Introduction to Pre-Implantation Genetic Diagnosis
Pre-Implantation Genetic Diagnosis (PGD) is an advanced reproductive technology that allows for the genetic screening of embryos before implantation during an in vitro fertilization (IVF) cycle. PGD enables the identification of specific genetic conditions, chromosomal abnormalities, and inherited disorders, thereby assisting in the selection of healthy embryos for transfer into the uterus.
Historical Context
PGD was first successfully used in humans in the late 1980s and early 1990s. The initial applications focused on detecting sex-linked genetic disorders, such as Duchenne muscular dystrophy and hemophilia. Over time, advancements in molecular genetics and reproductive medicine have expanded the scope of PGD to include a wide range of genetic conditions.
Indications for PGD
PGD is primarily indicated for couples who are at risk of transmitting specific genetic disorders to their offspring. Common indications include:
-
Carrier status of autosomal recessive or X-linked disorders: Couples both carrying a mutation for a recessive disorder, such as cystic fibrosis or sickle cell anemia.
-
Presence of structural chromosomal abnormalities: Individuals with balanced translocations or inversions that may lead to unbalanced gametes.
-
Advanced maternal age: Women over the age of 35, who have a higher risk of chromosomal abnormalities in embryos.
-
Recurrent pregnancy loss or implantation failure: Couples experiencing multiple miscarriages or failed IVF cycles.
Causes and Risks of Pre-Implantation Genetic Diagnosis
Pre-Implantation Genetic Diagnosis (PGD) is a specialized reproductive technology used alongside in vitro fertilization (IVF) to identify genetic or chromosomal abnormalities in embryos before implantation. While PGD offers significant benefits for couples at risk of passing on genetic disorders, it is associated with specific causes for its use and potential risks that should be carefully considered.
Causes of Genetic Disorders Detected by PGD
PGD can identify various genetic abnormalities, including:
-
Single-gene mutations: Responsible for monogenic disorders such as Huntington's disease, thalassemia, and Tay-Sachs disease.
-
Chromosomal abnormalities: Including aneuploidies (e.g., Down syndrome) and structural rearrangements (e.g., translocations).
-
Mitochondrial DNA mutations: Inherited maternally and associated with disorders like Leber's hereditary optic neuropathy.
Risks Associated with PGD
While PGD offers significant benefits, it is not without risks:
-
Embryo biopsy complications: The process of removing a cell from the embryo can potentially damage it, leading to reduced viability or failure to implant.
-
False positives/negatives: Errors in genetic testing can result in the misidentification of healthy embryos as affected or vice versa.
-
Ethical concerns: Issues related to the selection of embryos based on non-medical traits, such as sex selection for non-medical reasons, raise ethical debates.
-
Psychological impact: The decision-making process and outcomes of PGD can have emotional and psychological effects on individuals and couples.
Symptoms and Signs of Pre-Implantation Genetic Diagnosis
Pre-Implantation Genetic Diagnosis (PGD) itself is not a disease, so it doesn't have symptoms in the conventional sense. However, individuals or couples who consider PGD usually do so due to underlying genetic conditions, fertility issues, or recurrent pregnancy complications. Therefore, the “signs and symptoms” related to PGD are primarily linked to the conditions or circumstances that lead someone to seek it.
1. Indications Leading to PGD
PGD is typically recommended when there's a risk of passing on genetic disorders or reproductive challenges. Some indicators include:
-
Family history of genetic disorders
Couples may seek PGD if they or close relatives carry mutations causing diseases like cystic fibrosis, thalassemia, Huntington's disease, or muscular dystrophy. -
Recurrent miscarriages
Often caused by chromosomal abnormalities in embryos. -
Previous child with a genetic condition
Parents may want to prevent recurrence in future pregnancies. -
Advanced maternal age
Increases the risk of chromosomal abnormalities such as Down syndrome. -
Failed IVF attempts
PGD helps identify genetically healthy embryos, improving success rates.
2. Emotional and Psychological Signs
Couples seeking PGD often experience:
-
Anxiety over having a child with a genetic condition.
-
Emotional stress from infertility struggles or recurrent pregnancy losses.
-
Desire for reassurance before embryo implantation.
3. Physical Signs Related to Underlying Conditions
While PGD itself has no physical symptoms, individuals may exhibit signs linked to hereditary or fertility-related issues, such as:
-
Irregular menstrual cycles
Linked to hormonal or ovarian problems. -
Signs of genetic disorders in one partner
For example, muscular weakness, organ dysfunction, or metabolic disorders. -
Infertility-related symptoms
Such as abnormal sperm counts, ovulatory issues, or polycystic ovarian syndrome (PCOS).
4. Signs Indicating the Need for PGD
-
Multiple failed pregnancies despite healthy lifestyle.
-
A known carrier status for autosomal recessive or X-linked conditions.
-
Family history of diseases passed through specific genes.
-
Difficulty conceiving without assisted reproductive technologies like IVF.
Diagnosis of Pre-Implantation Genetic Diagnosis
Pre-Implantation Genetic Diagnosis (PGD) is a sophisticated laboratory technique used during in vitro fertilization (IVF) to identify genetic abnormalities in embryos before they are implanted in the uterus. The goal of PGD diagnosis is to help prevent the transmission of specific genetic disorders or chromosomal abnormalities to the offspring.
1. Pre-Diagnosis Screening and Assessment
Before proceeding with PGD, doctors perform several evaluations to ensure eligibility and appropriateness:
-
Medical History Review - Assessment of parental genetic background and family history.
-
Genetic Counseling - Couples are informed about possible risks, success rates, and limitations.
-
Blood Tests & Carrier Screening - Identifies if one or both partners are carriers of genetic disorders.
-
Hormonal Evaluations - Ensures reproductive health and readiness for IVF.
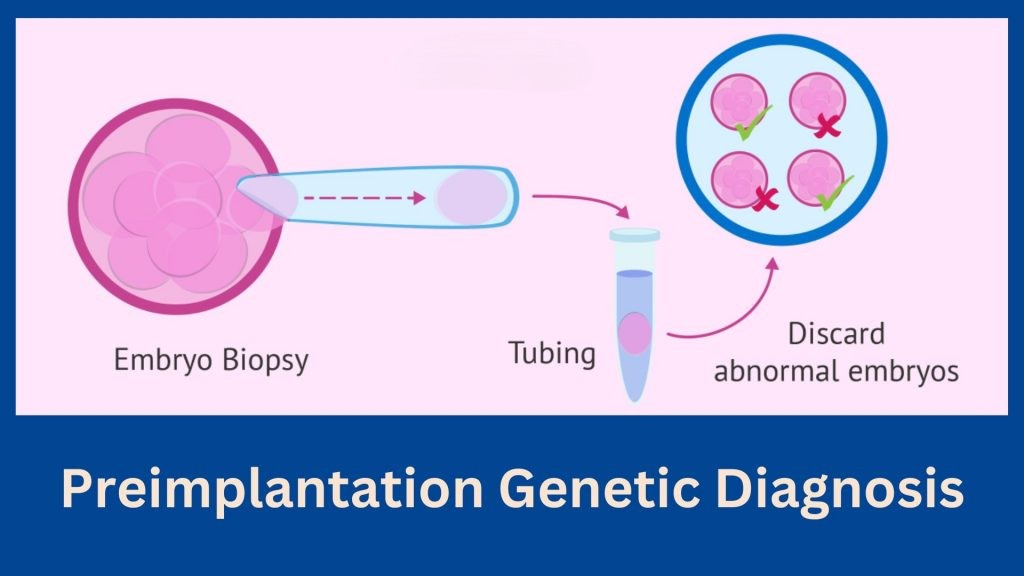
2. Embryo Biopsy Procedure
Once the couple undergoes IVF and embryos are formed, an embryo biopsy is performed:
-
Typically done on Day 3 (cleavage-stage embryos) or Day 5/6 (blastocyst-stage embryos).
-
A few cells are carefully removed from the embryo without harming its viability.
-
These cells are then subjected to advanced genetic testing techniques.
3. Genetic Testing Techniques Used in PGD
The diagnostic phase involves one or more of the following methods:
a. Polymerase Chain Reaction (PCR)
-
Detects single-gene disorders such as cystic fibrosis, sickle cell anemia, or Huntington's disease.
-
Rapid and highly specific.
b. Fluorescence In Situ Hybridization (FISH)
-
Identifies chromosomal abnormalities like translocations or aneuploidy.
-
Frequently used for sex-linked disorders.
c. Next-Generation Sequencing (NGS)
-
Offers a comprehensive and highly accurate diagnosis.
-
Can detect single-gene mutations, chromosomal imbalances, and mosaicism simultaneously.
d. Comparative Genomic Hybridization (CGH)
-
Assesses structural and numerical chromosomal abnormalities.
-
Enhances embryo selection for better IVF outcomes.
4. Interpretation of Results
-
Embryos are classified as:
-
Genetically Normal (Euploid) - Recommended for implantation.
-
Genetically Abnormal (Aneuploid or Mutated) - Excluded from transfer.
-
Mosaic - May require deeper counseling before selection.
-
5. Post-Diagnosis Counseling
After PGD results are obtained:
-
Genetic counselors discuss findings with the couple.
-
Options are explained, including transferring healthy embryos, freezing embryos, or considering donor gametes.
-
Emotional and psychological support is provided during decision-making.
6. Importance of PGD Diagnosis
-
Prevents the transmission of hereditary genetic disorders.
-
Increases chances of a healthy pregnancy.
-
Reduces risks of recurrent miscarriages caused by chromosomal abnormalities.
-
Helps couples with a history of failed IVF attempts make informed choices.
Treatment Options for Pre-Implantation Genetic Diagnosis
Pre-Implantation Genetic Diagnosis (PGD) is a specialized reproductive technology used alongside In Vitro Fertilization (IVF) to identify genetic abnormalities in embryos before implantation. The main objective of PGD is to ensure that only healthy embryos are transferred into the uterus, minimizing the risk of passing on genetic disorders. Treatment options associated with PGD involve a combination of medical, genetic, and reproductive techniques.
1. In Vitro Fertilization (IVF) with PGD
PGD is always performed in conjunction with IVF. The process involves:
-
Ovarian Stimulation: Hormonal medications are administered to stimulate the ovaries to produce multiple eggs.
-
Egg Retrieval: Mature eggs are collected using a minimally invasive procedure.
-
Fertilization: Eggs are fertilized with sperm in the laboratory to create embryos.
-
Embryo Biopsy: A few cells are carefully removed from the embryo for genetic analysis.
-
Embryo Testing: The cells are screened for specific genetic or chromosomal abnormalities before implantation.
This is the primary treatment option when there's a known risk of inherited genetic conditions.
2. Targeted PGD for Single-Gene Disorders
For couples at risk of transmitting specific inherited diseases, PGD can target:
-
Autosomal Recessive Disorders (e.g., cystic fibrosis, thalassemia)
-
Autosomal Dominant Disorders (e.g., Huntington's disease, Marfan syndrome)
-
X-linked Disorders (e.g., Duchenne muscular dystrophy, hemophilia)
This approach involves customized genetic probes that analyze embryos for the presence of defective genes. Only embryos without the disorder are selected for transfer.
3. Chromosomal PGD / PGT-A (Preimplantation Genetic Testing for Aneuploidies)
For couples with a history of recurrent miscarriages, failed IVF cycles, or advanced maternal age, PGD can test embryos for:
-
Missing or extra chromosomes (aneuploidies)
-
Structural chromosomal abnormalities
This improves the chances of a healthy pregnancy and reduces the likelihood of implantation failure.
4. PGD for HLA Matching (Savior Sibling)
In some cases, PGD is used to create an embryo that is a genetic match for an existing child suffering from conditions like thalassemia or leukemia.
-
Healthy embryos that are also HLA-compatible are selected.
-
Stem cells from the newborn's umbilical cord can be used for life-saving transplants for the affected sibling.
5. Combined Use of PGT-M, PGT-A, and PGT-SR
In complex cases, multiple forms of preimplantation testing can be used together:
-
PGT-M: For monogenic disorders.
-
PGT-A: For chromosomal abnormalities.
-
PGT-SR: For structural rearrangements like translocations.
This integrated approach offers maximum precision in selecting the healthiest embryos.
6. Counseling and Supportive Treatments
PGD is not just a medical process — it also involves:
-
Genetic Counseling: Educating couples about risks, procedures, and potential outcomes.
-
Psychological Support: Helping individuals and couples cope with emotional and ethical concerns.
-
Lifestyle Modifications: Optimizing health before and during treatment for better IVF success.
7. Alternative Reproductive Options
For couples where PGD is not feasible or unsuccessful, alternatives include:
-
Using Donor Eggs or Sperm to eliminate genetic risks.
-
Adoption as an alternative pathway to parenthood.
-
Prenatal Diagnosis followed by selective pregnancy management.
Prevention and Management of Pre-Implantation Genetic Diagnosis
Pre-Implantation Genetic Diagnosis (PGD) is an advanced reproductive technology used to screen embryos for specific genetic disorders before implantation during an in-vitro fertilization (IVF) cycle. While PGD helps prevent the transmission of inherited conditions, its successful outcomes depend on proper prevention strategies and effective management during and after the process.
Prevention
While PGD cannot prevent genetic disorders, it can prevent the transmission of specific inherited conditions by selecting unaffected embryos. Couples considering PGD should undergo genetic counseling to understand the risks and benefits and to determine the most appropriate course of action.
Management
The management of PGD involves:
-
Genetic Counseling: Providing information and support to individuals and couples regarding genetic risks and reproductive options.
-
IVF Coordination: Collaborating with fertility specialists to plan and execute the IVF and PGD procedures.
-
Emotional Support: Addressing the psychological aspects of PGD, including the emotional impact of the decision-making process and the outcomes.
Complications of Pre-Implantation Genetic Diagnosis
Potential complications associated with PGD include:
-
Embryo Damage: The biopsy procedure may harm the embryo, leading to its failure to develop or implant.
-
Misdiagnosis: Errors in genetic testing can result in the selection of affected embryos or the discarding of healthy ones.
-
Emotional Stress: The process can be emotionally taxing, particularly if the results are unfavorable or if no healthy embryos are available for transfer.
Living with the Condition of Pre-Implantation Genetic Diagnosis
Individuals and couples undergoing PGD should be prepared for the emotional and psychological aspects of the process:
-
Emotional Support: Access to counseling services can help individuals cope with the stress and emotions associated with PGD.
-
Informed Decision-Making: Understanding the implications of PGD results and the available options is crucial for making informed decisions.
-
Ongoing Monitoring: After embryo transfer, monitoring for pregnancy and fetal development is essential to ensure a healthy outcome.
Top 10 Frequently Asked Questions about Pre-Implantation Genetic Diagnosis
1. What is Pre-Implantation Genetic Diagnosis (PGD)?
Pre-Implantation Genetic Diagnosis (PGD) is a specialized procedure used in assisted reproductive technology (ART) to test embryos for specific genetic or chromosomal disorders before implantation during in vitro fertilization (IVF). This allows parents at risk of passing on inherited diseases to have a healthier child.
2. Why is PGD recommended?
PGD is recommended for:
-
Couples with a family history of genetic disorders.
-
Individuals carrying chromosomal abnormalities.
-
Couples with recurrent miscarriages.
-
Couples undergoing IVF who want to screen embryos for specific diseases.
It helps reduce the risk of genetic disorders in the child and improves the chances of a successful pregnancy.
3. How is PGD performed?
PGD involves several steps:
-
IVF procedure: Eggs are fertilized with sperm in the laboratory.
-
Embryo biopsy: A few cells are carefully removed from each embryo at the blastocyst stage (day 5-6).
-
Genetic testing: The biopsied cells are analyzed for specific genetic or chromosomal abnormalities.
-
Embryo selection: Only embryos without the targeted abnormalities are selected for uterine implantation.
4. What genetic disorders can PGD detect?
PGD can detect:
-
Single-gene disorders (e.g., cystic fibrosis, sickle cell anemia, Tay-Sachs disease).
-
Chromosomal abnormalities (e.g., Down syndrome, Turner syndrome).
-
Sex-linked disorders (e.g., hemophilia).
-
Inherited cancer syndromes in some cases.
The exact disorders screened depend on the couple's genetic background and medical history.
5. Is PGD safe for the embryo?
PGD is generally considered safe. The biopsy removes only a small number of cells, which typically does not harm the embryo's development. Advanced laboratory techniques and experienced embryologists further reduce the risk of damage. Most embryos continue to develop normally after PGD.
6. What are the success rates of PGD?
The success of PGD depends on multiple factors:
-
Quality of the embryos.
-
Age of the mother.
-
Type of genetic disorder being tested.
On average, PGD combined with IVF has a pregnancy success rate of 30-50% per cycle, similar to standard IVF, but it significantly reduces the risk of transferring an affected embryo.
7. Are there any risks associated with PGD?
Potential risks include:
-
Slight risk of embryo damage during biopsy (rare).
-
Misdiagnosis if genetic testing is not accurate.
-
Emotional and financial stress due to the cost and complexity of IVF with PGD.
-
Small risk of pregnancy loss, which is also present in regular IVF cycles.
Couples are advised to consult genetic counselors for proper guidance.
8. How should couples prepare for PGD?
Preparation includes:
-
Undergoing genetic counseling to identify risks and target genes.
-
Medical evaluation and fertility testing.
-
Discussing IVF protocols, medications, and cycle timing with the fertility specialist.
-
Ensuring emotional and financial readiness, as PGD involves time, costs, and repeated cycles in some cases.
9. How long does PGD take?
The process generally follows the IVF timeline:
-
Ovarian stimulation and egg retrieval: 2-3 weeks.
-
Fertilization and embryo culture: 3-6 days.
-
Genetic testing: 1-2 weeks.
-
Embryo transfer: Usually the same cycle or following a frozen embryo transfer cycle.
The complete process from start to embryo transfer can take approximately 4-6 weeks per cycle.
10. Can PGD guarantee a healthy baby?
While PGD significantly reduces the risk of known genetic disorders, it cannot guarantee a completely healthy baby. It screens for specific genetic conditions chosen by the couple and may not detect all possible genetic or developmental issues. Regular prenatal care and screenings are still recommended during pregnancy.


