Introduction to Vulval Lesion Excision
Vulval lesions refer to abnormal growths, bumps, or areas of irritation on the vulva, which is the external part of the female genital area. These lesions may be benign or, in some cases, indicative of a more serious condition, such as pre-cancerous or cancerous lesions. Lesions can develop for various reasons and may present in different forms, ranging from cysts, warts, and benign skin conditions to more complex issues like vulvar cancer or pre-cancerous changes.
What is Vulval Lesion Excision?
Vulval lesion excision is a surgical procedure in which abnormal tissue growths
on the vulva are removed. The excision can be either simple, where only the
lesion is removed, or more extensive when the lesion is pre-cancerous or
cancerous, requiring wider margins of tissue to be excised for safety.
Why is Vulval Lesion Excision Important?
Lesion excision plays a crucial role in the treatment and management of vulvar
health. For benign conditions, excision may be needed to alleviate symptoms like
pain, itching, or discomfort, especially if the lesion interferes with daily
activities, hygiene, or sexual health. In cases of malignancy or precancerous
changes, excision is essential to remove the lesion and prevent its progression
into cancer.
Causes and Risk Factors of Vulval Lesions
The vulva is a sensitive area prone to several dermatological conditions, infections, and neoplastic changes. Vulval lesions can arise from various causes, ranging from harmless cysts to more serious pre-cancerous or cancerous growths. Understanding these causes and their risk factors is essential in identifying the lesions early and choosing the right treatment.
1. Benign Conditions
-
Cysts: These are common benign lesions that often form when hair follicles or sebaceous glands become blocked. Examples include Bartholin's cysts, which develop near the vaginal opening, or epidermal cysts that are typically small, painless lumps.
-
Skin tags: These soft, non-cancerous growths on the skin are commonly found on the vulva and can result from friction or irritation. Skin tags are generally harmless but may cause discomfort if they get irritated.
-
Warts (HPV-related): Human papillomavirus (HPV) infection is a leading cause of warts in the genital area. Genital warts are typically caused by low-risk strains of HPV and can appear as raised, flesh-colored bumps. While they are non-cancerous, persistent HPV infections can sometimes lead to cervical, vulvar, or vaginal cancers.
2. Chronic Inflammatory and Dermatological Conditions
-
Lichen sclerosus: This is a long-term (chronic) condition that causes thin, white patches of skin on the vulva. The affected area can become itchy, painful, and scarred, making it an important condition to diagnose and manage early.
-
Lichen planus: Another chronic inflammatory condition that affects the skin and mucous membranes, including the vulva. Lichen planus can cause purple, itchy lesions and pain during sexual activity, and it may lead to scarring.
-
Vulvar dermatitis: This includes eczema or allergic reactions that cause irritation and inflammation in the vulvar area, often resulting in redness, scaling, and itching.
3. Pre-cancerous and Cancerous Conditions
-
Vulvar intraepithelial neoplasia (VIN): This is a precancerous condition where abnormal cell growth occurs on the vulvar skin. It is classified into grades (I, II, and III) based on severity, with higher-grade VIN lesions having a higher risk of progressing to vulvar cancer.
-
Vulvar cancer: This is a rare form of cancer that affects the vulva. It typically presents as a lump, ulcer, or thickening of the skin in the vulvar area and may be associated with symptoms like bleeding, itching, or pain.
4. Infectious Causes
-
Herpes simplex virus (HSV): Genital herpes caused by HSV can create painful blisters or sores on the vulva, which may resemble ulcers or lesions.
-
Bacterial infections: Infections, such as those caused by Staphylococcus or Streptococcus bacteria, can lead to abscesses or painful lumps that may require drainage and excision.
5. Risk Factors for Vulval Lesions
-
Age: The risk of developing vulvar cancer increases with age, particularly in post-menopausal women.
-
HPV infection: Persistent infection with high-risk strains of HPV is a major risk factor for developing pre-cancerous or cancerous lesions on the vulva.
-
Weakened immune system: Women with compromised immune systems (e.g., due to HIV/AIDS or immunosuppressive medications) are at a higher risk for vulvar lesions, particularly those caused by HPV.
-
Chronic irritation or trauma: Repeated friction or irritation (from tight clothing, poor hygiene, or scratching) may increase the risk of benign lesions or exacerbate pre-existing conditions.
Symptoms and Signs of Vulval Lesions
Vulval lesions can vary significantly in appearance and symptoms depending on their underlying cause. Below are common signs and symptoms that may indicate the presence of a vulval lesion:
Common Symptoms
-
Itching: Persistent vulvar itching (pruritus) is one of the most common complaints and can be associated with both benign and malignant lesions.
-
Pain and discomfort: Pain, especially during sexual activity (dyspareunia) or when sitting for prolonged periods, can result from lesions that involve the skin or deeper tissues.
-
Visible growths or lumps: Lesions may appear as small bumps, lumps, warts, or ulcers on the vulva, and they may be either painless or tender.
-
Changes in skin texture: The skin on the vulva may become thickened, red, inflamed, or white, especially in cases of lichen sclerosus or other inflammatory conditions.
-
Bleeding or discharge: Unexplained bleeding or abnormal discharge from the vulva may be indicative of a lesion that requires further evaluation.
-
Sores or ulcers: Open sores that do not heal over time, especially if they are painful or bleeding, should be evaluated for the possibility of cancer or infection.
Diagnosis of Vulval Lesions
Accurate diagnosis is essential to determine the appropriate treatment for vulval lesions. Diagnosis typically involves a combination of physical examination, medical history review, and laboratory tests. Here's what the diagnostic process typically looks like:
1. Physical Examination and History
-
The doctor will perform a thorough visual inspection of the vulva, looking for any abnormalities such as growths, discoloration, or lesions.
-
They will ask about symptoms such as itching, pain, bleeding, or changes in the appearance of the vulva.
-
Your gynecologist or dermatologist will also inquire about any risk factors, such as HPV exposure or a history of vulvar skin conditions.
2. Biopsy
-
If a lesion looks suspicious or has not responded to treatment, a biopsy may be necessary. This involves taking a small sample of the lesion for analysis under a microscope.
-
The biopsy helps determine whether the lesion is benign, pre-cancerous, or cancerous, and guides the next steps in treatment.
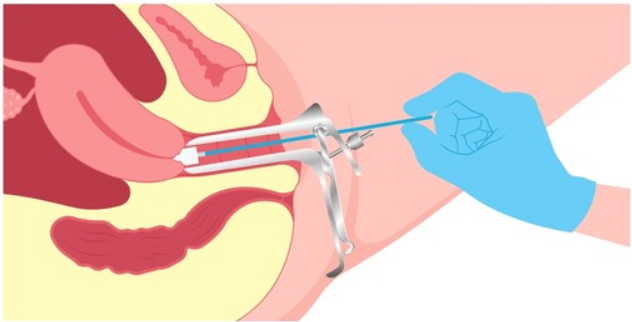
3. Colposcopy
-
A colposcope is an instrument used to closely examine the vulva, vagina, and cervix. It is especially useful for detecting abnormal areas that may require a biopsy.
4. Additional Tests
-
In some cases, further imaging studies, such as ultrasound or MRI, may be recommended if the lesion is suspected to involve deeper tissues.
-
HPV testing may also be done to check for the presence of high-risk strains of the virus, especially in women with a history of abnormal Pap smears or those at higher risk for vulvar cancer.
Treatment Options for Vulval Lesion Excision
Treatment options for vulval lesions vary based on the type, size, and location of the lesion, as well as whether it is benign or malignant. Here are the most common approaches:
1. Conservative Management
-
Topical treatments: For benign conditions like warts, creams or ointments (e.g., imiquimod or podophyllin) may be used to shrink or eliminate the lesions.
-
Observation: In cases where the lesion is small and asymptomatic, a "watch and wait" approach may be employed, with regular follow-ups to monitor the lesion for changes.
2. Surgical Excision
-
Local excision: Small, benign lesions can often be removed under local anesthesia. The lesion is excised along with a small margin of surrounding tissue, and the wound is closed with sutures.
-
Wide local excision (WLE): For pre-cancerous or cancerous lesions, WLE is performed to remove the lesion along with a wider margin of healthy tissue to ensure complete excision of abnormal cells.
-
Laser surgery: In some cases, lasers may be used to remove or shrink vulvar lesions, particularly warts or small tumors. This method is less invasive than traditional excision and has a faster recovery time.
3. Postoperative Care and Follow-up
-
After the excision, patients will need to follow specific wound care instructions to prevent infection and promote healing.
-
Regular follow-up visits will be necessary to check for recurrence of lesions or any signs of complications.
Prevention and Management of Vulval Lesions
While not all vulval lesions are preventable, there are several strategies for managing and minimizing the risk of developing lesions:
1. Regular Gynecological Examinations
-
Routine gynecological check-ups, including annual Pap smears, are essential for early detection of cervical, vaginal, or vulvar abnormalities. Women should also have their vulvar skin examined during these visits.
2. Safe Practices to Reduce HPV Risk
-
HPV is a major risk factor for vulvar cancer, so vaccination against HPV is recommended for young women and those at risk. Additionally, practicing safe sex (e.g., using condoms) can reduce the risk of HPV infection.
3. Proper Hygiene and Skin Care
-
Maintaining good vulvar hygiene, wearing loose, breathable clothing, and avoiding harsh soaps can help prevent irritation and lesions caused by friction, inflammation, or dermatitis.
4. Avoiding Chronic Irritation
-
Women with conditions like lichen sclerosus or other dermatologic issues should take extra care to avoid skin irritation and follow appropriate treatments to manage flare-ups and prevent complications.
Complications of Vulval Lesions & Risks Associated with Excision
While vulval lesion excision is a relatively safe procedure, there are some potential complications:
-
Infection: As with any surgery, there is a risk of infection at the excision site, especially if proper wound care is not followed.
-
Scarring: Some scarring is inevitable, particularly with wide excision. This may affect the appearance or elasticity of the vulva.
-
Recurrence: In some cases, lesions may recur, particularly if they were not completely excised or if underlying risk factors remain.
-
Pain and discomfort: Some pain, swelling, and discomfort are expected after the procedure, though this should subside as the wound heals.
-
Nerve damage: In rare cases, nerve damage during excision may lead to altered sensation in the vulvar area.
Living with Vulval Lesions Before and After Excision
Living with vulval lesions can be emotionally and physically challenging, especially if the lesion affects sexual health, self-esteem, or quality of life. However, with appropriate care, many women can successfully manage vulval lesions.
Before Excision:
-
Emotional and psychological support: Women may feel anxiety, shame, or embarrassment due to the appearance or symptoms of vulval lesions. Encouraging open communication with healthcare providers and providing reassurance that these conditions are treatable can help.
-
Managing symptoms: Symptomatic treatment for itching, pain, or irritation can help women cope until the excision is performed.
After Excision:
-
Healing and recovery: After excision, most women recover fully, but they must follow proper post-operative care instructions to avoid complications.
-
Emotional recovery: It may take time for some women to heal emotionally after excision, particularly if the lesion was pre-cancerous or malignant. Counseling or support groups may help.
Top 10 Frequently Asked Questions about Vulval Lesion Excision
1. What is Vulval Lesion Excision?
Vulval lesion excision is a surgical procedure to remove abnormal growths or lesions from the vulva, which is the external part of the female genitalia. Lesions can include warts, moles, skin tags, ulcers, cysts, or any unusual growths. The excision is typically done to prevent further complications, such as irritation, pain, bleeding, or, in the case of suspicious lesions, to rule out the possibility of cancer. By removing the lesion, the goal is to restore the vulvar area's health, reduce symptoms, and, if necessary, provide a sample for diagnostic purposes (such as a biopsy) to check for abnormal or cancerous cells.
The procedure is usually simple and, in many cases, is done under local anesthesia, with a small incision being made to remove the lesion.
2. Why is Vulval Lesion Excision Performed? What Conditions Does It Treat?
Vulval lesion excision is performed for a variety of reasons, including both medical and cosmetic concerns. Some common reasons for the procedure include:
-
Suspicious or abnormal growths: A lesion may appear abnormal or may not heal with standard treatments, making excision necessary to rule out cancerous or precancerous conditions.
-
Chronic irritation: Some lesions cause persistent irritation, pain, itching, or bleeding. Excision can relieve these symptoms.
-
Functional problems: If the lesion is large and interferes with normal activities like sexual intercourse or hygiene, excision may be recommended.
-
Cosmetic reasons: For patients who are self-conscious about their appearance due to benign lesions, excision can improve the aesthetic appearance of the vulva.
-
Infections or recurring lesions: If the lesion is linked to recurrent infections or persistent conditions like warts or cysts, excision helps in managing these issues.
3. How is the Vulval Lesion Excision Procedure Performed?
Vulval lesion excision is generally performed under local anesthesia, meaning the area is numbed to prevent discomfort during the procedure. In some cases, general anesthesia may be used, especially if the lesion is large or if the patient is undergoing other related procedures. Here's how the procedure typically unfolds:
-
Incision: The surgeon makes a small incision around the lesion to remove it. If necessary, they may remove a small amount of surrounding tissue as well to ensure complete excision, especially if the lesion is suspected to be cancerous or precancerous.
-
Excision: The lesion is carefully excised using a scalpel or other surgical tools.
-
Closure: After the lesion is removed, the wound is typically closed using dissolvable sutures. In some cases, the wound may be left open to heal naturally, depending on the size and location of the excision.
-
Post-operative care: After excision, the area is usually dressed with a bandage, and the patient is advised on how to care for the wound, keep it clean, and avoid irritation.
4. What Are the Expected Benefits and Outcomes After Vulval Lesion Excision?
After the excision of a vulval lesion, most patients can expect several benefits, including:
-
Relief from symptoms: Removal of painful, irritating, or bleeding lesions results in reduced discomfort.
-
Restoration of function: If the lesion interfered with normal activities like sexual intercourse or hygiene, excision helps restore normal function.
-
Aesthetic improvement: Excision may help improve the appearance of the vulva, especially for benign lesions that may be unsightly or bothersome.
-
Prevention of complications: Removing potentially cancerous or precancerous lesions reduces the risk of developing vulvar cancer or other related issues.
-
Improved self-esteem: Many women feel more comfortable with their bodies post-surgery, especially if the lesion caused emotional or psychological distress.
5. What Are the Risks and Possible Complications of the Procedure?
Although vulval lesion excision is generally a safe procedure, there are some potential risks and complications:
-
Infection: There is always a risk of infection at the surgical site, which could delay healing or cause further complications.
-
Scarring: Depending on the size and location of the lesion, excision may result in scarring. However, in most cases, the surgeon will aim to minimize visible scarring.
-
Bleeding: While bleeding is typically minimal, excessive bleeding could occur, especially if the lesion is large or if there's underlying vascularity.
-
Delayed healing: Some wounds may take longer to heal, particularly if the lesion was large or in a sensitive area.
-
Nerve damage: Although rare, there is a small risk of damaging nerves in the area, which could lead to changes in sensation or discomfort.
-
Recurrence of the lesion: If the lesion is not completely excised, there is a chance it could return. This is more common with lesions that are infected or due to recurring conditions like warts.
6. What Is the Recovery Process Like After Vulval Lesion Excision?
The recovery process after vulval lesion excision is usually straightforward, though it varies depending on the size and location of the excision. Most patients can expect:
-
Immediate post-surgery: Mild pain, swelling, and discomfort in the vulvar area for the first few days. Pain can be managed with over-the-counter pain relievers.
-
Hygiene: Keeping the area clean and dry is crucial to prevent infection. Patients are typically advised to wash the area gently with mild soap and water and avoid using scented products or irritants.
-
Activity restrictions: Patients are usually advised to avoid strenuous physical activity, sexual intercourse, and anything that may put pressure on the vulvar area for a few weeks while the area heals.
-
Follow-up care: A follow-up appointment is often scheduled to ensure proper healing and to address any concerns, such as infection or delayed healing.
Full recovery typically takes a few weeks, with patients able to resume normal activities once the area has healed.
7. Will the Surgery Affect My Sexual Health or Future Pregnancies?
In most cases, vulval lesion excision should not affect your sexual health or future pregnancies, especially if the lesion was small and the excision was minor. However, for larger excisions or those in sensitive areas, there may be temporary changes in sensation or discomfort.
-
Sexual health: After full recovery, most women can resume sexual activity with no problems. In some cases, if the lesion was large, the area might feel tender or sensitive for a while, and sexual activity should be avoided until healing is complete.
-
Future pregnancies: The excision of a vulval lesion typically does not affect fertility or the ability to have children. If the surgery is done with proper care and healing, there should be no long-term effects on vaginal or vulvar anatomy during pregnancy.
8. How Should I Prepare for the Surgery?
Before undergoing vulval lesion excision, patients will typically need to:
-
Consult with a surgeon: A thorough consultation to evaluate the lesion, medical history, and discuss the risks and benefits of the surgery.
-
Medical assessment: A pre-surgical checkup may be done to ensure the patient is in good health for surgery. This may include blood tests or screening for conditions like infections.
-
Avoid certain medications: If taking medications that affect bleeding (e.g., blood thinners), patients may be instructed to stop them before surgery.
-
Arrange post-surgery support: Since the procedure is typically done under local anesthesia, patients will need someone to accompany them home afterward, particularly if they are undergoing general anesthesia.
9. Is the Excision Always Necessary, or Are There Alternatives?
While excision is often the most effective treatment for problematic vulval lesions, there are alternatives depending on the type of lesion:
-
Topical treatments: For some benign lesions (such as warts or certain types of dermatitis), topical treatments like ointments or creams may be prescribed.
-
Laser therapy: Certain lesions, especially warts or precancerous growths, can be treated with laser therapy.
-
Cryotherapy: Freezing the lesion off with liquid nitrogen is another alternative for benign lesions like warts.
-
Monitoring: In cases where the lesion is small and asymptomatic, doctors may recommend a “watch and wait” approach, with regular follow-ups to monitor for any changes.
10. What Can I Expect in Terms of Long-Term Outcomes?
After a successful vulval lesion excision, the long-term outcomes are generally positive. Patients typically experience:
-
Improved comfort and function: The removal of the lesion often resolves symptoms like irritation, pain, or swelling.
-
Reduced risk of cancer: If the lesion was precancerous, excision significantly lowers the risk of it developing into vulvar cancer.
-
Good cosmetic results: Most patients report satisfaction with the appearance of the vulva after healing, with minimal scarring.
-
Long-term monitoring: For lesions that were cancerous or precancerous, long-term follow-up with your healthcare provider is crucial to ensure there is no recurrence.


