Introduction to Prostate Biopsy
A prostate biopsy is a medical procedure in which small tissue samples are removed from the prostate gland for examination under a microscope. It is primarily used to detect prostate cancer or other prostate-related conditions. The prostate gland is a small, walnut-shaped gland located below the bladder in men, responsible for producing seminal fluid that nourishes and transports sperm.
Prostate biopsy is usually recommended when a man has:
-
Elevated prostate-specific antigen (PSA) levels.
-
Abnormal findings during a digital rectal examination (DRE).
-
Previous imaging results suggesting potential abnormalities in the prostate.
Purpose of Prostate Biopsy
-
Confirming Cancer Diagnosis: Detects the presence, type, and aggressiveness of prostate cancer.
-
Guiding Treatment: Determines the most appropriate therapeutic approach.
-
Monitoring Disease: Helps in evaluating progression in men under active surveillance.
Prostate biopsies can be performed using different approaches, including transrectal, transperineal, and image-guided techniques, each with its own benefits and considerations. Advances in MRI-targeted biopsies have significantly improved the accuracy of detecting clinically significant prostate cancer.
Causes and Risk of Prostate Biopsy
A prostate biopsy is not performed for a disease itself but is indicated based on risk factors or diagnostic markers.
Common Indications for Prostate Biopsy
-
Elevated PSA Levels
PSA is a protein produced by the prostate. Elevated levels may indicate prostate cancer, inflammation (prostatitis), or benign enlargement (BPH). -
Abnormal Digital Rectal Examination (DRE)
Hard or irregular areas on the prostate may signal the need for a biopsy. -
Suspicious Imaging Findings
MRI or ultrasound may detect lesions or abnormalities requiring histological confirmation. -
Family History of Prostate Cancer
Men with first-degree relatives affected by prostate cancer have a higher risk and may need early screening.
Risk Factors for Prostate Cancer (Prompting Biopsy)
-
Age over 50 years.
-
African ancestry or certain ethnic backgrounds.
-
Genetic mutations (e.g., BRCA1, BRCA2).
-
Diet high in red meat or low in fruits/vegetables.
While prostate biopsy is generally safe, there are inherent risks associated with the procedure:
-
Infection or sepsis.
-
Bleeding from the rectum or urinary tract.
-
Urinary retention.
-
Discomfort or pain during and after the procedure.
Symptoms and Signs Indicating the Need for Prostate Biopsy
Most men do not have specific symptoms of prostate cancer, which is why screening is crucial. The need for a biopsy arises from screening results rather than clinical symptoms, but certain warning signs may prompt evaluation:
-
Difficulty or pain during urination.
-
Increased frequency of urination, especially at night (nocturia).
-
Blood in urine or semen.
-
Erectile dysfunction or pelvic discomfort.
-
Abnormal PSA levels or changes over time.
It is important to note that these symptoms can be caused by benign conditions as well, such as BPH or prostatitis. Only a biopsy can confirm the presence of malignant cells.
Diagnosis of Prostate Biopsy
Pre-Biopsy Evaluation
Before the procedure, a urologist will assess:
-
PSA levels over time.
-
Previous imaging, such as multiparametric MRI (mpMRI).
-
Overall health status, including bleeding disorders or medications like blood thinners.
Types of Prostate Biopsy
-
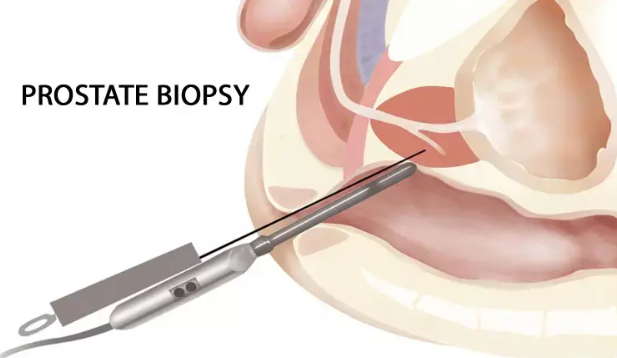
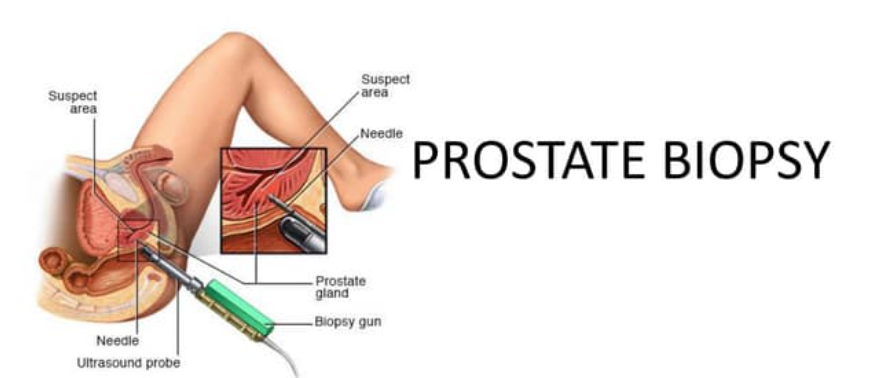
Transrectal Ultrasound-Guided Biopsy (TRUS)
-
The most common method.
-
A thin needle is inserted through the rectum to collect tissue samples.
-
-
Transperineal Biopsy
-
Needle inserted through the skin between the scrotum and anus (perineum).
-
Reduced risk of infection compared to TRUS.
-
-
MRI-Targeted Biopsy
-
Combines MRI imaging with ultrasound guidance to target suspicious areas.
-
Improves accuracy and reduces unnecessary sampling.
-
Procedure
-
Typically performed under local anesthesia; sometimes sedation may be used.
-
Multiple tissue cores (usually 10-12) are collected.
-
Samples are sent for histopathological analysis to detect cancer cells and evaluate Gleason score, which grades tumor aggressiveness.
Treatment Options Related to Prostate Biopsy
While a biopsy itself is a diagnostic procedure, the results guide subsequent treatment options:
If Cancer is Detected
-
Active Surveillance: Monitoring PSA levels and repeat biopsies for low-risk cancers.
-
Surgery (Radical Prostatectomy): Removal of the entire prostate in selected cases.
-
Radiation Therapy: External beam or brachytherapy depending on tumor stage.
-
Hormone Therapy: For advanced or aggressive cancer.
-
Chemotherapy or Targeted Therapy: In metastatic cases.
If Benign
-
No cancer detected; follow-up may include regular PSA monitoring and imaging.
-
Address underlying conditions like BPH or prostatitis if symptomatic.
Prevention and Management of Prostate Biopsy-Related Issues
Although a biopsy is necessary for diagnosis, steps can be taken to minimize complications:
Preventive Measures
-
Antibiotic Prophylaxis: Reduces risk of infection, especially in TRUS biopsies.
-
Bowel Preparation: Cleansing enema may reduce infection risk.
-
Review of Medications: Adjust blood thinners or anticoagulants before procedure.
Management Post-Biopsy
-
Pain Relief: Over-the-counter analgesics such as acetaminophen.
-
Hydration: Helps prevent urinary retention and flush out bacteria.
-
Monitoring for Complications: Watch for fever, heavy bleeding, or inability to urinate.
Complications of Prostate Biopsy
Although generally safe, complications can occur:
-
Infection
-
Mild: Fever, urinary tract irritation.
-
Severe: Sepsis requiring hospitalization.
-
-
Bleeding
-
Hematuria (blood in urine) and hematochezia (blood in stool) are common but usually resolve.
-
Hematospermia (blood in semen) may persist for weeks.
-
-
Urinary Retention
-
Swelling or blood clots may obstruct urine flow.
-
-
Pain or Discomfort
-
Rectal or perineal soreness for a few days.
-
-
Rare Complications
-
Injury to adjacent organs (very rare).
-
Long-term infections or prostatitis.
-
Living with the Condition of Prostate Biopsy
While a prostate biopsy is a diagnostic step, living with its results and the follow-up care is crucial:
Emotional Wellbeing
-
Anxiety related to cancer diagnosis is common; counseling may be helpful.
-
Support groups or peer counseling can reduce stress and improve coping mechanisms.
Lifestyle Considerations
-
Maintain a healthy diet rich in fruits, vegetables, and fiber.
-
Regular exercise improves urinary and cardiovascular health.
-
Follow recommended screening schedules and PSA monitoring if the biopsy was benign or cancer detected.
Follow-Up
-
Repeat biopsies may be needed if PSA rises or imaging suggests abnormalities.
-
Patients with low-grade cancer may undergo active surveillance, avoiding overtreatment.
-
Those undergoing treatment based on biopsy results must manage side effects such as urinary incontinence, erectile dysfunction, or fatigue.
Top 10 Frequently Asked Questions about Prostate Biopsy
1. What is a prostate biopsy?
A prostate biopsy is a medical procedure in which small samples of tissue are taken from the prostate gland to check for the presence of prostate cancer or other abnormalities. It is usually performed when blood tests (PSA) or imaging indicate a potential issue with the prostate.
2. Why is a prostate biopsy recommended?
A prostate biopsy is recommended when:
-
Blood tests show elevated prostate-specific antigen (PSA) levels.
-
There are abnormal findings during a digital rectal exam (DRE).
-
Imaging studies, such as MRI or ultrasound, suggest suspicious areas in the prostate.
It helps in early detection and diagnosis of prostate cancer, which improves treatment outcomes.
3. How is a prostate biopsy performed?
The procedure can be done in several ways:
-
Transrectal biopsy (TRUS-guided): A needle is inserted through the rectum under ultrasound guidance.
-
Transperineal biopsy: A needle is inserted through the skin between the scrotum and rectum.
-
MRI-guided biopsy: Combines MRI imaging with real-time ultrasound to target specific suspicious areas.
Multiple tissue samples are collected and sent to a lab for pathological examination.
4. Does a prostate biopsy hurt?
Most patients experience mild discomfort or pressure during the procedure. Local anesthesia is typically used, and sometimes sedation is provided. After the biopsy, mild pain, bruising, or blood in urine or stool is common but usually resolves within a few days.
5. Are there any risks associated with a prostate biopsy?
While generally safe, risks may include:
-
Bleeding from the rectum, urine, or semen.
-
Infection, which may require antibiotics.
-
Temporary difficulty urinating or urinary retention.
-
Rarely, severe infection or sepsis may occur. Your doctor will provide instructions to minimize risks before and after the biopsy.
6. How should I prepare for a prostate biopsy?
Preparation steps may include:
-
Informing your doctor about medications, especially blood thinners.
-
Fasting, if sedation is planned.
-
Taking a prophylactic antibiotic as prescribed to reduce infection risk.
-
Bowel preparation, if required, such as an enema for transrectal biopsy.
7. How long does it take to get results?
After the biopsy, tissue samples are sent to a pathology lab. Results usually take 5-10 days, depending on the laboratory. The report will indicate whether cancer cells or other abnormalities are present, and further treatment decisions will be based on the findings.
8. What happens if cancer is found?
If prostate cancer is detected, your doctor may discuss:
-
Active surveillance for slow-growing cancers.
-
Surgical options, such as prostatectomy.
-
Radiation therapy or hormonal therapy.
The choice of treatment depends on cancer stage, grade, PSA levels, age, and overall health.
9. Can a prostate biopsy miss cancer?
Yes, there is a small chance that a biopsy may miss cancer, especially if it is small or located in an area not sampled. If suspicion remains high, your doctor may recommend:
-
Repeat biopsy.
-
MRI-guided targeted biopsy.
-
Additional imaging or tests to confirm diagnosis.
10. What should I expect after the biopsy?
After a prostate biopsy, you may notice:
-
Mild pain, bruising, or swelling in the biopsy area.
-
Blood in urine, stool, or semen for a few days.
-
Temporary difficulty urinating in some cases.
Most patients recover within a week. You should report fever, severe pain, or persistent bleeding to your doctor immediately, as these may indicate complications.