Introduction to Plasma Cell Neoplasm / Multiple Myeloma
Multiple Myeloma (MM), also known as plasma cell neoplasm, is a type of hematologic cancer that originates from plasma cells—a subtype of white blood cells that are crucial for immune function. Plasma cells produce antibodies, which are responsible for fighting infections. In multiple myeloma, these plasma cells become cancerous and start growing uncontrollably in the bone marrow, leading to a variety of complications, including bone damage, kidney dysfunction, and immune suppression.
Epidemiology of Multiple Myeloma
-
Prevalence: Multiple myeloma represents 1% of all cancers and 10% of all blood cancers. It is a relatively rare condition but is considered the second most common hematologic malignancy, after non-Hodgkin lymphoma.
-
Incidence: The median age of diagnosis is around 69 years. The disease most commonly affects individuals over the age of 65, though it can occur in younger adults, particularly those with genetic predispositions.
-
Gender and Race: Men are more likely to develop MM than women. The disease is more common in African American populations than in Caucasian or other racial groups. Studies suggest that African Americans have a twofold higher risk compared to Caucasians.
Prognosis:
Despite advances in chemotherapy, stem cell transplantation, and immunotherapy, multiple myeloma remains largely incurable. However, with new therapies, the median survival rate has improved significantly, with 10-15% of patients achieving long-term remission.
Causes and Risk Factors of Plasma Cell Neoplasm / Multiple Myeloma
The exact cause of multiple myeloma is unknown, but several genetic and environmental factors are thought to contribute to its development. These factors may lead to DNA damage in plasma cells, causing them to become malignant.
Genetic Risk Factors
-
Monoclonal Gammopathy of Undetermined Significance (MGUS):
-
MGUS is a precursor condition that occurs when abnormal protein levels are found in the blood without obvious symptoms. It is often the first stage in plasma cell dyscrasia and is diagnosed in 3-4% of people aged 50 or older. 1% of MGUS patients develop MM each year.
-
-
Inherited Genetic Mutations:
-
Several genetic mutations have been implicated in the development of multiple myeloma, including TP53, RB1, and MYC mutations. These mutations disrupt the cell cycle and immune checkpoints, leading to uncontrolled cell division.
-
-
Familial Multiple Myeloma:
-
Although most cases of MM are sporadic, familial cases have been observed, suggesting a genetic component. Families with a history of MM may be at increased risk, particularly those with first-degree relatives affected by the disease.
-
Environmental and Lifestyle Risk Factors
-
Radiation Exposure:
-
Ionizing radiation is a known risk factor for multiple myeloma. Survivors of childhood cancers who underwent radiation therapy have a higher incidence of developing MM in later years.
-
-
Chemical Exposures:
-
Occupational exposure to pesticides, herbicides, petroleum products, and industrial chemicals has been associated with an elevated risk of MM.
-
-
Obesity:
-
Obesity, particularly excess body fat, is a modifiable risk factor for multiple myeloma. Studies show that individuals with a higher BMI are more likely to develop the disease, especially in postmenopausal women.
-
-
Chronic Viral Infections:
-
Certain chronic viral infections, like HIV or hepatitis C, may increase the risk of developing plasma cell neoplasms, although these associations are still under investigation.
-
Symptoms and Signs of Plasma Cell Neoplasm / Multiple Myeloma
The clinical presentation of multiple myeloma varies greatly, depending on the extent of disease and the organs involved. Some patients may have no symptoms at first, while others present with severe and debilitating conditions.
Key Symptoms of Multiple Myeloma:
-
Bone Pain:
-
Bone pain is often the most noticeable symptom
and can occur in the back,
ribs, hips, or
skull. The pain is caused by bone
destruction as myeloma cells invade the bone marrow
and disrupt normal bone metabolism. Bone pain may be
constant or worsen with activity.
-
Fatigue:
-
Anemia caused by the replacement of normal
plasma cells with myeloma cells leads to fatigue, weakness, and
shortness of breath.
-
Recurrent Infections:
-
Myeloma impairs the immune system, leading to an
increased susceptibility to infections. Patients may experience
frequent respiratory infections,
urinary tract infections, or skin
infections.
-
Hypercalcemia:
-
Elevated calcium levels due to bone breakdown
can lead to symptoms such as nausea,
vomiting, constipation, and
confusion.
-
Kidney Dysfunction:
-
The accumulation of light chains in the kidneys
can lead to renal damage, which is one of the
leading causes of kidney failure in multiple
myeloma patients. Symptoms of kidney dysfunction include
swelling, fatigue, and
changes in urination.
-
Neurological Symptoms:
-
If the tumor invades the spinal cord, patients
may experience numbness,
weakness, or paralysis. This
is due to spinal cord compression from
vertebral lesions.
-
Weight Loss:
-
Unexplained weight loss is common in advanced
stages of the disease and may be due to the increased
metabolic activity of the cancer cells.
Bone Pain:
-
Bone pain is often the most noticeable symptom and can occur in the back, ribs, hips, or skull. The pain is caused by bone destruction as myeloma cells invade the bone marrow and disrupt normal bone metabolism. Bone pain may be constant or worsen with activity.
Fatigue:
-
Anemia caused by the replacement of normal plasma cells with myeloma cells leads to fatigue, weakness, and shortness of breath.
Recurrent Infections:
-
Myeloma impairs the immune system, leading to an increased susceptibility to infections. Patients may experience frequent respiratory infections, urinary tract infections, or skin infections.
Hypercalcemia:
-
Elevated calcium levels due to bone breakdown can lead to symptoms such as nausea, vomiting, constipation, and confusion.
Kidney Dysfunction:
-
The accumulation of light chains in the kidneys can lead to renal damage, which is one of the leading causes of kidney failure in multiple myeloma patients. Symptoms of kidney dysfunction include swelling, fatigue, and changes in urination.
Neurological Symptoms:
-
If the tumor invades the spinal cord, patients may experience numbness, weakness, or paralysis. This is due to spinal cord compression from vertebral lesions.
Weight Loss:
-
Unexplained weight loss is common in advanced stages of the disease and may be due to the increased metabolic activity of the cancer cells.
Diagnosis of Plasma Cell Neoplasm / Multiple Myeloma
Diagnosing multiple myeloma requires a combination of clinical symptoms, laboratory tests, and imaging studies.
1. Laboratory Tests
-
Serum Protein Electrophoresis (SPEP): Detects monoclonal proteins (M-proteins) in the blood, which are a hallmark of myeloma.
-
Complete Blood Count (CBC): Often reveals anemia, low white blood cell count, and thrombocytopenia.
-
Bence-Jones Protein Test: Detects abnormal light chain proteins in urine, characteristic of multiple myeloma.
-
Free Light Chain Assay: This measures kappa and lambda light chains in the blood and is a diagnostic tool for multiple myeloma.
-
Bone Marrow Biopsy: To assess the percentage of plasma cells in the marrow. More than 10% plasma cells in the bone marrow is indicative of myeloma.
-
Beta-2 Microglobulin: This is often used as a prognostic indicator for myeloma.
-
Cytogenetic Testing: Helps identify genetic mutations or chromosomal abnormalities associated with myeloma.
2. Imaging Studies
-
X-rays: X-rays can detect bone lesions, osteolytic areas, and osteoporosis typical in MM.
-
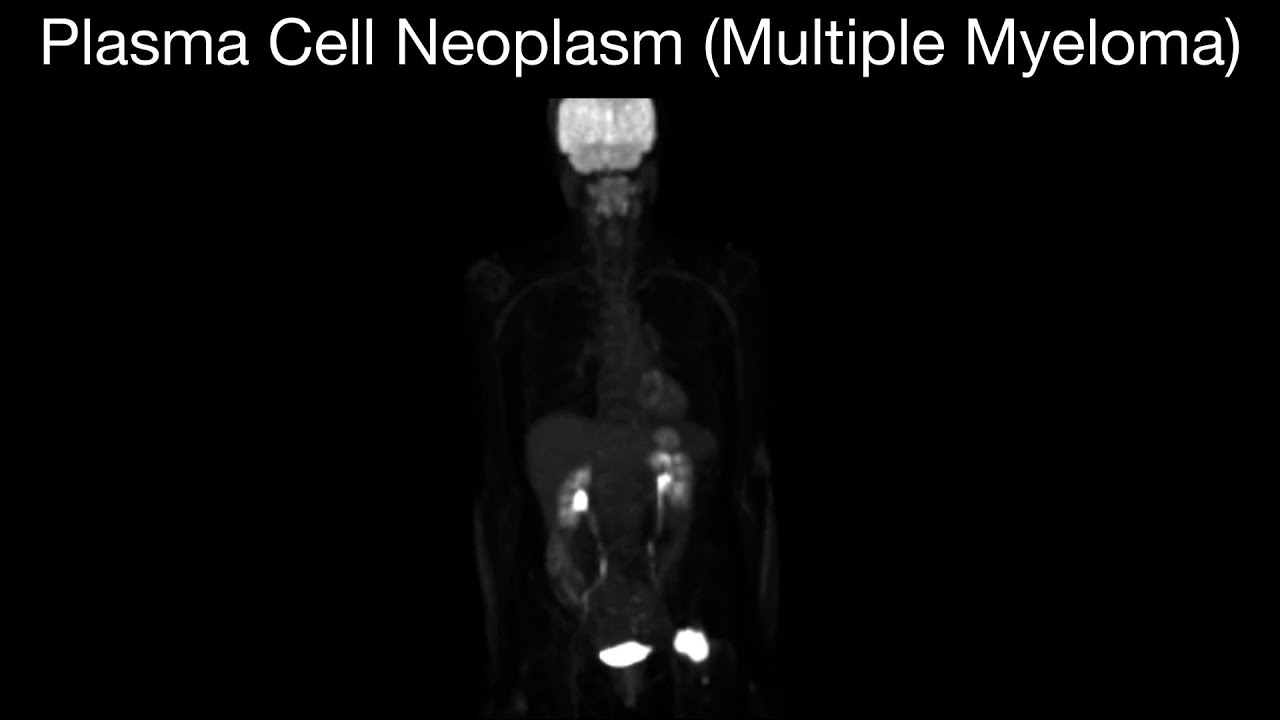
MRI/CT Scans: Useful for identifying spinal cord compression or soft tissue involvement. MRI can also identify areas of bone marrow infiltration.
-
PET Scans: Can assess the metabolic activity of the tumor and detect extramedullary disease (disease outside of the bone marrow).
Treatment Options for Plasma Cell Neoplasm / Multiple Myeloma
Multiple myeloma treatment is tailored to the individual's health, tumor characteristics, and stage of disease. The main treatment modalities include chemotherapy, stem cell transplantation, and targeted therapies.
1. Chemotherapy
Chemotherapy is often the first line of treatment for multiple myeloma. Common drugs include:
-
Melphalan
-
Cyclophosphamide
-
Vincristine
2. Stem Cell Transplantation
-
Autologous Stem Cell Transplant: Involves harvesting the patient’s own stem cells, administering high-dose chemotherapy to kill cancer cells, and reinfusing the stem cells to regenerate the bone marrow.
-
Allogeneic Stem Cell Transplant: A transplant from a healthy donor to replace the patient's diseased bone marrow. This is less commonly used but may offer advantages for high-risk patients.
3. Targeted Therapy
Targeted therapies aim to interfere with specific processes within the cancer cells. These include:
-
Proteasome Inhibitors (e.g., Bortezomib): These drugs prevent the breakdown of proteins within cancer cells, causing them to accumulate and die.
-
Immunomodulatory Drugs (e.g., Lenalidomide): These enhance the immune system’s ability to detect and kill cancer cells.
4. Radiation Therapy
-
Radiotherapy is used to treat localized bone lesions and manage spinal cord compression or bone pain.
5. Immunotherapy
-
Monoclonal Antibodies (e.g., Daratumumab) are used to target specific proteins on myeloma cells and activate the immune system to destroy the cancer.
Prevention and Management of Plasma Cell Neoplasm / Multiple Myeloma
Currently, prevention strategies for multiple myeloma are limited due to its largely genetic and unknown causes. However, for individuals at risk, early detection can significantly improve outcomes.
Management of Multiple Myeloma
-
Regular Follow-Up: Patients require regular monitoring through blood tests, MRI, and bone marrow assessments.
-
Symptom Management: Medications for pain, anemia, and infections.
-
Supportive Care: Bisphosphonates to strengthen bones and erythropoiesis-stimulating agents for anemia.
Complications of Plasma Cell Neoplasm / Multiple Myeloma
1. Bone Fractures
Multiple myeloma causes bone loss and increases the risk of fractures, particularly in weight-bearing bones.
2. Kidney Failure
-
Due to the accumulation of Bence-Jones proteins and other abnormal proteins, multiple myeloma often leads to kidney damage or renal failure.
3. Immune System Suppression
-
Increased susceptibility to infections due to the loss of normal immune cell production.
Living with Plasma Cell Neoplasm / Multiple Myeloma
Living with multiple myeloma requires continuous care, regular follow-ups, and a multidisciplinary approach:
1. Emotional and Psychological Support
-
Patients often experience depression, anxiety, and stress due to the chronic nature of the disease. Counseling and support groups can be very helpful.
2. Lifestyle Changes
-
Dietary support, regular exercise, and maintaining bone health can greatly improve quality of life.
Top 10 Frequently Asked Questions about Plasma Cell Neoplasm / Multiple Myeloma
1. What is multiple myeloma?
Multiple myeloma is a rare and incurable blood cancer that originates in plasma cells, a type of white blood cell found in the bone marrow. These malignant plasma cells multiply uncontrollably, producing abnormal proteins that can damage bones, kidneys, and the immune system. The term "multiple" refers to the frequent occurrence of multiple areas of bone involvement.
2. What are the common symptoms of multiple myeloma?
Symptoms can vary widely and may include:
-
Persistent bone pain, especially in the back, ribs, or hips
-
Fatigue or weakness
-
Frequent infections
-
Unexplained weight loss
-
Nausea or constipation
-
Kidney problems
-
Numbness or tingling in the legs
-
Easy bruising or bleeding
These symptoms often overlap with other conditions, making early diagnosis challenging.
3. How is multiple myeloma diagnosed?
Diagnosis typically involves:
-
Blood tests: To detect abnormal proteins (monoclonal proteins or M proteins) and assess kidney function.
-
Urine tests: To identify Bence Jones proteins.
-
Bone marrow biopsy: To examine the percentage of plasma cells and detect abnormalities.
-
Imaging tests: Such as X-rays, MRI, or PET scans to identify bone lesions or fractures.
The International Myeloma Working Group (IMWG) criteria are used to confirm the diagnosis.
4. What are the stages of multiple myeloma?
Multiple myeloma is staged using the Revised International Staging System (R-ISS), which considers:
-
Serum β2-microglobulin levels
-
Serum albumin levels
-
LDH levels
-
Cytogenetic abnormalities
Based on these factors, the disease is classified into three stages:
-
Stage I: Least aggressive
-
Stage II: Intermediate
-
Stage III: Most aggressive
This staging helps predict prognosis and guide treatment decisions.
5. What are the treatment options for multiple myeloma?
Treatment strategies include:
-
Chemotherapy: To kill rapidly dividing myeloma cells.
-
Immunomodulatory drugs: Such as lenalidomide to enhance the immune system's ability to fight cancer.
-
Proteasome inhibitors: Like bortezomib to disrupt the degradation of proteins within myeloma cells.
-
Monoclonal antibodies: Such as daratumumab to target specific proteins on myeloma cells.
-
Stem cell transplant: To replace damaged bone marrow with healthy cells.
-
Radiation therapy: To target and shrink tumors.
-
Bisphosphonates: To strengthen bones and prevent fractures.
Treatment plans are personalized based on the patient's health status and disease characteristics.
6. Is multiple myeloma curable?
Currently, multiple myeloma is considered incurable. However, with advancements in treatment, many patients can achieve periods of remission and manage the disease effectively, leading to improved quality of life and extended survival.
7. What are the risk factors for developing multiple myeloma?
Risk factors include:
-
Age: Most common in individuals over 65.
-
Gender: Men are at higher risk.
-
Race: More prevalent in African Americans.
-
Family history: Having a close relative with the disease increases risk.
-
Pre-existing conditions: Monoclonal gammopathy of undetermined significance (MGUS) or plasmacytoma.
-
Environmental exposures: Exposure to certain chemicals or radiation.
While these factors increase risk, many individuals with multiple myeloma have no known risk factors.
8. Can multiple myeloma be prevented?
There are no known strategies to prevent multiple myeloma. However, regular medical check-ups and monitoring conditions like MGUS can help detect the disease early, potentially improving outcomes.
9. What is the prognosis for someone with multiple myeloma?
Prognosis varies based on factors such as disease stage, response to treatment, and overall health. The five-year survival rate is approximately 54%. Advancements in treatment have significantly improved outcomes, with many patients living longer and maintaining a good quality of life.
10. What support is available for patients with multiple myeloma?
Support options include:
-
Medical teams: Oncologists, hematologists, and specialized nurses.
-
Support groups: Connecting with others facing similar challenges.
-
Counseling services: Emotional and psychological support.
-
Financial assistance: Resources to help with treatment costs.
-
Educational resources: Information on disease management and coping strategies.
It's important for patients to discuss available support services with their healthcare providers.


