Introduction to Ureterovesical Fistula
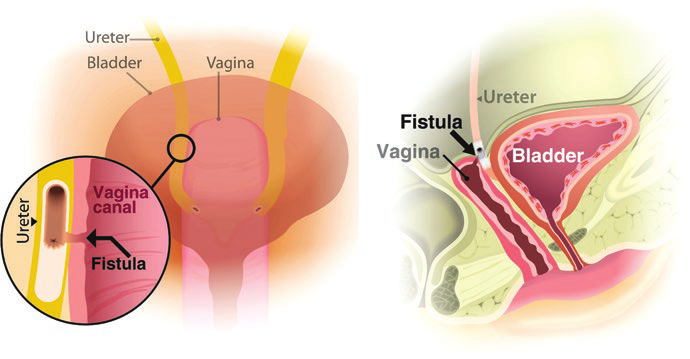
A ureterovesical fistula (UVF) is a rare but significant condition in which an abnormal passage forms between the ureter and the bladder. The ureter is responsible for carrying urine from the kidneys to the bladder, and the bladder stores urine until it is excreted from the body. When a fistula occurs, the normal flow of urine is disrupted, and the urine may leak from the ureter into the bladder in an unintended and abnormal manner. This abnormal connection allows urine to bypass its normal pathway, leading to potential complications such as urinary incontinence, urinary tract infections, kidney damage, and decreased renal function.
Ureterovesical fistulas can be acquired through trauma, surgical complications, infections, radiation therapy, or inflammatory diseases. These fistulas often arise after surgery on the pelvic organs, such as hysterectomy, prostatectomy, or bladder surgery. As the fistula disrupts the normal flow of urine, the patient may experience a variety of symptoms, including leakage, pain, recurrent infections, and kidney dysfunction.
The clinical significance of ureterovesical fistulas lies in their potential for long-term renal damage and chronic discomfort. If left untreated, these fistulas can lead to hydronephrosis (swelling of the kidney due to urine buildup) and renal failure. Timely intervention through surgical repair is essential to restore normal urinary function, prevent further kidney damage, and improve the patient's quality of life.
Causes and Risk Factors of Ureterovesical Fistula
Understanding the causes and risk factors of ureterovesical fistulas is key to preventing and managing the condition. A variety of underlying factors contribute to the formation of these fistulas, from surgical complications to diseases or trauma.
Common Causes of Ureterovesical Fistulas
-
Post-Surgical Injury
The most common cause of ureterovesical fistulas is iatrogenic injury, which refers to injury caused during medical or surgical procedures. Pelvic surgeries, including those for gynecological (e.g., hysterectomy), urological (e.g., prostatectomy, cystectomy), or colorectal surgeries, can inadvertently damage the ureter or bladder, leading to the formation of a fistula. These injuries are often due to surgical dissection or the inadvertent cutting or clipping of the ureter during an operation.-
Gynecological Surgeries: Ureterovesical fistulas are frequently seen as a complication of hysterectomies or pelvic surgeries that involve removal or dissection of nearby tissues.
-
Urological Surgeries: Procedures like prostatectomy (removal of the prostate) or cystectomy (removal of the bladder) often require careful attention to the ureters and can lead to inadvertent injury, especially when tissues are scarred or altered by prior surgery.
-
-
Radiation Therapy
Radiation therapy, particularly pelvic radiation, is a known risk factor for developing ureterovesical fistulas. The radiation used to treat pelvic cancers (such as prostate, cervical, bladder, or rectal cancers) can cause fibrosis and damage to the ureter or bladder wall, leading to the development of fistulas. Radiation-induced changes in tissue elasticity can weaken the structure of these organs, making them more prone to abnormal connections. -
Trauma or Injury
Trauma, including blunt force or penetrating injuries, can lead to ureterovesical fistulas. This is most commonly seen in motor vehicle accidents, falls, or any physical injury to the pelvic area that damages the bladder or ureters. Penetrating injuries such as gunshot wounds or stabbings can also cause immediate damage to these organs, creating a fistula between the ureter and the bladder. -
Malignancy (Cancer)
Cancers of the pelvic organs — such as bladder cancer, cervical cancer, prostate cancer, or colorectal cancer — can invade the surrounding tissues and cause erosion of the ureter or bladder wall. As the tumor grows, it may create an abnormal tract between the ureter and the bladder. Pelvic cancers often require chemotherapy or radiation therapy, both of which can contribute to the formation of fistulas due to the damage they cause to healthy tissues. -
Chronic Inflammatory Conditions
Inflammatory conditions, such as pelvic inflammatory disease (PID), inflammatory bowel disease (IBD), or chronic cystitis, can result in scarring and tissue damage in the pelvic region. When the tissue integrity of the bladder or ureter is compromised by chronic inflammation, the likelihood of fistula formation increases. -
Urinary Tract Infections (UTIs)
Chronic UTIs, particularly when left untreated, can lead to persistent inflammation and infection of the urinary tract. Over time, this can cause tissue breakdown and may result in the formation of a fistula between the ureter and bladder.
Risk Factors for Developing Ureterovesical Fistulas
-
Previous Pelvic Surgery
Patients who have undergone pelvic surgeries, particularly those involving the urinary tract, are at higher risk for developing ureterovesical fistulas due to potential injury during the procedure. -
Radiation Exposure
Pelvic radiation therapy increases the risk of ureterovesical fistulas due to the long-term effects of radiation on the surrounding tissue. The ureters and bladder can become weak and less elastic, making them more vulnerable to developing fistulas. -
Chronic Inflammatory Diseases
Individuals with chronic inflammatory diseases affecting the pelvic organs, such as IBD or chronic cystitis, are more prone to developing fistulas due to the ongoing damage caused by inflammation. -
Cancer Treatment (Radiation/Chemotherapy)
Cancer treatment, particularly in the pelvic region, is another risk factor. Chemotherapy and radiation therapy can weaken the bladder and ureter walls, increasing the likelihood of fistula formation. -
Trauma or Injury
Physical trauma, such as motor vehicle accidents or falls, that causes damage to the pelvic area increases the risk of ureterovesical fistulas.
Symptoms and Clinical Presentation of Ureterovesical Fistula
The symptoms of a ureterovesical fistula can vary depending on the size, location, and cause of the fistula. The most common symptoms include urinary leakage, infections, and pain. In some cases, patients may experience recurrent UTIs, hydronephrosis, or flank pain. Here are the most frequent signs and symptoms:
Key Symptoms
-
Urinary Leakage or Incontinence
-
One of the most noticeable symptoms is urinary leakage or incontinence. Patients may notice that urine leaks from the bladder at abnormal times, such as when not urinating. The leakage can occur continuously or intermittently, depending on the size of the fistula.
-
-
Flank Pain
-
Many individuals with a ureterovesical fistula experience flank pain due to pressure buildup in the kidney or ureter. This is often a result of hydronephrosis, where the kidney becomes swollen due to urine backup. The pain can be sharp or dull and may worsen over time.
-
-
Recurrent Urinary Tract Infections (UTIs)
-
Chronic UTIs are common with ureterovesical fistulas because of the abnormal urinary flow, which can lead to urine stagnation and infection. These infections can cause painful urination, cloudy or foul-smelling urine, and fever.
-
-
Blood in the Urine (Hematuria)
-
Some patients may notice blood in their urine, which can be a result of the fistula or the associated infection. This may present as visible blood or only detectable through a urine test.
-
-
Kidney Dysfunction
-
Kidney damage can result if the fistula is left untreated for a long time. Urine leakage into the surrounding tissues can cause hydronephrosis, impairing the function of the kidneys and leading to potential kidney failure if not addressed promptly.
-
-
General Malaise or Fever
-
If the fistula leads to an infection, patients may develop fever, chills, or general malaise. These symptoms may be signs of sepsis, which is a serious and life-threatening infection that can result from untreated urinary infections.
-
Diagnosis of Ureterovesical Fistula
Diagnosing a ureterovesical fistula involves a combination of clinical evaluation, imaging studies, and sometimes invasive diagnostic procedures. Here's how healthcare providers typically diagnose this condition:
Steps in Diagnosis
-
Medical History and Physical Examination
-
A thorough medical history is crucial. The doctor will inquire about prior surgeries, radiation therapy, pelvic trauma, and chronic infections. Physical examination may involve assessing signs of infection, swelling, or pain in the lower abdomen, flank, or pelvic area.
-
The physician will ask about urinary symptoms such as leakage, frequent UTIs, or flank pain.
-
-
Imaging Studies
-
CT Urography: Contrast-enhanced CT scans of the abdomen and pelvis are often the gold standard for diagnosing ureterovesical fistulas. They can identify any abnormal communications between the ureter and bladder and assess kidney function.
-
Retrograde Ureterography: This imaging technique involves introducing contrast material into the ureter and taking X-rays to visualize the abnormal tract between the ureter and bladder.
-
Cystoscopy: In this procedure, a small camera is inserted into the bladder through the urethra to directly visualize the bladder wall and any abnormal openings.
-
IVP (Intravenous Pyelography): IVP is a type of X-ray that uses contrast dye to visualize the kidneys, ureters, and bladder. It can reveal areas of urine leakage, obstruction, or fistula formation.
-
Ultrasound: An ultrasound may be used to assess kidney size and detect hydronephrosis (kidney swelling).
-
-
Laboratory Tests
-
Urinalysis and Urine Culture: These tests help identify any infection or blood in the urine (hematuria). Positive cultures can guide antibiotic treatment.
-
Renal Function Tests: Blood tests, such as creatinine and blood urea nitrogen (BUN), can be used to assess kidney function and determine the impact of the fistula on renal health.
-
Treatment Options for Ureterovesical Fistula
The treatment of ureterovesical fistulas depends on the size, location, and cause of the fistula, as well as the patient's overall health. Treatment options may include conservative management, surgical repair, or a combination of both.
Conservative Management (For Small or Early-Stage Fistulas)
-
Catheterization and Stenting
-
For small or recently diagnosed fistulas, ureteral
stenting (placing a catheter in the ureter to
divert urine flow) may be used. This allows the fistula to heal
over time, with urine being diverted away from the fistula site.
-
Antibiotics
-
Antibiotic therapy is used to treat or prevent
urinary tract infections (UTIs) and minimize
the risk of infection from urine leakage.
-
Hydration and Monitoring
-
Adequate hydration is essential to prevent
hydronephrosis and ensure normal kidney
function. Regular monitoring through imaging studies and urine
tests is necessary to assess the fistula's healing.
Surgical Treatment (Definitive Treatment)
Catheterization and Stenting
-
For small or recently diagnosed fistulas, ureteral stenting (placing a catheter in the ureter to divert urine flow) may be used. This allows the fistula to heal over time, with urine being diverted away from the fistula site.
Antibiotics
-
Antibiotic therapy is used to treat or prevent urinary tract infections (UTIs) and minimize the risk of infection from urine leakage.
Hydration and Monitoring
-
Adequate hydration is essential to prevent hydronephrosis and ensure normal kidney function. Regular monitoring through imaging studies and urine tests is necessary to assess the fistula's healing.
For larger fistulas or cases that do not respond to conservative treatment, surgical repair is often required. The goal of surgery is to remove the fistula tract and restore normal urine flow.
-
Ureteral Reimplantation (Ureteroneocystostomy)
This is the most common surgical procedure for ureterovesical fistulas. The surgeon excises the damaged portion of the ureter and reimplants the healthy segment into the bladder. This procedure restores the normal connection between the kidneys and bladder. -
Excision of the Fistula and Bladder Repair
In cases where the fistula involves both the bladder and ureter, the surgeon may remove the fistula tract and repair the bladder wall. This may require the use of sutures to close the opening and ensure the integrity of the bladder. -
Nephrectomy
In rare cases, when the kidney is severely damaged or the fistula cannot be repaired, a nephrectomy (removal of the affected kidney) may be necessary.
Prevention and Management of Ureterovesical Fistula
Ureterovesical fistula (abnormal connection between the ureter and bladder, sometimes extending to vagina) is usually an iatrogenic complication of pelvic or urologic surgery, and prevention depends on meticulous intra‑operative ureteral protection, while management ranges from temporary urinary diversion with stenting to definitive ureteral reimplantation into the bladder.
Prevention
While it may not be possible to prevent all ureterovesical fistulas, the risk can be minimized by:
-
Meticulous Surgical Technique: Surgeons should take extra care during pelvic surgeries to avoid injuring the ureter or bladder.
-
Radiation Protection: When radiation therapy is required, it's important to minimize exposure to the ureter and bladder.
-
Prompt Treatment of UTIs: Early intervention for urinary tract infections can help prevent the development of fistulas caused by infection or inflammation.
-
Avoiding Trauma: Protecting the pelvic area from injury (e.g., using seat belts, preventing falls) can reduce the risk of traumatic fistulas.
Management
For individuals diagnosed with ureterovesical fistulas:
-
Initial Monitoring: Early diagnosis and close monitoring with imaging studies can help identify small fistulas that may resolve on their own or require conservative management.
-
Surgical Management: Surgical repair is often necessary for larger fistulas. Follow-up care and monitoring are essential after surgery to ensure the fistula does not recur.
Complications of Ureterovesical Fistula
If left untreated, ureterovesical fistulas can lead to several complications:
-
Kidney Damage: Urine leakage can cause hydronephrosis, which leads to kidney damage or failure over time.
-
Infections: Chronic UTIs and kidney infections can occur due to abnormal urine flow.
-
Recurrence: Fistulas may recur after surgical repair, requiring additional interventions.
-
Scarring or Narrowing: The reimplantation site may develop narrowing or scarring, leading to urinary obstruction.
Living with Ureterovesical Fistula
Living with a ureterovesical fistula can be challenging, especially if symptoms are not managed appropriately. After treatment, patients must follow strict post-operative care guidelines to prevent recurrence. Regular follow-up with a healthcare provider is essential to monitor kidney function, urinary health, and overall quality of life.
Post-Treatment Care
-
Adherence to Postoperative Instructions: Patients must follow all instructions related to diet, hydration, hygiene, and avoiding strenuous activities to ensure proper healing.
-
Monitoring: Regular imaging studies are needed to ensure the fistula does not recur and to monitor kidney function.
-
Quality of Life: Managing urinary leakage, infections, and other complications can significantly improve a patient's quality of life.
Top 10 Frequently Asked Questions about Ureterovesical Fistula (UVF)
1. What is a Ureterovesical Fistula?
A ureterovesical fistula is an abnormal connection between the ureter (the tube that carries urine from the kidney to the bladder) and the bladder. Normally, urine flows from the kidney, through the ureter, into the bladder, and then out of the body via the urethra. However, in the case of a ureterovesical fistula, urine bypasses the normal urinary tract pathway due to the creation of a hole or passage between the ureter and bladder. This abnormal connection can lead to urine leakage, recurrent infections, and even damage to the kidneys if not treated. The fistula may result from previous surgeries, trauma, infections, or other medical conditions affecting the urinary system.
2. What causes a Ureterovesical Fistula?
Ureterovesical fistulas typically occur as a result of surgery, injury, or infection. Some of the most common causes include:
-
Pelvic or abdominal surgery: Previous operations like hysterectomy, prostate surgery, or any other surgery near the bladder or ureter can lead to accidental injury, creating a fistula.
-
Chronic inflammation: Conditions such as chronic urinary tract infections (UTIs), bladder or kidney stones, or inflammatory diseases (like tuberculosis) can weaken the tissue between the ureter and bladder, causing a fistula.
-
Trauma: Any injury to the pelvic or abdominal area, including accidents or blunt force trauma, may cause damage to the ureter or bladder.
-
Cancer: Tumors in the bladder, ureter, or surrounding areas can cause tissue breakdown, leading to the formation of a fistula.
In rare cases, the fistula may form spontaneously due to long-standing conditions like diverticulitis or radiation therapy.
3. What symptoms are associated with a Ureterovesical Fistula?
The symptoms of a ureterovesical fistula can vary, depending on the size and location of the fistula. Common symptoms include:
-
Urine leakage: Since the abnormal passage allows urine to flow outside the usual route, patients may experience urinary incontinence or continuous leakage, often described as an "overflow" condition.
-
Recurrent urinary tract infections: The abnormal connection increases the likelihood of bacteria entering the urinary system, leading to frequent UTIs, which may cause fever, pain, and burning during urination.
-
Urinary frequency or urgency: Some patients may experience a sensation of needing to urinate frequently or urgently, as the bladder is no longer functioning efficiently.
-
Flank or abdominal pain: When left untreated, urine backup can cause pressure and discomfort in the abdomen or lower back.
-
Kidney problems: Over time, a ureterovesical fistula can lead to kidney damage if urine flows backward (reflux) into the kidneys, increasing the risk of hydronephrosis (swelling of the kidney due to urine buildup).
4. How is a Ureterovesical Fistula diagnosed?
To diagnose a ureterovesical fistula, doctors typically rely on a combination of imaging studies, clinical examination, and patient history:
-
Imaging tests: A contrast study (like an intravenous pyelogram or CT urogram) helps visualize the fistula by showing how contrast dye travels through the urinary system. Cystoscopy, a procedure in which a small camera is inserted into the bladder, can directly view the fistula and help pinpoint its exact location.
-
Urine tests: The doctor may examine the urine to check for signs of infection, blood, or abnormal substances that could indicate a fistula.
-
Physical examination: A thorough exam will check for tenderness in the abdominal area, signs of urinary retention, or a history of previous surgeries or conditions that could have led to the fistula.
5. What are the treatment options for a Ureterovesical Fistula?
Treatment for a ureterovesical fistula typically involves surgical intervention to repair the abnormal connection. The specific approach depends on the size, location, and cause of the fistula:
-
Surgical repair: The primary treatment for ureterovesical fistulas is surgery to close the abnormal connection. This may involve stitching the fistula closed, removing any damaged tissue, and sometimes repositioning or reimplanting the ureter to restore proper function.
-
Stent placement: In some cases, a ureteral stent may be inserted to help drain urine from the kidney to the bladder while the area heals. Stents can provide temporary relief until surgical repair is performed.
-
Minimally invasive approaches: Depending on the location of the fistula, some surgeons may use laparoscopic or robotic techniques, which involve smaller incisions and faster recovery times.
If the fistula is caused by cancer or severe disease, additional treatments, such as chemotherapy or radiation, may be required.
6. What are the risks and complications of treating a Ureterovesical Fistula?
While surgery to repair a ureterovesical fistula is generally effective, there are some risks and potential complications:
-
Infection: There is a risk of infection at the surgical site, particularly in the urinary tract, which may require antibiotics or additional treatments.
-
Bleeding: Some bleeding is common during and after surgery, but excessive bleeding may require additional intervention.
-
Recurrence of the fistula: The fistula may recur if the repair fails, which could necessitate further surgery.
-
Damage to surrounding structures: The ureter and bladder are in close proximity to other vital organs, and surgery could inadvertently cause damage to surrounding tissues, such as nerves, blood vessels, or other organs.
-
Urinary retention or incontinence: In some cases, the surgical repair may lead to difficulty urinating, incomplete bladder emptying, or leakage, though this is rare and typically resolves with time.
7. What is the recovery process after Ureterovesical Fistula repair?
Recovery after surgery for ureterovesical fistula generally involves:
-
Hospital stay: Most patients stay in the hospital for 1-2 days after surgery, depending on the complexity of the procedure.
-
Catheter placement: A urinary catheter may be inserted to allow proper urine drainage while the area heals. The catheter is typically removed after a few days.
-
Follow-up care: Patients will need follow-up visits with the surgeon to monitor healing and ensure that the fistula does not recur. Imaging may also be performed to confirm that the fistula has been successfully closed.
-
Resuming normal activities: Most patients can return to light activities within 2-4 weeks, but strenuous exercise, heavy lifting, or activities that increase pressure on the bladder should be avoided for 6 weeks or longer.
-
Diet and fluid intake: Maintaining a healthy diet and staying hydrated is important for optimal healing.
8. How long does it take for full recovery?
While the initial recovery from surgery may take 1-2 weeks, full recovery can take 4-6 weeks for most patients. During this time, swelling and discomfort in the area will gradually subside. Some patients may experience mild urinary symptoms, such as urgency or frequency, during the early stages of recovery, but these symptoms typically improve as healing progresses. It can take several months for the internal tissues to fully heal and stabilize, especially in cases where the fistula was large or caused significant damage.
9. Can a Ureterovesical Fistula be prevented?
Preventing ureterovesical fistulas is often difficult, especially when caused by surgical complications or traumatic injury. However, steps that can minimize the risk include:
-
Careful surgical technique: Surgeons should ensure meticulous dissection and avoid unnecessary damage to the ureter during pelvic or abdominal surgeries.
-
Prompt treatment of urinary tract infections: Regular UTIs can contribute to tissue damage and increase the risk of fistula formation, so it is important to treat infections early.
-
Post-operative care: Following up after surgeries that involve the urinary tract and ensuring proper catheter care can help prevent the development of a fistula.
10. What are the long-term effects of a Ureterovesical Fistula if untreated?
If left untreated, a ureterovesical fistula can lead to:
-
Kidney damage: Urine leakage into the surrounding tissues may cause hydronephrosis (swelling of the kidney due to urine buildup), potentially leading to long-term kidney damage or failure.
-
Recurrent infections: The fistula increases the risk of frequent UTIs, which can spread to the kidneys or bloodstream, causing more serious complications.
-
Chronic incontinence or leakage: Without repair, the abnormal passage may cause persistent urine leakage, leading to discomfort and a reduced quality of life.


