Introduction to Voice Restoration Surgery (Thyroplasty)
Voice restoration surgery, often referred to as Thyroplasty, is a surgical procedure designed to restore the function of the vocal cords (also known as vocal folds) in individuals who suffer from voice disorders, such as vocal cord paralysis, atrophy, or scarring. The surgery is performed to improve the quality, strength, and pitch of the voice by addressing issues related to vocal fold dysfunction.
The vocal cords are two small muscles in the larynx (voice box) that vibrate to produce sound when air passes through them. In certain conditions, these vocal cords do not vibrate properly or do not meet in the middle when a person tries to speak. This can result in a breathy, weak, or even incoherent voice. In such cases, thyroplasty is a crucial intervention to restore proper vocal fold positioning and function, improving speech quality.
There are several types of Thyroplasty, including Type I (Medialization), Type II (Lateralization), Type III (Relaxation), and Type IV (Lengthening), each addressing different underlying causes of voice disorders. The most common use of Thyroplasty is for vocal cord paralysis, where one of the vocal cords is immobile due to nerve injury or other causes. The procedure involves placing an implant into the thyroid cartilage to push the paralyzed vocal fold toward the midline, enabling better closure and voice production. This approach significantly improves the strength and clarity of speech, enabling individuals to communicate more effectively.
Voice restoration surgery can help people regain their confidence, vocal strength, and quality of life, particularly those who rely on their voice for professional use or personal communication. The procedure is commonly recommended when non-surgical treatments, such as speech therapy or injections, fail to achieve desired results.
Causes and Risk Factors of Voice Dysfunction (Thyroplasty Indications)
Voice dysfunction that requires thyroplasty can be caused by a variety of factors, some of which are medical, while others may be due to injury or trauma. Here are the most common causes:
Vocal Cord Paralysis
Vocal cord paralysis is a primary cause of thyroplasty. It occurs when the nerve controlling one or both vocal cords is damaged, preventing the vocal cords from moving properly. This condition may result from:
-
Surgical complications (e.g., thyroid or neck surgery)
-
Neck trauma or injury
-
Neurological diseases like stroke, Parkinson's disease, or multiple sclerosis
-
Tumors or cancers affecting the neck or chest
In unilateral vocal cord paralysis, only one cord is affected, but the other can compensate somewhat. However, bilateral paralysis (both vocal cords) significantly impairs speech and breathing, often requiring thyroplasty.
Glottic Insufficiency
Glottic insufficiency occurs when the vocal cords cannot meet in the middle to form an airtight seal. This is usually due to:
-
Aging and vocal fold atrophy, where the vocal cords lose muscle mass and elasticity.
-
Scarring or injury to the vocal cords after surgery, intubation, or trauma.
-
Paralysis or nerve damage, which prevents proper cord movement.
When the vocal cords cannot come together fully, patients experience a breathy or weak voice. Medialization thyroplasty can correct this by positioning the vocal cords in a way that they meet properly.
Voice Pitch Abnormalities
Some individuals need pitch-modifying thyroplasty, which adjusts the tension or length of the vocal cords to raise or lower the voice. This is useful for people who experience:
-
High-pitched voices, which may be the result of vocal cord tension issues.
-
Gender-affirming voice surgery, where patients may wish to lower or raise their pitch to align with their gender identity.
Vocal Fold Atrophy (Age-Related)
As individuals age, their vocal cords naturally become thinner and weaker, leading to vocal fold atrophy. This condition reduces the vocal cords' ability to close completely, resulting in:
-
Hoarseness or a weak voice.
-
Difficulty with vocal projection and voice endurance.
-
Increased effort to produce sound or speak for long periods.
Thyroplasty can reposition the vocal cords to ensure better closure and improve vocal strength.
Trauma and Injury
Injury to the neck or larynx can damage the vocal cords or the structures surrounding them, leading to conditions that impair vocal cord function. Trauma can result in:
-
Vocal cord scarring, leading to permanent changes in the voice.
-
Vocal cord paralysis from nerve damage.
-
Hematomas or swelling affecting vocal cord movement.
Thyroplasty may be necessary to correct the damage and restore normal vocal cord function.
Symptoms and Signs — Indicating the Need for Thyroplasty
Patients who may require thyroplasty typically present with the following symptoms, which indicate that their vocal cords are not functioning properly:
1. Hoarseness or Breathy Voice
A hoarse, breathy, or weak voice is one of the most common signs that vocal cord function is impaired. This may be caused by a vocal cord paralysis or glottic insufficiency, where the cords cannot fully close.
2. Difficulty Speaking or Fatigue
Patients may experience vocal fatigue — their voice may tire quickly or become weak after speaking for a short time. Individuals with vocal fold atrophy or vocal cord paralysis find it difficult to speak at normal volume, and their voice may become exhausted after talking for an extended period.
3. Difficulty Swallowing (Dysphagia)
When the vocal cords do not close properly, it can lead to aspiration (food or liquid entering the windpipe), which can cause choking or difficulty swallowing. This is a serious symptom and may require immediate attention, as it can lead to pneumonia or other complications if not addressed.
4. Lack of Vocal Projection
Patients may also experience a reduced vocal range, where they are unable to project their voice adequately in public or noisy environments. The voice may sound muffled or strained, particularly in social or professional settings where effective communication is crucial.
5. Inability to Reach Certain Pitch
Individuals with abnormal vocal pitch — too high or too low — may also require pitch-modifying thyroplasty. This is common in those undergoing gender-affirming surgery or those suffering from abnormal tension or vocal fold anomalies.
Diagnosis of Thyroplasty: How is the Need for Surgery Determined?
Before recommending thyroplasty, an ENT (Ear, Nose, and Throat) specialist will perform several diagnostic tests to determine the underlying cause of vocal cord dysfunction:
1. Clinical Evaluation
The first step is a clinical evaluation, where the doctor will assess the patient's voice and ask about the symptoms, duration, and functional impact on daily life. The specialist will also review the patient's medical history, including any previous surgeries, injuries, or medical conditions.
2. Laryngoscopy and Videolaryngostroboscopy
The most common diagnostic tool is laryngoscopy, where a flexible scope is inserted into the throat to directly view the vocal cords. This allows the doctor to assess:
-
Vocal cord mobility during speech.
-
Vocal cord position (whether they are in the midline or not).
-
Glottic closure — whether the cords meet fully when speaking.
Videolaryngostroboscopy may also be used to capture detailed images of the vocal cords' movement during speech, helping identify abnormalities such as vocal cord paralysis or scarring.
3. Voice Assessment
A voice assessment by a speech-language pathologist (SLP) is an essential part of the diagnosis. The SLP evaluates:
-
Pitch, loudness, and quality of the voice.
-
Vocal endurance and any signs of vocal fatigue.
-
Speech intelligibility and resonance.
This helps determine the degree of impairment and whether surgery is necessary to restore normal voice function.
4. Imaging Studies (If Necessary)
In some cases, imaging tests such as CT scans or MRI may be used to assess the laryngeal structures, especially if there is suspicion of tumors or other structural issues that could affect vocal cord function.
Treatment Options for Voice Restoration Surgery (Thyroplasty)
There are several types of thyroplasty procedures, depending on the patient's condition and the specific issue with the vocal cords:
1. Medialization Thyroplasty
This is the most common type of thyroplasty, used for unilateral vocal cord paralysis or glottic insufficiency. During this procedure, the surgeon creates a small incision in the neck and inserts a silicone implant into the larynx to push the paralyzed vocal cord toward the midline. This allows the paralyzed cord to meet the functioning cord, improving voice quality and vocal strength.
2. Laryngeal Framework Surgery
In this procedure, the surgeon adjusts the framework of the larynx to improve vocal cord alignment. This is typically used for more complex cases of bilateral vocal cord paralysis or posterior glottic insufficiency, where medialization alone may not be sufficient.
3. Pitch Modifying Thyroplasty
Pitch modifying thyroplasty is used to raise or lower the voice pitch, depending on the patient's needs. This is particularly useful in patients undergoing gender-affirming surgery or those with abnormal pitch issues. The procedure alters the tension and length of the vocal cords, resulting in a higher or lower voice.
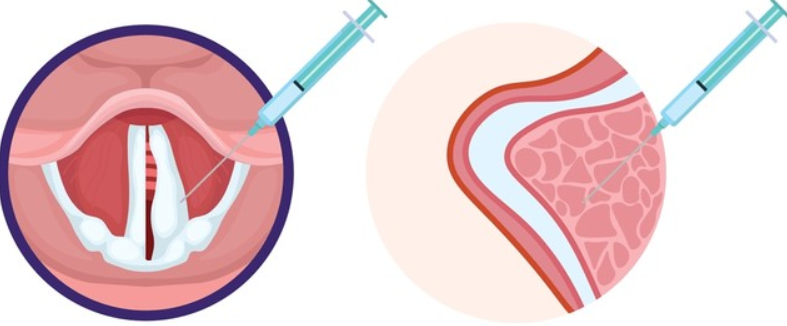
4. Injection Laryngoplasty
For some patients, an initial injection laryngoplasty (temporary injections of collagen, fat, or other substances) may be used to bulk up the vocal cords and improve their function. This can serve as a diagnostic tool or as a temporary solution before committing to more permanent thyroplasty.
Prevention and Management of Thyroplasty-Related Issues
1. Pre-Surgery Considerations
Before undergoing thyroplasty, it is important for patients to undergo a full voice evaluation, including diagnostic tests and a comprehensive medical history review. Patients should also be informed of the procedure's benefits, risks, and recovery process. Smoking cessation and avoiding voice strain in the weeks leading up to surgery are crucial for optimal healing.
2. Post-Operative Care
Post-operative care is essential for ensuring the success of the procedure:
-
Voice Rest: Complete voice rest for a few days after surgery is critical for proper healing and to prevent further strain on the vocal cords.
-
Follow-up Visits: Regular follow-up appointments are necessary to assess the voice and determine if any revisions are needed.
-
Voice Therapy: After surgery, patients are often referred to a speech therapist to help with voice rehabilitation and teach proper vocal techniques.
3. Long-Term Management
After recovering from surgery, patients should be mindful of voice hygiene to avoid future problems. This includes staying hydrated, avoiding excessive voice use, and speaking at appropriate volumes. Patients with vocal cord paralysis or other chronic conditions should have regular check-ups with their ENT specialist to monitor for any changes.
Complications of Thyroplasty
As with any surgery, there are potential risks and complications associated with thyroplasty:
-
Infection at the surgical site.
-
Implant displacement or migration, leading to poor voice quality.
-
Bleeding or swelling around the larynx.
-
Voice changes, including an unnatural or strained voice.
-
Breathing difficulties due to airway changes.
While these complications are rare, it is important for patients to follow post-operative care instructions and attend follow-up appointments to ensure the procedure's success.
Living with Voice Restoration Surgery (Thyroplasty)
1. Recovery and Rehabilitation
Recovery after thyroplasty typically takes several weeks. Patients will need to follow specific post-operative instructions, such as voice rest, avoiding strenuous activities, and attending regular follow-up visits. Many patients benefit from voice therapy to strengthen their voice and improve vocal function after the surgery.
2. Long-Term Outcomes
For most patients, thyroplasty results in significant improvements in voice quality, endurance, and clarity. Patients can generally return to their normal activities within a few weeks to a few months, depending on the type of procedure performed and their overall health.
Top 10 Frequently Asked Questions about Voice Restoration Surgery (Thyroplasty)
1. What is Thyroplasty (Voice Restoration Surgery)?
Thyroplasty is a surgical procedure designed to improve or restore voice function. It involves altering the framework of the larynx (voice box) to improve the positioning or tension of the vocal cords. This surgery is typically performed when there are issues with vocal cord paralysis, atrophy, or other structural problems that prevent the vocal cords from coming together properly. By using implants or other devices, the surgeon can correct the position of the vocal cords, which helps produce a clearer, stronger voice. Thyroplasty can also be used to adjust the pitch or tone of the voice depending on the patient's needs.
2. Who Needs Thyroplasty — What Conditions Does It Treat?
Thyroplasty is primarily used to treat vocal cord paralysis or weakness, a condition where one or both vocal cords fail to function properly. It may also be recommended for:
-
Vocal cord atrophy, where the vocal cords lose their bulk and cannot vibrate effectively.
-
Unilateral vocal cord paralysis, which occurs when one vocal cord is paralyzed and cannot move toward the midline to meet the opposite vocal cord, causing a weak, breathy voice.
-
Glottic insufficiency, where the vocal cords fail to completely close, leading to air leakage during speech.
-
Improvement of voice quality in individuals with voice disorders due to aging, trauma, or prior surgeries like thyroidectomy.
-
Voice pitch correction, if a patient seeks to raise or lower their vocal pitch for medical or personal reasons.
Thyroplasty is often considered when less invasive treatments (like voice therapy or injections) have not been effective.
3. What Are the Different Types of Thyroplasty?
There are several types of thyroplasty, each designed for specific conditions:
-
Type I (Medialization Thyroplasty): The most common type, where an implant is used to bring a paralyzed or weakened vocal cord closer to the midline, improving voice quality and reducing breathiness. This is often used in cases of unilateral vocal cord paralysis.
-
Type II (Lateralization Thyroplasty): This type moves the vocal cords apart, typically done when the airway needs to be enlarged or when there's a need to reduce the tension on the vocal cords.
-
Type III (Shortening Thyroplasty): This technique shortens the vocal cords and is used to lower the pitch of the voice, useful for patients who wish to achieve a deeper voice.
-
Type IV (Lengthening Thyroplasty): In this procedure, the vocal cords are lengthened, and it is typically used to raise the pitch of the voice, often used in patients looking for a higher voice.
The type of thyroplasty recommended will depend on the specific issue with the vocal cords and the desired outcome.
4. How Is Thyroplasty Performed?
Thyroplasty is typically done under local anesthesia with sedation, though some cases may require general anesthesia. The procedure is usually performed through a small incision in the neck to access the larynx. Once the surgeon has access to the vocal cords:
-
A small window is made in the thyroid cartilage (the "Adam's apple" area).
-
The surgeon may insert an implant (usually made of silicone, Gore-Tex, or another material) or reposition the cartilage of the larynx to correct the position of the vocal cords.
-
The surgeon may also make adjustments to improve the tension of the vocal cords, depending on the type of thyroplasty being performed.
-
After the implant or adjustment is made, the incision is closed, often without the need for sutures, depending on the size of the incision.
The surgery typically takes about 1-2 hours, and patients are usually discharged the same day or after a short stay in the hospital for observation.
5. What Benefits Can Patients Expect After Thyroplasty?
After successful thyroplasty, most patients experience:
-
Improved voice quality: Voice becomes stronger, clearer, and more stable, with reduced breathiness and strain.
-
Better vocal cord closure: If vocal cord paralysis or insufficiency was an issue, this procedure allows the vocal cords to come together properly, improving phonation.
-
Improved swallowing and airway function: In cases where vocal cord dysfunction had impacted swallowing or breathing, patients may experience better control and reduced risk of aspiration.
-
Pitch and tone adjustment: For those seeking a change in voice pitch, the procedure can raise or lower the voice to meet the desired tone.
These improvements can significantly impact quality of life, especially for individuals whose voice was previously a source of distress or functional limitation.
6. What Are the Risks and Possible Complications of Thyroplasty?
As with any surgery, there are some risks associated with thyroplasty:
-
Infection: Though rare, there is a risk of infection at the incision site.
-
Swelling and bruising: Mild swelling or bruising around the neck may occur after the surgery.
-
Voice changes: In some cases, the desired voice outcome may not be achieved, or the voice may sound too unnatural or strained.
-
Implant problems: The implant may shift, extrude, or fail to provide the desired result, requiring additional surgery.
-
Nerve damage: There's a small risk of injury to the nerves around the vocal cords, which could affect voice quality or cause temporary hoarseness or breathing issues.
-
Scarring: Permanent scarring around the incision or on the vocal cords may affect the voice.
Though these complications are rare, it is essential for patients to fully understand the risks and discuss them with their surgeon before undergoing the procedure.
7. What Is the Recovery Process Like After Thyroplasty?
The recovery process after thyroplasty is relatively straightforward, but it does require attention to detail:
-
Immediate aftercare: Patients are typically monitored in the hospital for a few hours after surgery to ensure there are no immediate complications, such as bleeding or airway issues.
-
Voice rest: It's crucial for patients to rest their voice for several days following surgery. Talking, whispering, or straining the voice should be avoided during this time to allow the vocal cords to heal properly.
-
Swelling and discomfort: Mild swelling and discomfort in the neck area are common, but this generally subsides within a week.
-
Follow-up care: Patients will need to visit their doctor for follow-up appointments to assess how the voice is healing and ensure that the implant is in the correct position.
-
Gradual return to normal activities: Most patients can return to work and normal activities within a few days, but strenuous physical activities should be avoided for at least a week or until cleared by the surgeon.
Full voice recovery may take several weeks, with patients often beginning speech therapy to optimize the new vocal function.
8. Will My Voice Ever Return to Normal After Thyroplasty?
While thyroplasty can significantly improve voice quality, the exact outcome depends on the individual's condition and the success of the surgery. In many cases, patients experience dramatic improvements in their voice, returning to a more natural and functional level. However, complete restoration to pre-condition voice quality may not always be achievable, especially if there has been significant long-term damage to the vocal cords.
Voice rehabilitation through speech therapy after surgery can help maximize the benefits of thyroplasty and help the patient adjust to their new vocal capabilities.
9. Is Thyroplasty a Permanent Solution?
Yes, for most patients, thyroplasty provides a permanent solution to the problem of vocal cord paralysis or insufficiency. The implant or adjustments to the larynx typically remain in place, and many patients enjoy long-term improvements. However, some patients may experience implant shifting or scar tissue formation that can require adjustments or further surgery, though this is relatively rare.
Continual care and regular follow-up visits with the surgeon are important to ensure that the surgical outcome is maintained and to monitor for any late-onset issues.
10. Who Is an Ideal Candidate for Thyroplasty?
Ideal candidates for thyroplasty are individuals with vocal cord paralysis, vocal fold insufficiency, or significant voice disorders that affect daily function, speech, or swallowing. Specifically:
-
Those with unilateral vocal cord paralysis (paralysis of one vocal cord) where the vocal cords cannot come together properly.
-
People with hoarseness, breathiness, or weak voice due to aging or other medical conditions, where voice therapy has not been effective.
-
Patients who have specific functional voice needs (e.g., public speakers, singers, professionals) who wish to improve vocal projection or quality.
It is important for patients to be in good overall health, understand the risks and benefits of the surgery, and have realistic expectations for the outcomes.


