Introduction to Vagina Posterior Repair
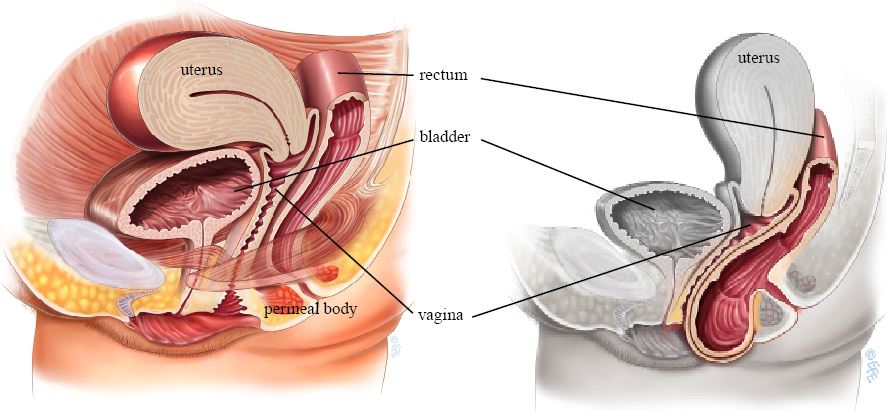
Posterior vaginal repair is a surgical procedure aimed at restoring the normal anatomy and support of the back wall (posterior wall) of the vagina and surrounding pelvic floor structures. It is commonly used to correct conditions such as posterior vaginal wall prolapse, rectocele, perineal body weakness, or a combination of these defects, which can arise when the supportive tissues between the vagina and rectum become weakened, stretched or damaged.
In a healthy anatomy, layers of fascia and pelvic floor muscles (including the rectovaginal fascia and perineal body) help support the vagina, maintain the separation between the rectum and vagina, and provide normal vaginal tone and function. When these support structures weaken, parts of the rectum (or, in some cases, small bowel) may bulge into the vagina, or the vaginal wall may sag, resulting in symptoms such as a vaginal bulge, a feeling of “fullness,” difficulty with bowel movements, discomfort, or decreased sexual satisfaction.
The goal of posterior repair is to reconstruct and reinforce the weakened fascial and muscular layers, restore normal anatomy and support, improve both bladder/bowel and sexual function (if affected), and relieve symptoms like bulge, pressure, or obstructed defecation.
Posterior repair may be done as a stand-alone procedure or combined with other pelvic floor repairs (e.g. perineorrhaphy, anterior vaginal wall repair, or vault suspension), depending on the patient's overall pelvic floor condition.
Causes and Risk Factors Leading to Need for Posterior Repair
Several factors may contribute to weakening of the posterior vaginal wall support, leading to the need for a posterior repair:
-
Childbirth and vaginal delivery: During pregnancy and especially vaginal childbirth (particularly difficult delivery, large baby, prolonged labor), the muscles, fascia, and perineal body may stretch, tear, or lose elasticity - making posterior wall prolapse or rectocele more likely. Repeated deliveries increase this risk.
-
Childbirth-related perineal trauma, episiotomy, or inadequate healing: Injuries to the perineum or the rectovaginal fascia during birth (e.g. tears, episiotomies) can compromise structural support. Over time, scar tissue or weakening may lead to prolapse or sagging.
-
Aging and tissue changes: With age, connective tissue loses elasticity; pelvic floor muscles may weaken; hormonal changes (e.g. reduced estrogen after menopause) may affect tissue quality - all contributing to loss of support.
-
Chronic increases in intra-abdominal pressure: Conditions leading to repeated straining (like chronic constipation), heavy lifting, chronic cough, obesity - these increase pelvic floor stress and can gradually weaken vaginal support structures over time. Similar risk factors apply for other compartments of pelvic organ prolapse.
-
Genetic/Connective-tissue predisposition: Some individuals may have inherently weaker fascia or connective tissue, making them more susceptible to prolapse or posterior wall weakness, even without obvious trauma or multiple childbirths.
-
Previous pelvic surgeries or inadequate repair: Prior surgeries involving the perineum, vaginal walls, episiotomies, or repairs may - if not properly healed or if scar tissue formation is suboptimal - predispose to posterior wall defects.
When these factors combine (e.g. childbirth + aging + chronic straining), the risk of a posterior vaginal wall defect or prolapse increases. Posterior repair becomes an option when symptoms affect quality of life or function.
Symptoms and Signs Suggestive of Posterior Wall Defect / Indication for Posterior Repair
Women with posterior vaginal wall prolapse or posterior compartment weakness may present with a variety of symptoms. The decision for surgery often depends on the severity of these symptoms and their impact on quality of life. Common presentations:
-
Sensation of vaginal bulge, fullness or pressure - many women describe a feeling that “something is coming down” or a bulge at the back wall of the vagina. This may worsen with standing, straining, lifting or bowel movements.
-
Difficulty with bowel movements, obstructed defecation, straining, incomplete evacuation, need to press/vaginal “splinting” to pass stool - especially when rectum bulges into vaginal wall (rectocele).
-
Discomfort or pain in pelvic or perineal area, particularly during sitting or intercourse. Some may experience dyspareunia (painful intercourse) if the posterior wall is lax or distorted.
-
Visible or palpable bulge at vaginal opening or perineum, especially when straining or during Valsalva maneuver. Some may notice tissue protrusion from vaginal opening.
-
Vaginal or perineal laxity / “looseness” - a sensation of reduced vaginal support or tone, often affecting sexual function or causing discomfort.
-
Recurrent infections or irritation - due to folds or redundant tissue that may trap moisture or cause friction.
-
Impact on quality of life - embarrassment, social discomfort, reduced sexual satisfaction, difficulty with hygiene, and psychological distress.
These symptoms vary widely - from mild discomfort to significant functional impairment - and many women may delay seeking help because of embarrassment or belief that such changes are “normal after childbirth.” However, when these symptoms impair daily living, posterior repair becomes a valid therapeutic option.
Diagnosis and Pre-operative Evaluation for Vagina Posterior Repair
Proper diagnosis and evaluation are critical to ensure that posterior repair is indicated and will provide benefit. The diagnostic pathway typically includes:
Clinical History and Physical Examination
-
Detailed medical, obstetric and gynecologic history - childbirth history, number of vaginal deliveries, history of perineal tears or episiotomy, symptoms (bulge, bowel dysfunction, pain, dyspareunia), lifestyle factors (constipation, heavy lifting, chronic cough), previous surgeries.
-
Physical pelvic examination (in lithotomy position) - inspection and palpation of vaginal walls (anterior and posterior), perineal body, genital hiatus, tissue integrity, muscle tone, presence of bulge / defect, measurements of pelvic floor support.
Pelvic Organ Prolapse Quantification (POP-Q) or similar examination
-
If prolapse is suspected, standardized assessment like POP-Q may be used to categorize prolapse severity (vaginal compartments, extent of descent), helping guide decision for repair.
Rectal/Defecatory Evaluation (if bowel symptoms present)
-
If the patient reports difficulty in bowel movements, obstructed defecation or incomplete evacuation, evaluation may include digital rectal exam, possibly defecography or proctological assessment to rule out rectal causes beyond the rectovaginal fascia defect.
Assessment of Perineal Body and Introitus
-
Examination of perineal length, perineal body integrity, introitus width, vaginal wall laxity, and any scar tissue from prior tears/repairs.
Counseling and Shared Decision-Making
-
Discussion with patient regarding goals: whether they seek repair for symptom relief (bulge, bowel issues), for functional improvement (bowel, sexual), or for aesthetic/perineal reconstruction.
-
Explanation of benefits, limitations, risks, possible alternatives (non-surgical measures: pelvic floor physiotherapy, lifestyle modifications, pessary use), realistic outcomes.
Only after thorough evaluation and shared decision-making should surgery be planned.
Treatment Options: Approaches for Vagina Posterior Repair
There are several surgical approaches for posterior vaginal wall repair, depending on the defect, patient's anatomy, symptoms, and surgeon's preference. Key options:
Traditional Posterior Colporrhaphy (Native Tissue Repair)
-
This is the most commonly performed posterior repair. It involves making an incision along the posterior vaginal wall (midline), dissecting the vaginal epithelium away from the underlying fascia/musculature (rectovaginal fascia), then plicating (folding and suturing) the fascia in the midline to reinforce support. Redundant vaginal mucosa may be trimmed, and the vaginal wall closed with absorbable sutures.
-
If needed, a concomitant perineorrhaphy (repair of perineal body) may be done: this repairs and reinforces the perineal muscles and tissues, trims redundant skin, and tightens the genital hiatus to support the posterior compartment and improve perineal anatomy.
-
This approach uses the patient's own tissues (“native tissue repair”) and avoids synthetic mesh - which many recent guidelines recommend, due to mesh-related complications in vaginal repairs.
Site-Specific Defect Repair
-
Instead of uniform midline plication, surgeons may identify specific areas of fascia weakness and repair only those defects. This may limit tissue tightening to necessary regions, possibly reducing risk of vaginal over-constriction.
-
This technique may be preferred in patients where prolapse or defect is localized, rather than generalized laxity.
Use of Grafts or Mesh (less favored nowadays)
-
In the past, synthetic mesh or biologic grafts were sometimes used to reinforce the posterior wall repair - especially in patients with weak native tissue or recurrent prolapse. However, evidence shows variable results; mesh in posterior repairs has been associated with higher risks (erosion, functional problems), and many guidelines now advise against routine mesh use in posterior compartment repairs.
-
For most cases, native tissue repair remains the standard, unless special circumstances demand otherwise.
Combined Repairs
-
Posterior repair is often combined with perineorrhaphy when perineal body deficiency or widened genital hiatus is present.
-
In cases of multi-compartment prolapse (e.g. both anterior and posterior defects, or uterine prolapse), posterior colporrhaphy may be performed alongside anterior repair or apical support procedures - depending on the overall pelvic floor evaluation.
Prevention and Non-Surgical Management / When to Consider Repair
Not all posterior wall defects or mild prolapse require surgery. Prevention and non-surgical management may help lessen progression or delay need for surgery. Key aspects:
Pelvic Floor Muscle Training (PFMT) / Physiotherapy
-
Strengthening pelvic floor muscles via regular, guided exercises (e.g., Kegel exercises) may improve support, reduce prolapse symptoms, and enhance outcomes - particularly in early or mild stages.
-
Pelvic floor physiotherapy may also aid in recovery and maintenance after repair.
Lifestyle Modifications
-
Avoiding chronic straining (e.g., managing constipation, avoiding heavy lifting, controlling chronic cough), maintaining healthy body weight, avoiding excessive intra-abdominal pressure - all help reduce stress on pelvic floor support structures.
-
Healthy tissue maintenance: good nutrition, hydration, avoid smoking (which impairs connective tissue healing).
Use of Pessaries or Support Devices
-
For women who are poor surgical candidates, or who wish to delay surgery, vaginal pessaries (support devices) may offer symptomatic relief by providing mechanical support.
Regular Monitoring and Conservative Management
-
If symptoms are mild and not significantly affecting quality-of-life, periodic monitoring with pelvic floor evaluation may suffice.
Surgery becomes more justified when symptoms (bulge, obstructed defecation, sexual dysfunction, quality-of-life impact) are moderate to severe, or when non-surgical management fails.
Complications and Risks of Vagina Posterior Repair
As with any surgery, posterior repair carries potential risks and complications - short-term and long-term. Important to counsel patients on these before surgery.
Early/Post-operative Risks
-
Bleeding, hematoma, bruising - due to incision and tissue dissection. Proper surgical technique and postoperative care reduce risk.
-
Infection - vaginal surgeries carry increased risk; infection prevention protocols essential.
-
Pain, discomfort, vaginal bleeding or spotting - mild bleeding or discharge may persist for 1-2 weeks after surgery; sutures typically dissolve, but occasional “stitch-remnants” may emerge, which generally is normal.
-
Delayed healing or wound dehiscence - especially if the patient strains (e.g. constipation, heavy lifting) too soon after surgery. Proper postoperative instructions needed.
Medium-Term or Long-Term Risks
-
Dyspareunia (painful intercourse) or sexual dysfunction - if the vaginal canal is over-constricted, or excessive tissue tightening/scarring occurs. Surgeons must balance repair strength with preservation of vaginal caliber.
-
Recurrence of prolapse or rectocele - despite repair, some cases may relapse over time - especially if underlying risk factors (e.g. chronic straining, poor tissue quality) persist. Native-tissue repairs have acceptable but not perfect long-term durability.
-
Bowel or rectal dysfunction - rarely, if dissection or sutures involve rectal wall, there might be complications; careful surgical technique and postoperative follow-up needed.
-
Altered sensation, perineal tightness, or discomfort - due to perineorrhaphy or perineal body reconstruction. Over-tightening should be avoided to prevent long-term discomfort.
Because of these risks, success depends heavily on proper patient selection, surgical technique, realistic expectations, and good postoperative care.
Living with Vagina Posterior Repair: Recovery and Long-Term Outlook
Postoperative Recovery
-
Most patients are discharged within a few days; a vaginal “pack” may be placed immediately post-surgery to control bleeding - removed usually after 24-48 hours. A catheter may be used overnight in some cases.
-
Expect vaginal bleeding or spotting for 1-2 weeks (similar to a light period); sanitary pads recommended over tampons to reduce infection risk.
-
Pain or discomfort is common initially - painkillers and rest recommended. Bowel management (diet, stool softeners) is important to avoid straining.
Return to Activities
-
Light daily activities may resume within a few days; however, avoid heavy lifting, straining, or vigorous exercise for several weeks.
-
Doctors generally recommend abstaining from vaginal intercourse for about 6 weeks to allow healing.
-
Follow-up appointment usually at 4-6 weeks to assess healing, discuss symptoms, and plan gradual return to normal life.
Long-Term Outlook
-
Many women report relief of bulge sensation, improved bowel function, reduced need for manual splinting during defecation, and restored vaginal anatomy and function after successful repair.
-
To maintain results over the long term: adopt healthy lifestyle habits - avoid chronic straining, constipation; maintain pelvic floor strength; avoid excessive intra-abdominal pressure; manage body weight.
-
Regular gynecologic / urogynecologic follow-ups recommended to monitor pelvic floor support, detect recurrence early, and manage any long-term functional issues (e.g. sexual discomfort, bowel changes).
Top 10 Frequently Asked Questions about Vaginal Posterior Repair
1. What is Vaginal Posterior Repair?
Vaginal Posterior Repair, also known as Posterior Colporrhaphy or Rectocele Repair, is a surgical procedure designed to correct a rectocele, a condition where the rectum bulges into the back wall of the vagina. This typically happens when the tissue and muscles that support the vaginal walls and rectum weaken, often due to childbirth, aging, or chronic strain (such as constipation). The surgery involves tightening and supporting the posterior vaginal wall, often by repairing or reinforcing the pelvic fascia, which separates the vagina from the rectum, to restore normal anatomy and function. In some cases, the perineum (the area between the vaginal opening and the anus) may also be repaired if needed.
2. When is Vaginal Posterior Repair recommended?
Vaginal Posterior Repair is usually recommended for women experiencing:
-
Rectocele (vaginal bulging): This condition occurs when the posterior wall of the vagina weakens, causing the rectum to push through the vaginal wall, resulting in a noticeable bulge and a feeling of pressure or heaviness.
-
Difficulty during bowel movements: Women with rectocele may feel like they need to press on their vagina to help pass stool, or they may experience incomplete bowel evacuation.
-
Sexual discomfort: If the rectocele or other vaginal wall prolapse causes discomfort during intercourse, a posterior repair can help restore the vaginal walls and improve comfort.
-
Pelvic organ prolapse (POP): Vaginal posterior repair can be a part of a broader treatment plan for pelvic organ prolapse, where various organs (such as the bladder, uterus, and rectum) descend into the vaginal canal.
3. How is Vaginal Posterior Repair performed?
The procedure is usually done under general or regional anesthesia, and it involves the following steps:
-
An incision is made along the posterior wall of the vagina, near the vaginal entrance.
-
The weakened or stretched tissue is carefully repaired or tightened to restore normal support and reduce any prolapse or bulging.
-
The perineal body (tissue between the vagina and anus) may also be repaired if necessary to improve pelvic floor support, especially after childbirth injuries.
-
Excess tissue may be trimmed, and the vaginal wall is then sutured back together. The stitches used are typically absorbable, meaning they dissolve naturally over time.
-
In some cases, the surgery is done alongside anterior vaginal wall repair or other pelvic floor surgeries, depending on the individual's condition.
The goal of the surgery is to restore the anatomical position of the rectum, repair any tears or weaknesses, and relieve symptoms of prolapse.
4. What are the benefits of Vaginal Posterior Repair?
After undergoing Vaginal Posterior Repair, patients can expect several benefits:
-
Restoration of normal anatomy: The procedure helps reposition and support the posterior vaginal wall and rectum, reducing bulging and pressure.
-
Improved bowel function: The surgery can help alleviate difficulties during bowel movements, such as needing to press on the vagina to pass stool, by restoring support to the rectum.
-
Increased sexual comfort: For women who experience pain or discomfort during intercourse due to vaginal laxity or rectocele, the repair can restore normal vaginal tone and improve sexual satisfaction.
-
Enhanced pelvic floor health: By repairing weakened tissues, Vaginal Posterior Repair improves overall pelvic floor strength, which can reduce the risk of future prolapse or incontinence issues.
-
Improved self-esteem and comfort: Many women report feeling more comfortable, both physically and emotionally, after the repair, as the condition can affect confidence and quality of life.
5. What are the risks and potential complications of Vaginal Posterior Repair?
As with any surgery, Vaginal Posterior Repair carries some risks:
-
Infection: There is always a risk of infection at the surgical site or in the urinary tract.
-
Bleeding: Some bleeding is expected, but excessive bleeding may require further treatment.
-
Scarring: Though the surgeon tries to minimize visible scarring, some scarring is inevitable. In rare cases, scarring can cause discomfort or difficulty during intercourse.
-
Changes in sensation: Some women may experience changes in vaginal sensation, either increased sensitivity or numbness, after surgery.
-
Urinary or bowel issues: Although rare, there is a possibility of temporary or long-term difficulty with urination or bowel movements after surgery.
-
Recurrence of prolapse: In some cases, the prolapse may recur, particularly if there are underlying risk factors such as multiple childbirths or obesity.
To minimize these risks, it's essential to follow post-operative care instructions and attend follow-up visits with the surgeon.
6. What does the recovery process involve after Vaginal Posterior Repair?
The recovery process after Vaginal Posterior Repair can vary depending on the individual and the complexity of the surgery:
-
Hospital stay: Most women can go home the same day or after an overnight stay, depending on the surgical approach and recovery.
-
Pain management: Mild to moderate pain and discomfort are common after surgery. Pain can usually be controlled with prescribed medications.
-
Activity restrictions: Women are typically advised to avoid strenuous physical activities, heavy lifting, and sexual intercourse for about 6-8 weeks to allow proper healing.
-
Follow-up care: A follow-up visit with the surgeon is usually scheduled within 2-4 weeks after surgery to monitor healing, check for any complications, and remove any stitches if necessary.
-
Hygiene and care: Proper hygiene, including gentle washing of the vaginal area, is important to prevent infection. Additionally, women may be asked to refrain from using tampons or engaging in activities that put pressure on the pelvic area during the initial healing period.
Recovery usually takes a few weeks, but it may take up to 3 months for complete healing.
7. How long does it take to recover from Vaginal Posterior Repair?
While the immediate recovery phase typically lasts 2-6 weeks, full recovery can take 2-3 months. During the initial recovery phase, most women experience mild to moderate soreness, swelling, and occasional vaginal discharge. Patients are encouraged to take it easy and gradually resume their regular activities.
-
First 2-3 weeks: Limited activity, mostly resting and avoiding strenuous efforts.
-
Up to 3 months: Complete tissue healing and return to full functionality. During this time, follow-up appointments are crucial to monitor for any complications and ensure proper recovery.
8. Does Vaginal Posterior Repair affect sexual function?
Many women report improved sexual satisfaction after Vaginal Posterior Repair. The
surgery can restore normal vaginal tone, reduce the feeling of vaginal laxity, and
address any discomfort caused by rectocele or perineal damage.
However, it is important to allow the vaginal tissues time to heal before resuming
sexual activity. Women are usually advised to avoid sexual intercourse for about
6-8 weeks after surgery to allow the vaginal tissues to heal properly
and avoid complications.
If there is any concern about sexual discomfort after recovery, a follow-up visit with
the surgeon or a pelvic health specialist can help address issues and guide pelvic floor
rehabilitation.
9. Can I still have children after Vaginal Posterior Repair?
Yes, it is generally possible to have children after Vaginal Posterior Repair. However,
it's important to consider the impact of childbirth on the surgical repair. Vaginal
deliveries, in particular, may put pressure on the pelvic floor and potentially reverse
some of the benefits of the repair.
Surgeons typically recommend waiting until family planning is complete
before undergoing the procedure to ensure the results are long-lasting. If a woman does
decide to have a baby after the surgery, it's important to discuss potential risks with
the healthcare provider, as future pregnancies may affect pelvic floor health.
10. How can I prevent prolapse or other issues from recurring after surgery?
While surgery can correct prolapse and vaginal wall weakness, there are steps you can take to maintain the results:
-
Maintain a healthy weight: Excess weight can increase pressure on the pelvic floor, which can contribute to prolapse and other pelvic floor issues.
-
Avoid constipation and straining: Regular bowel movements without excessive straining will reduce pressure on the pelvic region.
-
Pelvic floor exercises (Kegel exercises): Strengthening the pelvic floor muscles can help prevent recurrence of prolapse and improve overall pelvic health.
-
Lifestyle changes: Avoid heavy lifting and high-impact activities that put strain on the pelvic area. Consider using proper lifting techniques if engaging in physical activity.
By following these preventive measures, women can reduce the risk of prolapse recurrence and maintain pelvic health long after surgery.


