Introduction to Pseudopancreatic Cyst
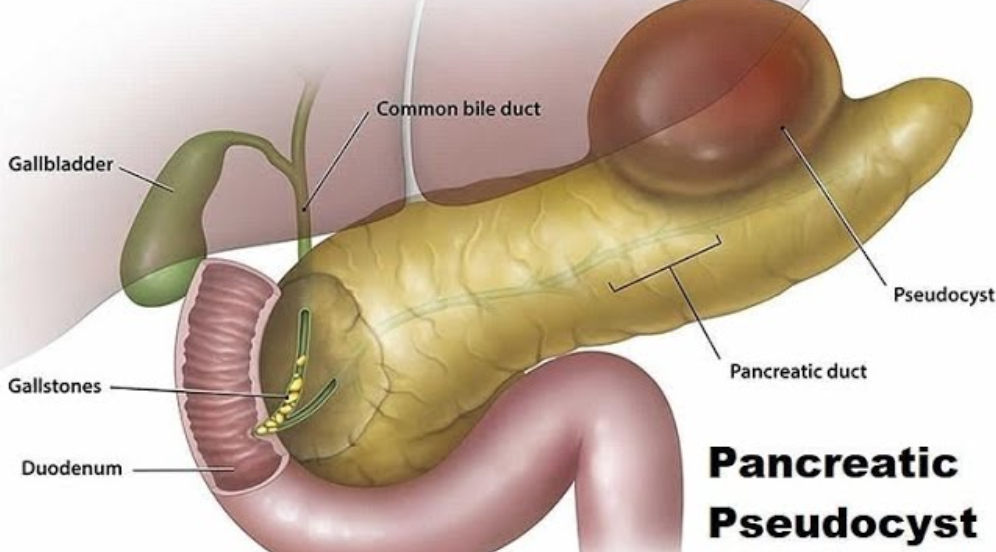
A pseudopancreatic cyst, also known simply as a pancreatic pseudocyst, is a fluid-filled sac that forms in the pancreas, often following inflammation or injury. Unlike true cysts, pseudocysts are not lined with epithelial cells; instead, their walls are composed of fibrous and granulation tissue, giving them a “pseudo” lining.
These cysts can range from small, asymptomatic lesions to large, symptomatic masses causing significant complications. They are most commonly associated with acute or chronic pancreatitis, pancreatic trauma, or pancreatic ductal obstructions.
Key Features
-
Fluid-filled, encapsulated sacs in or around the pancreas.
-
Wall formation occurs over 4-6 weeks after pancreatic injury or inflammation.
-
Can contain enzymes, necrotic tissue, or blood.
-
Most pseudocysts resolve spontaneously, but some require medical or surgical intervention.
Pseudopancreatic cysts account for approximately 10-20% of pancreatic cystic lesions and are more common in men aged 30-50 years.
Causes and Risk of Pseudopancreatic Cyst
A pseudopancreatic cyst is a fluid-filled sac that forms in or around the pancreas, typically after pancreatic injury or inflammation. Unlike true cysts, pseudocysts do not have an epithelial lining, and their walls are made of fibrous or granulation tissue. Understanding the causes and risk factors helps in prevention, early detection, and management.
Common Causes
-
Acute Pancreatitis
-
The most frequent cause.
-
Enzyme leakage during inflammation can lead to fluid accumulation.
-
-
Chronic Pancreatitis
-
Recurrent inflammation results in ductal obstruction and cyst formation.
-
-
Pancreatic Trauma
-
Blunt abdominal trauma or surgical injury can lead to pseudocyst development.
-
-
Pancreatic Duct Obstruction
-
Tumors or gallstones may block fluid flow, increasing cyst risk.
-
-
Post-Surgical Complications
-
Complications from procedures such as pancreatic resection or distal pancreatectomy.
-
Risk Factors
-
Excessive alcohol consumption (major risk factor for pancreatitis).
-
Gallstones obstructing the pancreatic duct.
-
Male gender (more common in men).
-
Age (most common between 30-50 years).
-
Hypertriglyceridemia and metabolic disorders.
-
History of pancreatic trauma or surgery.
Symptoms and Signs of Pseudopancreatic Cyst
A pseudopancreatic cyst is a fluid-filled sac that typically forms in or around the pancreas, often as a result of pancreatitis, trauma, or pancreatic duct obstruction. Unlike true cysts, pseudocysts lack an epithelial lining and are instead surrounded by fibrous tissue. The symptoms can vary depending on the cyst’s size, location, and complications.
Common Symptoms
-
Abdominal pain: Typically in the upper abdomen, sometimes radiating to the back.
-
Nausea and vomiting: Due to gastric or duodenal compression.
-
Early satiety and bloating: Caused by pressure on the stomach.
-
Palpable abdominal mass: In some large cysts.
-
Weight loss: Due to reduced appetite or malabsorption.
Red Flag Symptoms
-
Fever or chills: Suggests infection of the cyst (infected pseudocyst).
-
Jaundice: Indicates bile duct compression.
-
Hypotension or shock: Rare but can occur in hemorrhagic pseudocysts.
Complications Presenting with Symptoms
-
Rapidly enlarging cysts may rupture, causing peritonitis.
-
Compression of blood vessels may cause portal hypertension.
-
Pancreatic enzyme leakage may result in systemic inflammation.
Diagnosis of Pseudopancreatic Cyst
Diagnosing a pseudopancreatic cyst involves a combination of clinical evaluation, laboratory tests, and imaging studies. Accurate diagnosis is crucial, as pseudocysts can mimic other pancreatic or abdominal conditions, and early detection helps prevent complications.
Clinical Assessment
-
History of pancreatitis, trauma, or pancreatic surgery.
-
Symptom evaluation (abdominal pain, nausea, early satiety).
-
Physical examination (palpable mass, tenderness).
Laboratory Tests
-
Serum amylase and lipase: Often elevated in acute pseudocysts.
-
Liver function tests: Elevated if bile duct compression occurs.
-
Complete blood count (CBC): Detects infection or anemia.
-
Tumor markers: CA 19-9 or CEA to rule out cystic neoplasms.
Imaging Techniques
-
Ultrasound (USG)
-
Initial screening tool.
-
Detects fluid-filled lesions but may miss small cysts.
-
-
Contrast-Enhanced CT Scan
-
Gold standard for detecting size, location, and complications.
-
Differentiates pseudocysts from neoplastic cysts.
-
-
Magnetic Resonance Imaging (MRI) / MRCP
-
Useful for ductal anatomy and cyst characterization.
-
-
Endoscopic Ultrasound (EUS)
-
Provides high-resolution images and allows for fine-needle aspiration (FNA) for fluid analysis.
-
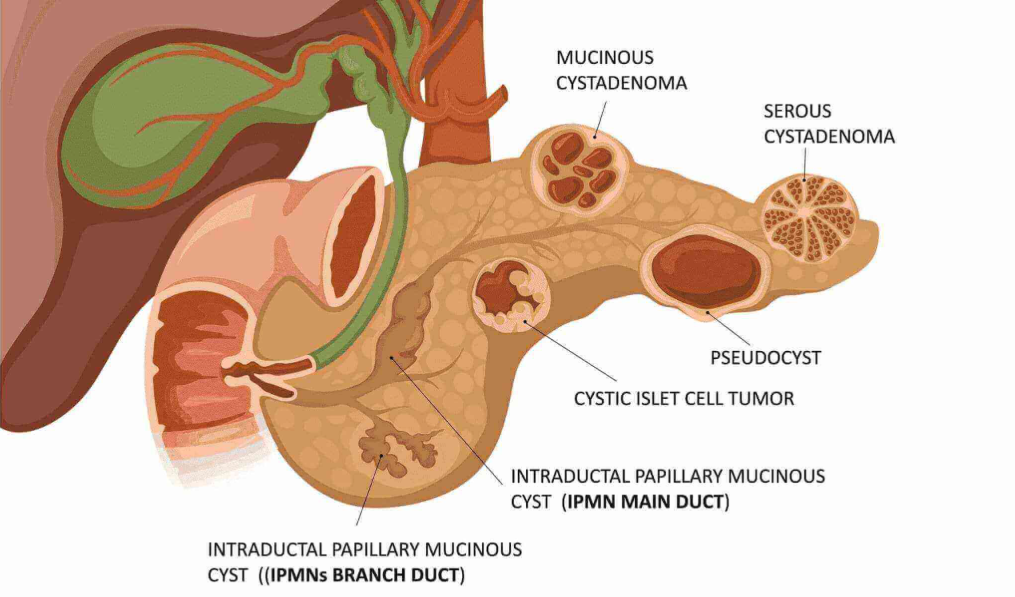
Differential Diagnosis
-
True pancreatic cysts (cystic neoplasms)
-
Cystic pancreatic tumors (mucinous or serous)
-
Abscess or pancreatic necrosis
-
Gastrointestinal duplication cysts
Treatment Options of Pseudopancreatic Cyst
Pseudopancreatic cysts are fluid-filled sacs in or around the pancreas that usually develop after pancreatitis, pancreatic trauma, or occasionally due to pancreatic tumors. The treatment approach depends on the cyst’s size, location, symptoms, risk of complications, and whether it is infected or causing obstruction.
Conservative Management
-
Recommended for asymptomatic cysts <5 cm.
-
Includes:
-
Regular imaging surveillance (USG or CT every 4-6 weeks initially).
-
Monitoring pancreatic enzyme levels.
-
Lifestyle modifications (avoid alcohol and fatty foods).
-
Endoscopic Treatment
-
Endoscopic Drainage
-
Transgastric or transduodenal approach under EUS guidance.
-
Stents may be placed to maintain drainage.
-
-
Endoscopic Cystogastrostomy
-
Creates a connection between cyst and stomach to allow continuous drainage.
-
Percutaneous Drainage
-
For cysts not amenable to endoscopic drainage.
-
Image-guided (CT or USG) with a catheter to drain cyst fluid.
Surgical Treatment
Indicated for complicated, persistent, or large cysts (>6 cm) or if malignancy is suspected.
-
Open cystogastrostomy or cystojejunostomy
-
Pancreatic resection for cysts with neoplastic potential or severe complications
Adjunctive Treatments
-
Pain management
-
Nutritional support
-
Antibiotics for infected pseudocysts
Prevention and Management of Pseudopancreatic Cyst
A pseudopancreatic cyst is a fluid-filled sac that forms in the pancreas, usually as a result of pancreatitis (inflammation of the pancreas) or pancreatic trauma. Unlike true cysts, pseudocysts are not lined by epithelial cells; instead, their walls are made of fibrous and granulation tissue. While some pseudocysts may resolve on their own, others can lead to complications such as infection, bleeding, rupture, or obstruction of adjacent organs. Therefore, prevention and effective management are crucial for minimizing risks and maintaining pancreatic health.
Preventive Strategies
-
Reduce risk factors for pancreatitis:
-
Limit alcohol intake
-
Manage gallstones
-
Control triglyceride levels
-
-
Early management of pancreatic injury or inflammation
Ongoing Management
-
Regular follow-up imaging to monitor cyst regression or growth
-
Pancreatic enzyme supplements if exocrine function is impaired
-
Dietary adjustments: Small, low-fat meals
Complications of Pseudopancreatic Cyst
Pseudopancreatic cysts are fluid-filled sacs that develop in or around the pancreas, usually following pancreatitis or pancreatic injury. While some cysts remain small and asymptomatic, larger or untreated cysts can lead to serious complications. Understanding these potential risks is crucial for timely management.
-
Infection
-
Can lead to abscess formation, sepsis.
-
-
Hemorrhage
-
Erosion into blood vessels may cause life-threatening bleeding.
-
-
Rupture
-
Spillage into peritoneal cavity causes peritonitis.
-
-
Obstruction
-
Gastric outlet or bile duct compression leading to vomiting or jaundice.
-
-
Chronic Pancreatitis
-
Recurrent cysts may cause ongoing pancreatic inflammation.
-
-
Malignant Transformation
-
Rare, usually associated with misdiagnosis of neoplastic cysts.
-
Living with the Condition of Pseudopancreatic Cyst
A pseudopancreatic cyst is a fluid-filled sac that forms in or around the pancreas, usually as a result of pancreatitis, trauma, or pancreatic duct obstruction. While some cysts may resolve on their own, others persist and can lead to complications. Learning how to live with this condition involves careful monitoring, lifestyle adjustments, and understanding warning signs that require medical attention.
Lifestyle Considerations
-
Avoid alcohol, smoking, and fatty foods.
-
Maintain hydration and balanced nutrition.
-
Engage in moderate physical activity.
Monitoring and Follow-Up
-
Regular imaging every 4-12 weeks depending on cyst size and symptoms.
-
Report new symptoms promptly (pain, jaundice, fever).
-
Maintain long-term follow-up with a gastroenterologist or pancreatic specialist.
Psychological Support
-
Anxiety about cyst progression is common.
-
Counseling and support groups help patients cope with uncertainty.
Prognosis
-
Most small pseudocysts resolve spontaneously.
-
With timely intervention, complicated cysts have excellent outcomes.
-
Persistent or recurrent cysts require monitoring for pancreatic function.
Top 10 Frequently Asked Questions about Pseudopancreatic Cysts
1. What is a pseudopancreatic cyst?
A pseudopancreatic cyst is a fluid-filled sac that forms in the abdomen, typically around the pancreas, as a complication of acute or chronic pancreatitis. Unlike true cysts, these do not have an epithelial lining; instead, they are surrounded by fibrous tissue or granulation tissue.
2. What causes a pseudopancreatic cyst?
The most common causes include:
-
Acute pancreatitis - inflammation of the pancreas leading to fluid accumulation.
-
Chronic pancreatitis - prolonged inflammation causing persistent damage.
-
Abdominal trauma - injury to the pancreas.
-
Blockage of pancreatic ducts - due to gallstones, tumors, or scarring.
3. What are the common symptoms of a pseudopancreatic cyst?
Symptoms vary based on size and location but may include:
-
Upper abdominal pain or discomfort
-
Nausea and vomiting
-
Loss of appetite and weight loss
-
Fever and chills (if infected)
-
Feeling of fullness or abdominal mass
-
Jaundice (if the cyst compresses bile ducts)
4. How is a pseudopancreatic cyst diagnosed?
Doctors use a combination of clinical evaluation and imaging tests, including:
-
Ultrasound - first-line imaging to detect cysts.
-
CT scan or MRI - detailed imaging to determine size, number, and complications.
-
Endoscopic Ultrasound (EUS) - provides high-resolution images and allows guided drainage if necessary.
-
Blood tests - to assess pancreatic enzyme levels and detect infection.
5. Are pseudopancreatic cysts dangerous?
While many pseudopancreatic cysts resolve on their own, complications can arise if left untreated, such as:
-
Infection leading to abscess formation
-
Rupture causing severe abdominal bleeding or peritonitis
-
Compression of nearby organs, like bile ducts or intestines
-
Hemorrhage within the cyst
Early diagnosis and management help prevent these risks.
6. What are the treatment options for pseudopancreatic cysts?
Treatment depends on the size, symptoms, and complications:
-
Observation - small, asymptomatic cysts may resolve naturally.
-
Endoscopic drainage - inserting a tube to drain cyst fluid.
-
Percutaneous drainage - needle-guided drainage through the skin.
-
Surgical drainage or removal - for persistent, large, or complicated cysts.
-
Antibiotics - used if infection is present.
7. When is surgical intervention necessary?
Surgery is typically required when:
-
The cyst is larger than 6 cm and persists beyond 6 weeks.
-
Symptoms like pain, jaundice, or digestive obstruction occur.
-
There is infection or internal bleeding.
-
The cyst continues to grow despite conservative management.
8. Can pseudopancreatic cysts recur after treatment?
Yes, recurrence is possible, especially in patients with chronic pancreatitis or ongoing alcohol abuse. Preventing recurrence involves treating the underlying cause, such as avoiding alcohol, managing gallstones, and maintaining a healthy pancreas.
9. What lifestyle changes help manage and prevent pseudopancreatic cysts?
-
Avoid alcohol and smoking, as they worsen pancreatic damage.
-
Eat a low-fat, balanced diet to reduce pancreatic stress.
-
Manage gallstones if present.
-
Control diabetes and other metabolic conditions.
-
Follow up regularly with your doctor to monitor cyst size and function.
10. What is the long-term outlook for patients with pseudopancreatic cysts?
With early diagnosis and appropriate management, the prognosis is generally good. Most small cysts resolve spontaneously, but large or complicated cysts may require drainage or surgery. Regular follow-ups and imaging are essential to avoid recurrence and detect complications early.