens, repeated TURBT, intravesical therapy, or in some cases more radical surgery (e.g. partial or total cystectomy) may be considered, based on tumor behavior.
-
For patients, this means commitment - regular follow-up visits, possible repeated procedures, consistent bladder monitoring. While this may feel onerous, it's vital for long-term disease control and survival.
Quality of Life After TURBT
-
Bladder preservation and normal life: One of the major advantages of TURBT (vs radical bladder removal) is that the bladder is preserved, allowing near-normal urinary function and quality of life.
-
Psychological impact: Dealing with cancer diagnosis, repeated surveillance, anxiety about recurrence - emotional and psychological support (family, counselling, support groups) may be essential for holistic care.
-
Healthy lifestyle and risk awareness: Avoiding known risk factors (smoking, exposure to toxins), maintaining hydration, regular medical checkups, being alert to urinary symptoms - all help long-term wellness.
Top 10 Frequently Asked Questions about Transurethral Resection of Bladder Tumor (TURBT)
1. What is Transurethral Resection of Bladder Tumor (TURBT)?
Transurethral Resection of Bladder Tumor (TURBT) is a minimally invasive surgical procedure used to remove tumors from the bladder. The procedure involves inserting a cystoscope (a thin, flexible tube with a light and camera) through the urethra (the tube that carries urine from the bladder out of the body) to reach the bladder. Using specialized tools, the surgeon can cut or vaporize the tumor tissue. The advantage of TURBT is that it doesn't require any external incisions, as the procedure is performed entirely through the urethra, making it less invasive and promoting a quicker recovery. The tissue that is removed is sent to a laboratory for biopsy to check if the tumor is cancerous, as well as to evaluate the stage and grade of the tumor.
2. Why is TURBT performed?
TURBT is typically performed when there is suspicion or confirmation of bladder cancer, especially for non-muscle invasive bladder cancer (NMIBC). It is used to:
-
Remove tumors in the bladder, particularly when they are superficial (only affecting the inner lining) and have not invaded deeper tissue.
-
Diagnose and stage cancer by removing tissue for examination, allowing the doctor to assess the extent of cancer and guide further treatment options.
-
Treat symptoms like blood in the urine, frequent urination, or difficulty urinating caused by bladder tumors.
-
Resect bladder tumors that could lead to infection or further complications if left untreated.
TURBT is often the first treatment for bladder tumors, especially when cancer is confined to the bladder lining.
3. How is TURBT performed? What happens during surgery?
During TURBT, the patient is typically given general anesthesia or spinal anesthesia to numb the lower body. A cystoscope is inserted into the urethra, allowing the surgeon to see the bladder and locate the tumor. Specialized surgical tools are then passed through the cystoscope to remove the tumor. The surgeon may use a resectoscope with an electrified loop to cut and cauterize (seal) the tumor, which helps to control bleeding. The tumor is then removed in small pieces. The surgery usually lasts between 30 to 90 minutes, depending on the tumor's size and location. Afterward, a catheter is placed in the bladder to allow for urine drainage, and patients are typically monitored in the hospital for a short period before being discharged.
4. What are the risks and complications of TURBT?
Like any surgical procedure, TURBT carries risks, although complications are rare:
-
Bleeding: This is the most common complication, and some blood in the urine is expected after surgery. In some cases, bleeding may be more significant and require medical intervention.
-
Infection: There is a small risk of infection in the urinary tract after the procedure, which may require antibiotics.
-
Urinary retention: In some cases, patients may experience difficulty urinating after surgery, requiring temporary catheterization.
-
Bladder perforation: Although rare, there is a risk of puncturing the bladder during surgery, which may require additional treatment.
-
Irritative symptoms: Some patients experience discomfort, burning sensations during urination, or frequent urination in the days following surgery.
-
Tumor recurrence: Even after TURBT, bladder tumors may recur, which is why follow-up cystoscopies are necessary for ongoing monitoring.
5. What is the recovery process like after TURBT?
Recovery after TURBT is generally quick because it is minimally invasive. However, some discomfort is to be expected in the first few days:
-
Pain management: Mild discomfort, burning sensation while urinating, and some blood in the urine are common post-procedure. These symptoms usually subside within a few days. Pain relievers or anti-inflammatory medications are often prescribed.
-
Urinary changes: Temporary changes in urination, such as frequent urges or a burning sensation, may occur for several days.
-
Catheter: A catheter is typically left in place for 1-2 days after surgery to help drain the bladder and allow the area to heal.
-
Follow-up care: The patient will need to follow up with their doctor for further cystoscopies and imaging tests to monitor for recurrence of tumors.
Full recovery generally takes 1-2 weeks, with most patients able to return to normal activities after about a week. Physical activities or heavy lifting should be avoided for at least 2-3 weeks to ensure proper healing.
6. What are the possible side effects or complications after TURBT?
While TURBT is generally safe, there are potential side effects or complications:
-
Post-operative bleeding: Some blood in the urine is common, but heavy or prolonged bleeding may require medical attention.
-
Infection: A urinary tract infection (UTI) may occur, which may require antibiotics.
-
Bladder spasms: After the procedure, some patients experience bladder spasms, which can be painful and may cause difficulty urinating.
-
Urinary retention: In some cases, patients may have difficulty urinating after the procedure, which may require a catheter for a longer period.
-
Scarring: Scar tissue may form at the site of tumor removal, leading to urinary blockages or other issues that might require additional treatment.
7. What can I expect during the first few days after TURBT?
The first few days after TURBT may involve some discomfort and post-operative symptoms:
-
Blood in urine: It is normal to have some blood in the urine after surgery. This should gradually decrease as the healing process progresses.
-
Pain or burning sensation: Patients may experience mild pain or a burning sensation while urinating, which typically resolves within a few days.
-
Frequent urination: The bladder may be sensitive post-surgery, causing the urge to urinate frequently. Drinking plenty of water can help reduce discomfort.
-
Follow-up: The patient will be advised to attend follow-up appointments for monitoring and further testing, such as another cystoscopy, to ensure that the bladder has healed and that no tumor remains.
8. How soon can I resume normal activities after TURBT?
Most patients can return to light daily activities within 1-2 weeks. However, patients are advised to:
-
Avoid strenuous activities: Physical exertion, heavy lifting, and activities that put pressure on the abdomen or bladder should be avoided for about 4-6 weeks.
-
Gradual return: Light activities such as walking and basic tasks can generally be resumed a few days after surgery, but patients should follow the advice of their doctor and physical therapist.
9. Will I need further treatment after TURBT?
After TURBT, additional treatments may be required, depending on the pathology of the tumor:
-
Intravesical therapy: If the tumor is high-grade or has a high risk of recurrence, the patient may receive chemotherapy or immunotherapy directly into the bladder to reduce the risk of tumor regrowth.
-
Second TURBT: In some cases, a second TURBT is recommended to remove any remaining cancerous tissue or to ensure that the tumor has been completely excised.
-
Monitoring: Even if the surgery is successful, regular cystoscopies are needed for ongoing surveillance of the bladder to check for recurrence, as bladder tumors have a tendency to come back.
10. What is the long-term prognosis after TURBT?
The long-term prognosis after TURBT depends on several factors, including the type, stage, and grade of the tumor, as well as the patient's overall health.
-
Non-invasive tumors: If the tumor was non-muscle-invasive and fully resected, the prognosis is generally good, though regular follow-up is required to monitor for recurrence.
-
Higher-grade or invasive tumors: If the tumor was high-grade or invasive, additional treatments may be necessary, and the risk of recurrence is higher. In such cases, further therapy such as chemotherapy, immunotherapy, or even more invasive surgeries may be required.
-
Survival rates: Bladder cancer has a relatively high survival rate when detected early, and TURBT is a crucial step in managing non-muscle-invasive bladder cancer. Regular follow-ups are essential to detect any recurrence early and to prevent the cancer from spreading.


