Introduction to Vitrectomy
Vitrectomy is a delicate and sophisticated surgical procedure performed by retina specialists to treat various vitreoretinal diseases and conditions. The procedure involves removing all or part of the vitreous humor - the gel-like substance that fills the center of the eye - to address a variety of vision-threatening issues. Vitrectomy is essential in treating a range of conditions that affect the retina, macula, or vitreous cavity, ultimately aiming to restore or preserve a patient's sight.
The vitreous humor is a transparent gel that helps maintain the shape of the eyeball and allows light to pass through to the retina. However, in certain conditions - such as retinal detachment, vitreous hemorrhage, macular holes, retinal tears, and epiretinal membranes - the vitreous can become cloudy, pull on the retina, or interfere with vision. Vitrectomy is used to remove these obstructive or damaging elements, often followed by retinal reattachment, membrane peeling, or gas tamponade to stabilize the eye and promote healing.
Key objectives of vitrectomy include:
-
Removing vitreous hemorrhage caused by diseases like diabetic retinopathy or injury
-
Reattaching the retina in cases of retinal detachment
-
Repairing macular holes or epiretinal membranes that distort vision
-
Clearing up infections like endophthalmitis, where bacteria or fungi invade the eye
-
Managing complications after other surgeries, such as cataract surgery or lens dislocations
Vitrectomy is typically performed in an operating room under local anesthesia or general anesthesia depending on the severity and location of the problem. The procedure usually requires small incisions to access the vitreous cavity, which is then removed using microsurgical instruments. Once the vitreous is removed, the space may be filled with saline solution, gas bubble, or silicone oil to maintain pressure and support the retina until it heals.
Causes / Indications and Risk Factors for Vitrectomy
Vitrectomy is not performed arbitrarily - it's indicated under specific eye conditions where vitreous or retinal pathology threatens vision or eye integrity. Common indications include:
-
Vitreous hemorrhage: bleeding into the vitreous cavity (due to trauma, diabetic eye disease, retinal tears) which clouds the gel and blocks light, impairing vision.
-
Retinal detachment: when the retina separates from the underlying layers, leading to vision loss; vitrectomy allows retina repair, removal of traction, and re-attachment.
-
Macular hole or epiretinal membrane (macular pucker): abnormalities affecting the central retina (macula) that distort vision; removing vitreous and peeling membranes helps restore retinal anatomy.
-
Complications from other eye surgeries: e.g. after complicated cataract surgery, posterior capsule rupture, or lens fragment retention, vitreous may prolapse or become problematic - vitrectomy helps clean the vitreous cavity.
-
Trauma or eye injury: penetrating injuries, foreign bodies, or blunt trauma causing vitreous damage, hemorrhage, or retinal disruption may require vitrectomy.
-
Severe diabetic retinopathy / retinal vascular disorders: abnormal blood vessels, proliferative changes, retinal bleeding or scar tissue formation may necessitate vitrectomy to remove vitreous blood and stabilize retina.
-
Intraocular infection (endophthalmitis), inflammation, or other vitreoretinal diseases: where clearing of vitreous and repair may salvage vision or prevent further damage.
Risk factors or circumstances that influence the decision for vitrectomy:
-
Severity and persistence of symptoms (e.g. non-clearing hemorrhage, progression of detachment, lack of improvement with conservative therapy)
-
Condition of retina/lens/overall eye health - pre-existing cataract, glaucoma, prior surgeries, degree of retinal damage or comorbidities.
-
Patient's systemic health, compliance - post-op requirements (e.g. head positioning, follow-up visits), ability to manage after-care.
Thus, vitrectomy is indicated when the potential benefit - preservation or restoration of vision, prevention of permanent damage - outweighs the risks inherent to intraocular surgery.
Symptoms and Signs - When Vitrectomy May Be Needed
Patients who eventually undergo vitrectomy often present with one or more of the following symptoms or clinical signs, indicating vitreous or retinal disease:
-
Sudden or progressive loss of vision / blurred vision - may be partial or complete depending on severity of vitreous hemorrhage, retinal detachment, or macular involvement.
-
Floaters, flashes, or “spots” in vision - often described as cobweb-like shadows, moving specks, or sudden flashes - may indicate vitreous hemorrhage, retina traction, or posterior vitreous detachment.
-
Dark curtain or shadow over part of visual field - especially suggestive of retinal detachment - a serious sign needing prompt evaluation.
-
Distorted or wavy central vision (metamorphopsia) - may occur when macula is involved (macular hole, epiretinal membrane), or when scar tissue distorts retinal surface.
-
Persistent vitreous hemorrhage not clearing on its own - repeated or dense bleeding, especially in diabetic retinopathy or vascular disease, raising risk of further complications.
-
Eye trauma history with visual disturbance - following injury, foreign body, lens issues or surgery complications leading to vitreous damage.
-
Reduced night vision, glare, shadows, fluctuating vision - may reflect media opacities (blood, debris) in vitreous that interfere with light transmission.
If such symptoms are present - especially sudden ones, or those worsening over time - prompt ophthalmologic evaluation is critical. Early detection and timely vitrectomy often yield better visual outcomes and reduce risk of permanent damage.
Diagnosis - How Eye Specialists Decide When to Do Vitrectomy
Deciding on vitrectomy involves a thorough ophthalmic work-up. Steps usually include:
a. Clinical and Ophthalmic Examination
-
Visual acuity test (how well the patient sees with or without correction) to assess degree of vision loss.
-
Slit-lamp + dilated fundus exam: to inspect front (anterior) chamber and back (retina, vitreous) of eye - check for hemorrhage, debris, retinal tears, detachments, membranes, macular problems, etc.
-
Intraocular pressure (IOP) measurement - ensures no dangerously high or low pressures, especially important if gas/oil will be used.
b. Imaging & Diagnostic Tests
-
Optical Coherence Tomography (OCT): crucial for macular disorders (macular hole, epiretinal membrane), gives cross-sectional view of retina and vitreoretinal interface to detect subtle traction, membrane, macular edema.
-
Ultrasound B-scan: useful when dense hemorrhage or opacity prevents clear fundus view; can detect retinal detachment, vitreous opacities, foreign bodies.
-
Fluorescein angiography (in vascular retinopathies) to visualize blood vessel leaks, neovascularization, helps plan treatment. (Though not always needed).
c. Evaluation of Overall Eye & Patient Health
-
Review of ocular history - prior eye surgeries (cataract, IOL), trauma, lens status (phakic, pseudophakic), comorbidities (diabetes, hypertension), risk factors for infection or healing issues.
-
Assessment of patient's ability to comply with post-surgery requirements (e.g. head posture if gas bubble used), follow-up schedule, hygiene, medication adherence.
d. Informed Consent & Shared Decision Making
Because vitrectomy has potential risks and variable outcomes - especially depending on eye condition - a retina specialist must counsel the patient about:
-
expected benefit (vision preservation or improvement),
-
possible complications (bleeding, infection, retina tears, cataract, pressure changes),
-
post-operative requirements (gas/oil tamponade, positioning, limitations),
-
alternative options (observation, laser, injections) if suitable.
If benefits outweigh risks, and patient consents with understanding, surgery is scheduled.
Treatment Options & What Vitrectomy Involves - The Procedure
Vitrectomy is not a single uniform procedure. Depending on the underlying condition, eye status, and surgeon's decision, different variants and steps are used. Overview:
a. Types of Vitrectomy
-
Pars Plana (Posterior) Vitrectomy (PPV) - the most common type. Instruments are introduced through small incisions (ports) in the sclera (white of eye) about 3-4 mm behind the cornea, through the pars plana. This gives access to the vitreous cavity and retina with minimal disruption to anterior structures.
-
Anterior Vitrectomy - used when vitreous gel moves forward (e.g. after complicated cataract surgery, lens issues), or when vitreous prolapses into front chamber; smaller volume removed.
b. What Happens During Surgery
-
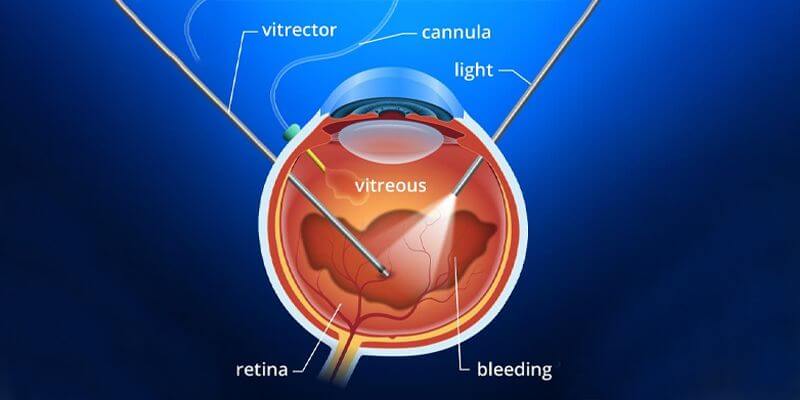
Under local anesthesia (or general, depending on case), surgeon makes tiny incisions/ports (23-gauge, 25-gauge or smaller) into sclera for instrument insertion - a light source, a vitreous cutter (vitrector), and infusion line.
-
The vitreous gel is cut and suctioned out - core vitrectomy (central vitreous) or complete removal depending on pathology (blood, debris, hemorrhage, scar tissue)
-
If needed, additional procedures may be done:
-
Membrane peeling / epiretinal membrane removal (e.g. for macular pucker)
-
Internal limiting membrane (ILM) peeling (e.g. for macular hole)
-
Laser photocoagulation, cryotherapy, or retinopexy to fix retinal tears, detachments
-
Removal of retained lens fragments, foreign bodies if present
-
-
At the end of surgery, the vitreous cavity is refilled with: saline / balanced salt solution; or - depending on condition - a gas bubble or silicone oil to provide internal tamponade and keep retina attached while healing occurs.
-
Because modern instrumentation is small gauge, often no sutures are needed - ports self-seal; reduces inflammation, speeds recovery.
c. Combined Procedures
Vitrectomy is often combined with other surgeries when necessary - for example, cataract surgery (phacoemulsification) if cataract is present or likely to develop soon after vitrectomy. Combined surgery can save a second operation and may improve overall outcome.
Vitrectomy thus offers flexibility - can be tailored (partial / full), combined with membrane peeling / laser / other surgical steps - depending on individual eye pathology.
Prevention and Management - Before & After Vitrectomy
Because vitrectomy deals with serious retinal or vitreous conditions, “prevention” here refers to early detection, timely intervention, and good postoperative management to optimize outcomes.
a. Before Surgery - Preparation & Prevention
-
Regular eye check-ups, especially for high-risk individuals (diabetics, hypertension, eye injury history, prior eye surgery) - early detection of retinal problems, hemorrhage, detachments, or membranes helps intervene before severe vision loss.
-
Control systemic risk factors - e.g. manage diabetes, hypertension, vascular disease, other comorbidities to reduce risk of retinal vascular complications or hemorrhage.
-
Patient counselling & education - explain risks, benefits, post-operative expectations (tamponade, positioning, activity restrictions), need for follow-ups.
-
Ensure access to experienced vitreoretinal surgeon, appropriate facility, sterile setup - because vitrectomy is delicate surgery requiring significant expertise.
b. After Surgery - Post-operative Care & Long-Term Management
-
Eye care and medications: use prescribed antibiotic/anti-inflammatory eye drops to prevent infection and control inflammation. Keep the eye clean, avoid touching or rubbing eye.
-
Positioning and care if gas bubble used: Many procedures require patients to maintain specific head/eye positions (e.g. face-down) for a period for proper healing and retina attachment. Avoid flights or altitude changes while gas bubble remains.
-
Avoid strenuous activity, heavy lifting, eye strain for a few weeks. Rest and gradual return to normal activity as per surgeon instructions.
-
Regular follow-up visits - to check retina status, intraocular pressure, cataract formation, inflammation, retinal attachment, need for further interventions (like silicone-oil removal if used).
-
Long-term eye health maintenance - manage systemic risk factors (blood sugar, blood pressure), avoid eye trauma, maintain periodic retinal screenings, use protective eyewear if needed.
Timely intervention, good surgical technique, and disciplined post-operative care maximize the chances of successful visual recovery and minimize complications.
Complications and Risks of Vitrectomy
While vitrectomy is a powerful and often vision-saving procedure, it carries inherent risks. Many are rare with modern techniques, but patients must be aware.
Common / Known Risks
-
Cataract formation or acceleration - especially in older patients; vitrectomy often hastens formation of lens opacities requiring later cataract surgery. Some studies suggest visually significant cataract develops in many patients after vitrectomy.
-
Intraocular inflammation, redness, discomfort, swelling - typical after surgery, generally transient.
-
Bleeding / hemorrhage inside eye (vitreous hemorrhage, choroidal bleeding) - though uncommon, can threaten vision especially if severe.
-
Retinal tears or detachment (iatrogenic) - even in skilled hands, instrument manipulation can cause unintended retinal tears; in some series occurrence ~2-4%.
-
Infection (endophthalmitis) - a serious but rare complication (modern small-gauge vitrectomy has low incidence), but when occurs can lead to severe vision loss.
-
Intraocular pressure (IOP) changes - glaucoma or hypotony - pressure may rise or fall depending on tamponade substance (gas/oil), inflammation, or surgical impact.
Less Common but Serious / Long-Term Risks
-
Need for additional surgeries - e.g. to remove silicone oil, repair recurrent detachment, manage complications like retinal tears, glaucoma, or cataract.
-
Visual outcome not guaranteed / limited recovery - if retina or macula was severely damaged before surgery, some patients may have only partial improvement or stabilization rather than full restoration.
-
Lens/IOL complications in future surgeries - prior vitrectomy may complicate later cataract surgery or intraocular lens (IOL) implantation / stability.
-
Rare events: suprachoroidal hemorrhage, retinal toxicity, sympathetic ophthalmia, prolonged inflammation - though very rare, these severe complications can threaten vision.
Large contemporary reviews suggest that severe complications have low incidence (e.g. <1% for some), but less-severe complications - hemorrhage, need for additional surgery - remain significant considerations.
Hence, vitrectomy must be offered only when benefits outweigh risks, and patients must be counselled clearly about potential outcomes and need for follow-up.
Living with Vitrectomy - Recovery, Quality of Life & Long-Term Outlook
Vitrectomy can significantly improve vision and quality of life, especially when performed timely and under good conditions. But recovery and long-term care matter a lot. Here's what living with vitrectomy often involves:
Recovery Period (Short / Medium Term)
-
Immediately after surgery: Redness, mild discomfort, light sensitivity, watery eye or mild pain are common. Eye drops (antibiotic, anti-inflammatory) prescribed. Eye shield or patch may be used in initial period.
-
Visual experience may be altered: if a gas bubble is used - vision often blurred (bubble interferes with light refraction), may see “bubbles” or distortion until bubble dissolves; patient may need to maintain certain head/eye position for days to weeks.
-
Restrictions: avoid heavy lifting, strenuous physical exertion, eye rubbing or pressure; avoid air travel/altitude changes if gas bubble still present.
Medium / Long-Term Outcomes
-
Many patients experience improvement or stabilization of vision - especially when retinal detachment, hemorrhage, macular hole or membrane were successfully repaired.
-
Some may need additional surgery - for cataract formation, silicone-oil removal (if used), or to manage complications such as secondary glaucoma, retina re-detachment, etc.
-
Need for regular follow-up: retina exams, IOP checks, lens status monitoring, retina integrity, optical coherence tomography as needed, especially in chronic conditions (diabetic retinopathy, vascular diseases).
-
Lifestyle and systemic health: Good control of systemic disease (e.g. diabetes, hypertension), eye protection (sunglasses, avoid trauma), healthy habits to reduce risk of further retinal vascular complications.
Psychosocial & Quality-of-Life Considerations
-
For many, vitrectomy offers hope of regained vision, or at least prevention of further vision loss - a big improvement in quality of life, daily functioning, independence.
-
Realistic expectations are important: depending on underlying disease, full “normal” vision may not return; but stabilization, reduced symptoms (floaters, flashes, visual distortion) and improved reliability are often possible.
-
Patients should be informed about possibility of cataract development, need for follow-up procedures, and long-term care commitment - mental preparedness and support help with better adaptation.
Top 10 Frequently Asked Questions about Vitrectomy
1. What is Vitrectomy?
Vitrectomy is a surgical procedure in which the vitreous humor - the clear, gel-like substance that fills the center of the eye - is removed. The vitreous may need to be removed when it becomes cloudy due to conditions like bleeding, infections, scar tissue, or retinal detachment. This procedure allows surgeons to access the retina and other delicate structures of the eye to treat diseases, correct defects, or remove damaged tissue. After the vitreous is removed, the eye is usually filled with a special fluid or gas to help maintain the shape of the eye while the retina heals.
2. Why is Vitrectomy needed - what conditions does it treat?
Vitrectomy is typically needed when the vitreous humor becomes involved in diseases or conditions that affect vision or the health of the eye. Some of the conditions that may require vitrectomy include:
-
Retinal Detachment: Where the retina, which is responsible for vision, separates from its normal position.
-
Vitreous Hemorrhage: When blood enters the vitreous, usually from a ruptured blood vessel, causing vision obstruction.
-
Macular Hole: A small break in the central part of the retina (macula) that can lead to significant vision loss.
-
Diabetic Retinopathy: A condition in which damage from diabetes affects the retina, often causing bleeding or scarring.
-
Epiretinal Membrane: Scar tissue that forms on the surface of the retina, leading to vision distortion.
-
Infections or Inflammation: Conditions such as endophthalmitis, which can affect the vitreous and require surgical removal.
In these cases, vitrectomy helps improve vision or prevent further complications by addressing underlying damage or obstructions.
3. How is Vitrectomy performed?
The vitrectomy procedure is typically done under local anesthesia,
meaning the patient remains awake, but the eye is numbed, or it may be done under
general anesthesia for certain cases. The surgeon makes a small
incision in the eye to access the vitreous humor. A specialized instrument is used to
carefully remove the vitreous gel. Once removed, the surgeon can treat the underlying
problem, such as repairing a tear in the retina or removing scar tissue.
After the procedure, the eye is filled with a gas bubble or
silicone oil to maintain the shape of the eye and support the retina
during the healing process. The incision is usually so small that it may not require
sutures.
4. What benefits or improvements can I expect after Vitrectomy?
Vitrectomy can lead to several positive outcomes, including:
-
Improved Vision: Many patients experience significant improvement in vision, particularly if the surgery was performed to remove blood or debris from the vitreous. If the procedure is done to treat retinal detachment, it can restore or preserve vision.
-
Relief from Retinal Pressure: In cases of retinal detachment, macular hole, or other retinal conditions, vitrectomy can relieve pressure on the retina, preventing further damage and vision loss.
-
Restoration of Eye Health: The surgery removes damaged tissue and debris, leading to a healthier eye and improved function.
-
Stabilization of Vision: For some conditions, vitrectomy may prevent further deterioration of vision and prevent complications like retinal scarring or continued hemorrhaging.
However, the extent of improvement depends on the severity of the underlying condition, how long it's been present, and the overall health of the retina and eye.
5. What are the risks and potential complications of Vitrectomy?
While vitrectomy is generally safe, as with any surgery, there are potential risks and complications:
-
Infection: As with any eye surgery, there is a risk of infection at the surgical site, which could lead to more serious complications if not treated.
-
Bleeding: Although bleeding is controlled during the procedure, there is a possibility of post-surgical bleeding, especially if there was a history of retinal hemorrhage.
-
Retinal Detachment: A rare but serious complication where the retina may detach after surgery, requiring further treatment.
-
Increased Eye Pressure (Glaucoma): The eye pressure may rise after surgery, which can damage the optic nerve if not addressed.
-
Cataract Formation: Cataracts can form more quickly in the operated eye, especially in older patients, due to changes in the lens after surgery.
-
Vision Loss or Visual Distortion: While the goal of vitrectomy is to improve vision, in some cases, it may not restore full vision, or the vision may be distorted, especially if the retina is severely damaged.
While these risks exist, most complications are manageable, and the surgeon will provide instructions to minimize them.
6. What is the recovery process like after Vitrectomy?
The recovery process after vitrectomy depends on the complexity of the surgery and the individual's overall health:
-
Post-surgery care: After the procedure, patients may need to rest and keep the eye shielded. The first few days typically involve mild discomfort and swelling, which can be managed with medication.
-
Follow-up appointments: Regular follow-up visits are crucial to monitor healing and ensure no complications arise.
-
Activity restrictions: Patients are generally advised to avoid heavy lifting, vigorous activity, and certain movements for the first few weeks. For some surgeries, patients may need to position themselves in specific ways (e.g., face-down) to encourage proper healing, especially if gas bubbles were used.
-
Vision stabilization: Initial vision recovery may involve blurry or hazy sight, which gradually improves over time. Complete healing can take several weeks to months, and vision may continue to improve during this period.
For patients who had a gas bubble inserted, it may take several weeks for it to absorb and for vision to stabilize. The full recovery period may take 6 months or longer in some cases.
7. How long does it take to recover from Vitrectomy?
While recovery times vary by individual and the specific procedure, the general timeline is:
-
Immediate recovery: Patients may stay in the hospital for a day or two after the surgery, depending on the complexity of the procedure.
-
1-2 weeks: Most of the swelling, discomfort, and bruising subside, and patients can resume light daily activities, though strenuous physical activities should still be avoided.
-
3-6 weeks: Vision may improve during this time, but it's crucial to attend follow-up visits to check for complications and healing.
-
3-6 months: Full recovery and stabilization of vision can take several months, especially if retinal damage was severe or the eye was filled with gas or silicone oil.
During recovery, patients should take great care to follow post-operative instructions to avoid complications and speed up the healing process.
8. Does Vitrectomy affect my lifestyle or daily activities?
Vitrectomy may have a short-term impact on your daily activities, but with proper care, you can gradually return to normal. During the first few weeks, patients are advised to avoid heavy lifting, bending, or any activities that put pressure on the eyes.
-
Vision: You may experience blurry vision in the immediate aftermath of the surgery, but this should improve with time. It may take a few weeks for your vision to stabilize, and complete recovery can take months.
-
Lifestyle: For patients who had a gas bubble inserted, it may be necessary to maintain specific head positions to help the retina heal. This is typically only for a short period after surgery.
-
Work and activities: Depending on your job and daily activities, you may need to take time off work or avoid certain tasks (like driving) for a few weeks.
Once the eye has healed and follow-up tests confirm that the surgery was successful, most patients can resume their normal activities.
9. Can I drive after Vitrectomy?
After vitrectomy, it's important to avoid driving until your vision stabilizes and you have received clearance from your doctor. In the early stages of recovery, your vision may be blurry, and your eye may be sensitive to light, making it unsafe to drive.
-
Your doctor will advise when it's safe for you to resume driving based on your recovery progress and vision.
-
It's essential to have someone available to help you with transportation during the recovery period.
10. What are the long-term outcomes of Vitrectomy?
Long-term outcomes of vitrectomy vary depending on the underlying condition that required the surgery, as well as individual factors such as overall eye health and adherence to recovery protocols. In general:
-
Vision improvement: Many patients experience a significant improvement in vision, particularly when treated early for conditions like retinal detachment or macular holes.
-
Prevention of further complications: Vitrectomy can help prevent further vision loss or complications in the future, particularly if the disease is progressive, like diabetic retinopathy.
-
Retina health: Once the retinal problem is treated, and healing takes place, the risk of further retinal detachment or complications is reduced. However, regular follow-up visits are essential to monitor the eye for potential problems.
While vitrectomy may not always restore perfect vision, it can substantially improve quality of life and prevent irreversible damage to the retina and vision.


