Introduction to Pineal Parenchymal Tumors of Intermediate Differentiation
Pineal Parenchymal Tumors of Intermediate Differentiation (PPTID) are rare, primary tumors that originate in the pineal gland, an essential part of the brain located in the epithalamus. These tumors arise from the pineal parenchymal cells, which are responsible for the production of melatonin and regulate the body's circadian rhythms. PPTID is a form of neuroepithelial tumor and typically represents an intermediate stage in the pineal tumor classification system—falling between the benign pineocytomas and the malignant pineoblastomas.
The classification and diagnosis of PPTIDs are challenging due to the tumor's heterogeneous nature and the overlap in histological features with other types of tumors. These tumors are considered Grade II-III according to the World Health Organization (WHO) classification, representing tumors with intermediate differentiation. Because of their rarity and complex behavior, PPTIDs require specialized treatment approaches involving surgery, radiotherapy, and sometimes chemotherapy.
Causes and Risk Factors of Pineal Parenchymal Tumors of Intermediate Differentiation
The exact cause of PPTIDs remains largely unknown, but several potential factors have been implicated in the development of these tumors. Understanding these factors is important for early detection and treatment.
Genetic Factors:
-
Sporadic Mutations: Most cases of PPTIDs occur sporadically, meaning there are no clear hereditary links. However, genetic mutations in certain tumor suppressor genes may increase the likelihood of developing PPTID.
-
Genetic Syndromes: Though rare, certain inherited conditions may predispose individuals to develop pineal tumors. These include:
-
Li-Fraumeni Syndrome: Caused by mutations in the TP53 gene, which increases susceptibility to a variety of cancers, including pineal parenchymal tumors.
-
Neurofibromatosis type 1 and 2: Genetic conditions that may predispose individuals to brain and spinal tumors, including those affecting the pineal gland.
-
Von Hippel-Lindau Disease (VHL): Mutations in the VHL gene can lead to the formation of various types of tumors, including those in the brain.
-
Environmental and Lifestyle Factors:
-
Ionizing Radiation: Exposure to radiation therapy or environmental radiation, particularly in childhood, is one of the known risk factors for developing brain tumors, including PPTIDs. The pineal gland is sensitive to radiation, and prolonged exposure may increase the risk of abnormal cell growth.
-
Age and Sex: PPTIDs can develop at any age, but they are most commonly diagnosed in adults aged 30-50 years. The incidence appears to be slightly higher in males than females.
Cellular Abnormalities:
In some cases, abnormalities in the cellular differentiation process of the pineal gland can lead to the development of these tumors. Impaired differentiation during cell division may cause the development of poorly differentiated or undifferentiated cells, which can result in tumor formation.
Symptoms and Signs of Pineal Parenchymal Tumors of Intermediate Differentiation
PPTIDs present with a variety of symptoms, many of which are related to the mass effect of the tumor or its effects on surrounding brain structures. Symptoms may be gradual or sudden, depending on the tumor's size and location. These tumors often cause increased intracranial pressure (ICP), which can lead to a range of neurological symptoms.
Common Symptoms of PPTIDs:
-
Headache: A frequent symptom due to increased
intracranial pressure. The headache can be severe and
persistent.
-
Nausea and Vomiting: Often associated with elevated ICP
and caused by obstructive hydrocephalus, where the
tumor blocks the normal flow of cerebrospinal fluid (CSF).
-
Vision Problems: Visual disturbances, including
double vision (diplopia) or upward gaze
palsy, are common due to compression of the tectal
plate of the midbrain.
-
Cognitive Changes: Memory problems, difficulty
concentrating, and personality changes may occur if the tumor affects
nearby brain structures involved in cognition.
-
Balance Issues: Unsteadiness, difficulty walking, or
gait abnormalities may result from the tumor's effect
on the cerebellum and brainstem.
-
Endocrine Dysfunction: Rarely, tumors affecting the
pineal gland can alter the production of melatonin,
leading to sleep disturbances or other hormonal imbalances.
Red Flag Symptoms:
-
Sudden visual changes or loss of
coordination.
-
Severe headache with vomiting that doesn't subside.
-
Seizures or unusual neurological symptoms like
paralysis or numbness.
Headache: A frequent symptom due to increased intracranial pressure. The headache can be severe and persistent.
Nausea and Vomiting: Often associated with elevated ICP and caused by obstructive hydrocephalus, where the tumor blocks the normal flow of cerebrospinal fluid (CSF).
Vision Problems: Visual disturbances, including double vision (diplopia) or upward gaze palsy, are common due to compression of the tectal plate of the midbrain.
Cognitive Changes: Memory problems, difficulty concentrating, and personality changes may occur if the tumor affects nearby brain structures involved in cognition.
Balance Issues: Unsteadiness, difficulty walking, or gait abnormalities may result from the tumor's effect on the cerebellum and brainstem.
Endocrine Dysfunction: Rarely, tumors affecting the pineal gland can alter the production of melatonin, leading to sleep disturbances or other hormonal imbalances.
Sudden visual changes or loss of coordination.
Severe headache with vomiting that doesn't subside.
Seizures or unusual neurological symptoms like paralysis or numbness.
Prompt medical evaluation is essential to diagnose and treat these tumors early.
Diagnosis of Pineal Parenchymal Tumors of Intermediate Differentiation
Diagnosing PPTID requires a multi-step approach, involving clinical evaluation, imaging studies, and tissue biopsy.
1. Clinical Evaluation:
Physicians begin by reviewing the patient's medical history, symptoms, and family history. Neurological examinations to assess motor function, reflexes, and cranial nerve function are crucial.
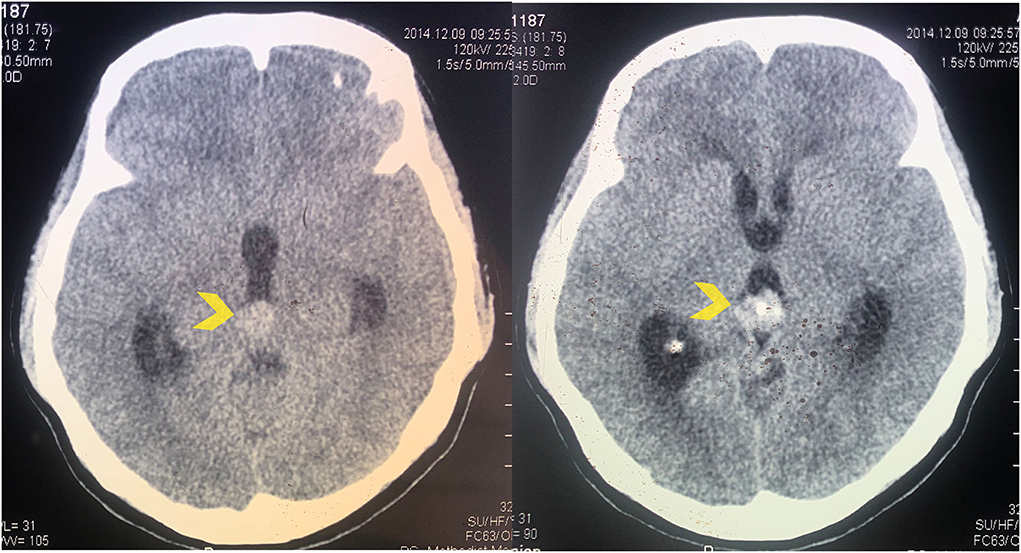
2. Imaging Studies:
The following imaging techniques are commonly used:
-
Magnetic Resonance Imaging (MRI): The gold standard for imaging brain tumors. MRI helps assess the size, location, and extent of the tumor. PPTIDs often appear as well-defined masses that enhance with contrast. They may show calcifications or cystic changes.
-
Computed Tomography (CT): Useful in detecting calcifications and assessing the presence of hydrocephalus or other structural changes in the brain.
-
Positron Emission Tomography (PET): Can be used in cases where malignancy is suspected, to assess the metabolic activity of the tumor.
3. Biopsy and Histopathology:
-
Stereotactic Biopsy: A minimally invasive procedure used to obtain a tissue sample for pathological examination.
-
Histological Examination: The tumor's cellular differentiation, mitotic rate, and degree of atypia are evaluated under a microscope to determine whether the tumor is benign, intermediate, or malignant.
4. Molecular Testing:
Molecular analysis may help identify specific genetic mutations or markers, which can influence treatment decisions. For example, the presence of mutations in DICER1 or RB1 genes may help identify higher-risk tumors.
Treatment Options for Pineal Parenchymal Tumors of Intermediate Differentiation
The treatment of PPTID often involves a multidisciplinary approach combining neurosurgery, radiotherapy, and chemotherapy. The choice of treatment depends on the tumor grade, location, and patient health status.
1. Surgery:
The first line of treatment is typically surgical resection. The goal is to remove as much of the tumor as possible while minimizing damage to surrounding brain structures. However, total resection may not always be feasible due to the tumor's proximity to critical brain regions.
-
Gross Total Resection (GTR): When possible, the complete removal of the tumor is preferred.
-
Subtotal Resection: In some cases, only part of the tumor can be safely removed, particularly if it is located near vital structures.
2. Radiation Therapy:
-
Adjuvant Radiotherapy is recommended if the tumor is not entirely resectable or if there is evidence of malignancy (Grade III). External beam radiation or stereotactic radiosurgery (SRS) may be used for targeted treatment.
-
Radiation is often used for residual or recurrent tumors, with the goal of preventing further tumor growth.
3. Chemotherapy:
-
While chemotherapy is not a first-line treatment for most PPTIDs, it may be used for high-grade tumors or those with metastasis.
-
Chemotherapeutic agents such as etoposide, cisplatin, and vincristine are commonly used in combination to treat aggressive tumors.
4. Emerging Therapies:
-
Targeted Therapy and Immunotherapy: Clinical trials are underway to explore the potential of new drugs and therapies targeting specific tumor pathways in pineal tumors.
Prevention and Management of Pineal Parenchymal Tumors of Intermediate Differentiation
Currently, there are no known prevention strategies for PPTIDs due to the sporadic nature of the disease. However, early diagnosis and treatment play a vital role in managing the disease and improving patient outcomes.
Management Strategies:
-
Regular Monitoring: Lifelong follow-up with MRI scans is often necessary to monitor for recurrence or metastasis, particularly for high-risk patients.
-
Symptom Management: Patients may require medications such as steroids for brain edema, pain management, and anti-seizure drugs if necessary.
-
Rehabilitation: After surgery or treatment, rehabilitation services like physical therapy, occupational therapy, and neuropsychological support can help patients recover physical function and cognitive abilities.
Complications of Pineal Parenchymal Tumors of Intermediate Differentiation
Several complications may arise during the course of PPTID treatment and recovery:
1. Surgical Complications:
-
Infection: As with any brain surgery, there is a risk of infection at the surgical site.
-
Bleeding: Hemorrhage during surgery is a potential risk.
-
Neurological Deficits: Depending on tumor location, patients may experience worsening motor or sensory functions.
2. Radiation Side Effects:
-
Cognitive Decline: Long-term radiation exposure to the brain can lead to cognitive impairments.
-
Radiation Necrosis: A rare but serious complication involving tissue death due to radiation.
3. Recurrence or Metastasis:
-
Some PPTIDs, especially those with a high mitotic rate, can recur after initial treatment, requiring additional therapy.
Living with Pineal Parenchymal Tumors of Intermediate Differentiation
Living with PPTID requires regular monitoring and managing any long-term effects of treatment. Patients should work closely with their healthcare team to optimize their recovery and quality of life.
Follow-Up Care:
-
Regular MRIs are essential to monitor for tumor recurrence or new growth.
-
Cognitive and Physical Rehabilitation may be necessary for patients with neurological deficits after treatment.
Psychosocial Support:
-
Patients may benefit from psychological counseling to help cope with the emotional challenges of cancer treatment.
-
Support groups can provide a sense of community and help reduce feelings of isolation.
Top 10 Frequently Asked Questions about Pineal Parenchymal Tumors of Intermediate Differentiation
1. What are Pineal Parenchymal Tumors of Intermediate Differentiation (PPTID)?
Pineal Parenchymal Tumors of Intermediate Differentiation (PPTID) are rare brain tumors that originate in the pineal gland, a small gland located in the brain responsible for regulating sleep-wake cycles. They are classified as intermediate-grade tumors, meaning they are more aggressive than benign pineal tumors but less aggressive than high-grade malignant tumors.
2. What causes Pineal Parenchymal Tumors of Intermediate Differentiation?
The exact cause of PPTID is unknown. Like other brain tumors, they may result from genetic mutations, abnormal cell growth, or disruptions in cellular signaling pathways in the pineal gland. There are no known environmental or lifestyle factors directly linked to their development.
3. What are the common symptoms of PPTID?
Symptoms of PPTID are often due to pressure on surrounding brain structures and may include:
-
Headaches, often worse in the morning
-
Nausea and vomiting
-
Vision problems or double vision
-
Difficulty with balance or coordination
-
Sleep disturbances
-
Hydrocephalus (fluid accumulation in the brain) in severe cases
Symptoms can vary depending on tumor size and location.
4. How is PPTID diagnosed?
Diagnosis usually involves a combination of:
-
MRI (Magnetic Resonance Imaging): To visualize the tumor and its size/location.
-
CT Scan (Computed Tomography): For bone and structural assessment.
-
Biopsy or Surgical Resection: To obtain tissue for histopathological analysis, which confirms the diagnosis and tumor grade.
-
Neurological evaluation: To assess cognitive, motor, and sensory functions.
5. What are the treatment options for PPTID?
Treatment is multimodal and may include:
-
Surgical resection: Removal of as much tumor as safely possible.
-
Radiation therapy: Often used after surgery to reduce recurrence risk.
-
Chemotherapy: Sometimes used in aggressive cases or when surgery isn't possible.
-
Observation: For small, asymptomatic tumors, in select cases, with regular imaging follow-up.
The treatment plan is personalized based on tumor size, location, and patient health.
6. Can PPTID tumors be completely removed?
Complete surgical removal is the goal whenever possible, but it depends on tumor location and proximity to critical brain structures. Sometimes, only partial resection is feasible, followed by radiation therapy to control residual tumor tissue. The extent of resection can impact prognosis and recurrence risk.
7. What is the prognosis for PPTID?
The prognosis varies depending on:
-
Tumor size and grade
-
Completeness of surgical removal
-
Patient's age and overall health
-
Response to radiation or chemotherapy
PPTID generally has a better prognosis than high-grade pineal tumors but requires long-term monitoring due to potential recurrence.
8. Are PPTID tumors cancerous?
Yes, PPTID is considered a malignant tumor, but it is intermediate-grade, meaning it has a moderate growth rate. While not as aggressive as high-grade malignant pineal tumors, PPTID can spread locally and may recur after treatment, which is why careful follow-up is essential.
9. What are the risks of surgery for PPTID?
Surgery carries risks due to the tumor's location near vital brain structures, which may include:
-
Bleeding or infection
-
Neurological deficits (vision changes, balance issues, or cognitive problems)
-
Cerebrospinal fluid leakage
-
Incomplete tumor removal
A skilled neurosurgeon and advanced imaging techniques help minimize these risks.
10. How can patients manage life after PPTID treatment?
Post-treatment management involves:
-
Regular follow-up imaging to monitor for recurrence
-
Rehabilitation therapies: Physical, occupational, or speech therapy as needed
-
Healthy lifestyle: Balanced diet, adequate sleep, and stress management
-
Psychological support: Counseling or support groups can help with anxiety and coping
-
Medication adherence: For symptom control or adjunct therapy
Long-term monitoring is essential for early detection of recurrence and maintaining quality of life.


