Introduction to Pineoblastoma and Supratentorial Primitive Neuroectodermal Tumors
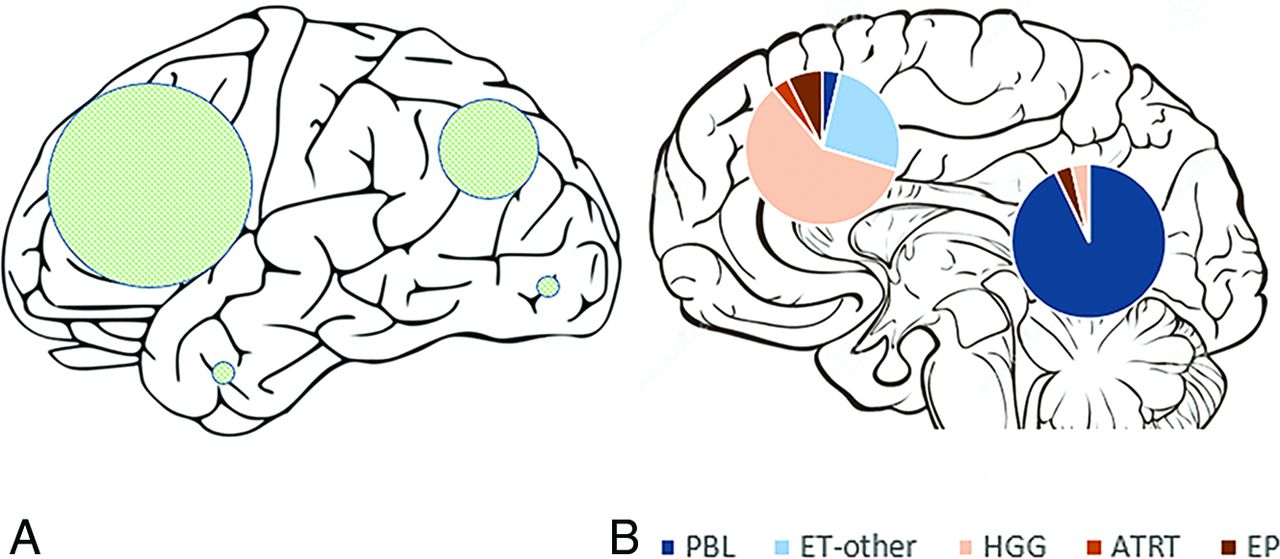
Pineoblastoma and Supratentorial Primitive Neuroectodermal Tumors (PNETs) are two aggressive types of brain tumors that develop in neuroectodermal cells, which are the cells responsible for creating the nervous system. These tumors are part of the broader category known as primitive neuroectodermal tumors (PNETs), which originate from undifferentiated cells and exhibit high malignant potential.
Pineoblastoma:
Pineoblastomas are malignant tumors that arise from the pineal gland, a small endocrine gland located deep within the brain. The pineal gland plays an essential role in producing melatonin, a hormone that regulates sleep-wake cycles. Pineoblastomas are classified as WHO grade IV tumors due to their aggressive nature and potential for metastasis.
Supratentorial PNETs:
Supratentorial PNETs, unlike pineoblastomas, develop in the supratentorial compartment of the brain, which includes the cerebral hemispheres above the tentorium cerebelli. They are usually diagnosed in children and young adults and are often associated with poor prognosis due to their high-grade malignancy. These tumors are referred to as supratentorial due to their location, differentiating them from medulloblastomas (a common PNET that arises in the cerebellum).
Both of these tumors are highly aggressive and difficult to treat, often requiring multidisciplinary care and advanced treatment protocols.
Causes and Risk Factors of Pineoblastoma and Supratentorial PNETs
The exact causes of pineoblastomas and supratentorial PNETs remain poorly understood, but genetic factors, environmental exposures, and age-related factors have been implicated in their development.
Genetic Predispositions:
-
Germline Mutations: Specific genetic mutations or tumor suppressor gene mutations may increase the risk of these tumors. For instance, mutations in TP53 (the tumor suppressor gene) and RB1 (a gene involved in cell cycle regulation) have been identified in some cases.
-
Li-Fraumeni Syndrome: This rare inherited condition is linked to mutations in the TP53 gene, which is involved in regulating the cell cycle and preventing cancer. Individuals with this syndrome are at higher risk for pineoblastomas, among other cancers.
-
Neurofibromatosis Type 1 and 2 (NF1 and NF2): These genetic disorders are known to increase the risk of various CNS tumors, although they are more commonly associated with other types of brain tumors, such as gliomas. Still, individuals with these syndromes may have an increased risk of pineal and supratentorial tumors.
-
Turcot Syndrome: A hereditary condition characterized by the development of brain tumors, including PNETs, along with colorectal cancer.
Environmental Risk Factors:
-
Radiation Exposure: Previous exposure to ionizing radiation, particularly during childhood, is a known risk factor for developing these aggressive brain tumors. Children undergoing radiotherapy for other cancers are at an elevated risk of developing pineoblastomas or PNETs.
-
Environmental Toxins: Though not conclusively proven, certain environmental toxins or chemicals could be linked to an increased risk of brain tumors. Research into the effects of pesticides, industrial chemicals, and pollution on brain cancer remains ongoing.
Age and Sex:
-
Pineoblastomas typically affect children and young adults, with a higher incidence in males than females.
-
Supratentorial PNETs are most commonly diagnosed in children and adolescents, though they can also affect adults. They show a slight male predominance.
Symptoms and Signs of Pineoblastoma and Supratentorial PNETs
Both pineoblastomas and supratentorial PNETs present with similar symptoms due to their location in the brain and the intracranial pressure (ICP) they create. Symptoms may develop gradually, but they can also worsen rapidly as the tumor grows.
Pineoblastoma Symptoms:
-
Headaches: Due to increased ICP, persistent or worsening headaches are common.
-
Nausea and Vomiting: Often associated with increased ICP, these symptoms are typically worse in the morning or when changing positions.
-
Vision Problems: Pineoblastomas often affect the pineal gland, which is located near structures that control eye movement. This can lead to visual disturbances such as double vision, difficulty with upward gaze, or Parinaud syndrome.
-
Balance Issues: Due to pressure on the brainstem, patients may experience coordination problems and difficulty walking.
-
Cognitive and Behavioral Changes: Tumors affecting the pineal gland or surrounding brain regions may cause memory problems, personality changes, or confusion.
-
Seizures: These may occur due to the tumor's involvement with the brain cortex.
Supratentorial PNET Symptoms:
-
Severe Headaches: Like pineoblastomas, supratentorial PNETs can increase ICP, leading to headaches.
-
Nausea and Vomiting: Often the result of obstructed CSF flow due to tumor mass effect.
-
Motor Deficits: Depending on the tumor's location, patients may experience weakness or paralysis in one part of the body.
-
Cognitive Impairment: Memory problems, attention deficits, and changes in thinking ability can occur, especially if the tumor is located in the frontal or temporal lobes.
-
Seizures: As a result of the tumor's impact on the brain's electrical activity.
Diagnosis of Pineoblastoma and Supratentorial PNETs
Diagnosing these tumors typically involves a combination of imaging studies, biopsy, and genetic testing.
1. Imaging Studies:
-
MRI (Magnetic Resonance Imaging): MRI is the gold standard for diagnosing pineoblastomas and supratentorial PNETs. These tumors appear as well-circumscribed masses with contrast enhancement. Pineoblastomas often show calcifications, and both types may show cystic changes or necrosis.
-
CT Scan: A CT scan is useful for detecting calcifications and assessing hydrocephalus (CSF buildup), but MRI provides more detailed images of the tumor.
-
PET Scan: Positron emission tomography (PET) is sometimes used to assess tumor metabolic activity and detect metastasis.
2. Biopsy and Histopathology:
-
Stereotactic Biopsy: A biopsy is usually required to obtain a tissue sample from the tumor for histopathological analysis. This can be performed using neuronavigation or stereotactic techniques.
-
Histological Examination: PNETs, including pineoblastomas, are composed of small, undifferentiated cells. The tumor's characteristics, such as mitotic rate, necrosis, and cellular differentiation, help determine the tumor grade (typically WHO Grade IV for pineoblastomas and Grade III for high-grade PNETs).
-
Immunohistochemistry: Specific markers such as Synaptophysin, Neurofilament protein, and GFAP are often used to confirm the diagnosis.
Treatment Options for Pineoblastoma and Supratentorial PNETs
Treatment of pineoblastomas and supratentorial PNETs requires a multidisciplinary approach, including surgery, radiation therapy, and chemotherapy. The treatment plan is based on the tumor's grade, location, and extent of spread.
1. Surgical Treatment:
-
Gross Total Resection (GTR): Complete surgical removal of the tumor is the treatment of choice if the tumor is operable and does not involve critical brain regions. GTR improves overall survival and reduces recurrence.
-
Subtotal Resection: In cases where complete removal is not possible, a partial resection may be performed to reduce tumor size and alleviate symptoms.
2. Radiation Therapy:
-
Adjuvant Radiotherapy: After surgery, radiation therapy is often employed to target any residual tumor cells. High-dose external beam radiation or stereotactic radiosurgery (SRS) can be used, especially for small, localized tumors.
-
Targeted Radiation: Modern proton therapy or SRS allows for high-precision treatment while minimizing damage to surrounding healthy tissues.
3. Chemotherapy:
-
Chemotherapy Regimens: The primary chemotherapeutic agents for PNETs include cisplatin, etoposide, and cyclophosphamide. These are used for high-grade tumors or when the tumor has spread.
-
Adjuvant Chemotherapy: In some cases, chemotherapy is given after surgery and radiation to prevent recurrence.
Prevention and Management of Pineoblastoma and Supratentorial PNETs
Prevention:
Currently, there are no known methods to prevent pineoblastomas or supratentorial PNETs due to their genetic and sporadic nature. However, minimizing radiation exposure and seeking early medical evaluation for symptoms is crucial.
Management:
-
Long-Term Follow-Up: Ongoing monitoring with MRI scans and neurological assessments to detect recurrence or metastasis is essential.
-
Symptom Management: Managing symptoms like pain, nausea, and hydrocephalus through medications and shunt placements.
-
Rehabilitation: After surgery or radiation, physical therapy, cognitive therapy, and speech therapy may be necessary to regain lost functions.
Complications of Pineoblastoma and Supratentorial PNETs
Surgical Complications:
-
Infection and hemorrhage are common
surgical risks.
-
Neurological deficits (e.g., vision
loss, speech deficits) can occur if the
tumor is near vital brain structures.
Radiation Complications:
-
Cognitive decline, neuroendocrine
dysfunction, and radiation necrosis can
occur as late effects.
Chemotherapy Side Effects:
-
Bone marrow suppression, immune system
weakening, and hair loss.
Infection and hemorrhage are common surgical risks.
Neurological deficits (e.g., vision loss, speech deficits) can occur if the tumor is near vital brain structures.
-
Cognitive decline, neuroendocrine dysfunction, and radiation necrosis can occur as late effects.
Chemotherapy Side Effects:
-
Bone marrow suppression, immune system
weakening, and hair loss.
Bone marrow suppression, immune system weakening, and hair loss.
Living with Pineoblastoma and Supratentorial PNETs
Patients diagnosed with pineoblastomas and supratentorial PNETs require a comprehensive rehabilitation plan and psychosocial support to navigate the challenges of living with these aggressive tumors.
Rehabilitation:
-
Physical therapy and neuropsychological
therapy may be required for patients who experience motor
or cognitive impairments after treatment.
Psychosocial Support:
-
Counseling and support groups for
patients and their families can help them cope with the emotional toll
of diagnosis and treatment.
Physical therapy and neuropsychological therapy may be required for patients who experience motor or cognitive impairments after treatment.
-
Counseling and support groups for patients and their families can help them cope with the emotional toll of diagnosis and treatment.
Top 10 Frequently Asked Questions about Pineoblastoma and Supratentorial Primitive Neuroectodermal Tumors (PNETs)
1. What are pineoblastoma and supratentorial primitive neuroectodermal tumors (PNETs)?
Pineoblastoma is a rare, aggressive brain tumor that originates in the pineal gland, which is located in the center of the brain. It belongs to a group of tumors known as primitive neuroectodermal tumors (PNETs), which are composed of primitive, undifferentiated cells that can develop into different types of brain tissue.
Supratentorial PNETs refer to tumors that develop in the upper part of the brain, above the tentorium (a structure that separates the cerebrum from the cerebellum). These tumors are most commonly found in children and young adults and are characterized by fast growth and a high likelihood of spreading to other areas of the brain and spinal cord.
2. What causes pineoblastoma and PNETs?
The exact cause of pineoblastoma and supratentorial PNETs is not well understood, but they are believed to arise from genetic mutations in cells in the brain. These mutations cause cells to grow uncontrollably and form a tumor. Certain genetic syndromes may increase the risk of developing these tumors, including:
-
Li-Fraumeni syndrome.
-
Turcot syndrome.
-
Neurofibromatosis type 1 (NF1).
-
Familial retinoblastoma (for pineoblastoma).
However, many cases occur sporadically, without any clear inherited genetic mutation.
3. What are the symptoms of pineoblastoma and PNETs?
Symptoms vary depending on the tumor's size, location, and how much pressure it puts on surrounding brain structures. Common symptoms include:
-
Headaches (especially in the morning or after sleeping).
-
Nausea and vomiting.
-
Vision problems (due to pressure on the optic nerves).
-
Seizures.
-
Cognitive changes (difficulty with concentration, memory, or reasoning).
-
Balance or coordination issues.
-
Abnormal eye movements or double vision.
-
Developmental delays or neurological deficits in children.
Since these symptoms overlap with other conditions, diagnosis typically requires imaging tests.
4. How is pineoblastoma or PNET diagnosed?
The diagnosis of pineoblastoma and PNETs involves several steps:
-
Neurological examination: To assess cognitive and motor function.
-
Imaging tests: Such as MRI or CT scans, which provide detailed images of the brain and help identify the location and size of the tumor.
-
Biopsy: A tissue sample may be taken through stereotactic biopsy or surgical removal to confirm the diagnosis and determine the tumor's type and grade.
-
Molecular and genetic testing: To understand the tumor's genetic makeup and guide treatment decisions.
5. What are the treatment options for pineoblastoma and PNETs?
The treatment for pineoblastoma and supratentorial PNETs typically involves a combination of:
-
Surgery: The first step is often to remove as much of the tumor as possible. However, due to the tumor's location, complete removal may not always be possible.
-
Radiation therapy: After surgery, radiation is often used to target any remaining tumor cells, especially in high-grade tumors or those that cannot be fully resected.
-
Chemotherapy: Often used in combination with surgery and radiation, particularly for high-risk tumors or when the tumor has spread.
-
Targeted therapy: In some cases, newer therapies targeting specific genetic mutations or cancer cell behaviors may be used, although this is still being researched.
Treatment is highly individualized and based on the tumor's location, size, and whether it has spread to other parts of the body.
6. What is the prognosis for pineoblastoma and PNETs?
The prognosis for patients with pineoblastoma and PNETs can vary based on factors such as:
-
Tumor grade: High-grade tumors (which are more aggressive) typically have a worse prognosis.
-
Surgical resection: The more tumor that can be safely removed, the better the chances of a favorable outcome.
-
Response to treatment: Patients who respond well to chemotherapy and radiation may have better outcomes.
-
Age and overall health: Children and younger adults often have better prognoses compared to older individuals.
Despite aggressive treatment, these tumors are often associated with a poor prognosis, especially if the tumor has spread. Survival rates vary depending on the extent of the disease and treatment efficacy.
7. Can pineoblastoma and PNETs recur after treatment?
Yes, both pineoblastoma and supratentorial PNETs have the potential to recur after treatment, especially if the tumor was not completely removed or if the disease was aggressive. Tumors that have spread to other areas, such as the spinal cord or brain, may also increase the risk of recurrence. Regular follow-up imaging, such as MRI scans, is essential for detecting recurrence early. If the tumor recurs, additional treatment options such as radiation, chemotherapy, or surgical re-intervention may be required.
8. Are there any side effects of the treatments for pineoblastoma and PNETs?
Treatment for pineoblastoma and PNETs can cause various side effects, depending on the type of therapy used:
-
Surgery: Risks include infection, bleeding, or damage to surrounding brain tissue, leading to neurological deficits.
-
Radiation therapy: Can cause fatigue, hair loss, skin irritation, and long-term effects like cognitive decline or developmental delays in children.
-
Chemotherapy: Common side effects include nausea, vomiting, fatigue, hair loss, and increased risk of infections due to suppressed immunity.
-
Endocrine issues: Treatment may affect the pineal gland's function, which can lead to problems with sleep cycles or hormonal imbalances.
These side effects are managed through supportive care and monitoring.
9. Can pineoblastoma and PNETs be prevented?
Currently, there is no known way to prevent pineoblastoma or PNETs, as the exact causes of these tumors are not fully understood. Genetic factors may play a role, and individuals with a family history of certain conditions (like Li-Fraumeni syndrome or neurofibromatosis) may be at higher risk. While prevention isn't possible, early detection through regular check-ups and genetic counseling can help in managing the risk and improving treatment outcomes if these tumors occur.
10. What support is available for patients with pineoblastoma and PNETs?
Support for patients with pineoblastoma and PNETs is crucial for both physical and emotional well-being:
-
Multidisciplinary care: A team of oncologists, neurosurgeons, radiologists, and psychologists work together to provide comprehensive care.
-
Support groups: Connecting with others who are going through similar experiences can help patients and families cope with the emotional aspects of cancer treatment.
-
Rehabilitation: After treatment, patients may need physical therapy, cognitive therapy, or speech therapy to recover from the effects of surgery or radiation.
-
Counseling: Emotional and psychological support is vital, particularly in dealing with the stress and trauma of a cancer diagnosis and treatment.


