Introduction to Pure Tone Audiometry (PTA)
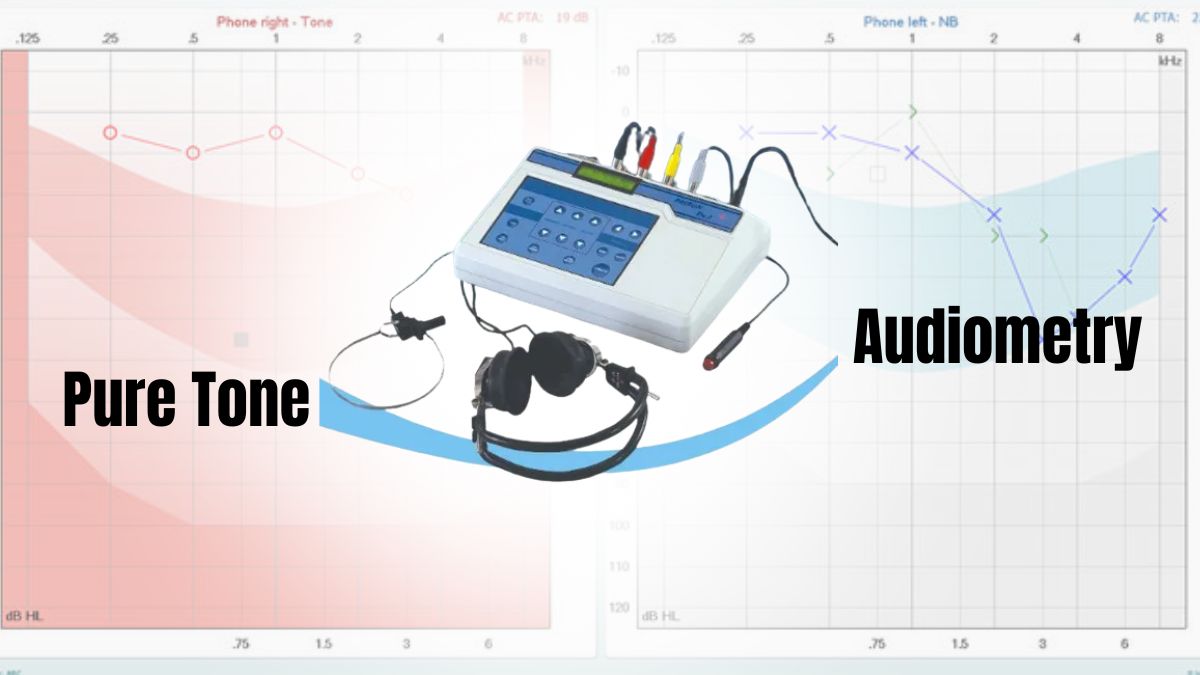
Pure Tone Audiometry (PTA) is a standard hearing test used to assess an individual's hearing ability. It measures the softest sounds a person can hear at different frequencies or pitches. This test is fundamental in diagnosing hearing loss and determining the type, degree, and configuration of any hearing impairment. PTA is commonly used by audiologists in both clinical and diagnostic settings to evaluate patients' hearing and guide treatment options.
During PTA, the patient wears headphones or ear inserts, and a series of pure tones (single-frequency sounds) are presented at varying volumes. The test involves testing air conduction (sounds transmitted through the outer and middle ear) and bone conduction (sounds transmitted through the bones of the skull to the inner ear). By presenting these tones across a range of frequencies (usually from 250 Hz to 8000 Hz), the audiologist can determine the threshold at which the patient can hear each sound.
The results of the PTA are recorded on an audiogram, a graph that shows the hearing threshold for each frequency tested. This helps identify whether the hearing loss is conductive (caused by issues in the outer or middle ear), sensorineural (caused by inner ear or nerve issues), or mixed (a combination of both).
Pure Tone Audiometry is widely used to identify hearing impairments, monitor changes in hearing, and plan treatment such as hearing aids, surgical interventions, or speech therapy. It is a non-invasive, simple, and reliable diagnostic tool that provides critical information to manage hearing health effectively.
Causes and Risk of Pure Tone Audiometry
Pure Tone Audiometry (PTA) is a hearing test that is commonly used to assess an individual's hearing sensitivity across a range of frequencies. While PTA is a diagnostic tool rather than a condition itself, it helps identify underlying hearing issues. The causes of hearing loss or abnormalities detected through PTA can be attributed to several factors, as outlined below:
Common Causes of Hearing Loss
Conductive Hearing Loss
-
Middle Ear Infections (Otitis Media): Fluid accumulation in the middle ear due to infection can cause temporary conductive hearing loss.
-
Otosclerosis: Abnormal bone growth in the middle ear impedes the movement of the ossicles (small bones in the ear).
-
Tympanic Membrane Perforation: A hole or tear in the eardrum affects sound transmission.
-
Foreign Bodies or Wax Impaction: Obstruction in the ear canal can cause conductive hearing loss.
-
Eustachian Tube Dysfunction: The tube connecting the middle ear to the throat may become blocked, affecting equalization of ear pressure.
Sensorineural Hearing Loss
-
Aging (Presbycusis): Age-related degeneration of the cochlea and auditory nerve fibers results in high-frequency hearing loss.
-
Noise-Induced Hearing Loss (NIHL): Prolonged exposure to loud noises (e.g., concerts, machinery, or heavy machinery) damages hair cells in the cochlea.
-
Genetic Factors: Inherited conditions such as Usher syndrome and Pendred syndrome can lead to congenital or progressive sensorineural hearing loss.
-
Ototoxic Medications: Certain medications, including aminoglycoside antibiotics and chemotherapy agents, can damage the inner ear.
-
Infections: Meningitis, measles, and other infections may cause sensorineural hearing loss, especially in children.
Mixed Hearing Loss
-
Combination of Conductive and Sensorineural Loss: This occurs when an individual has both a middle ear problem (conductive) and inner ear damage (sensorineural).
Risk Factors
-
Age: Older adults experience presbycusis or age-related hearing loss.
-
Occupational Noise Exposure: Individuals working in noisy environments, such as factories, airports, or construction sites, are at higher risk of NIHL.
-
Medical Conditions: Hypertension, diabetes, and cardiovascular diseases have been associated with increased risk of hearing loss.
-
Family History: Genetic predisposition plays a significant role in both congenital and acquired hearing loss.
Symptoms and Signs of Hearing Loss
Hearing loss can develop gradually or suddenly, and the symptoms may vary depending on the cause and severity. It's important to recognize the signs early, as untreated hearing loss can impact communication, relationships, and quality of life. Below are common symptoms and signs of hearing loss:
Symptoms of Hearing Loss
-
Difficulty Understanding Speech: Struggling to follow conversations, particularly in noisy settings.
-
Asking for Repetition: Frequently asking people to repeat themselves, especially in group settings.
-
Turning Up Volume: Turning up the TV, radio, or phone volume louder than before.
-
Tinnitus: Ringing, buzzing, or hissing sounds in the ears, often occurring with hearing loss.
-
Withdrawal from Social Situations: Avoiding social interactions due to difficulty hearing or misunderstanding conversations.
-
Fullness in the Ear: Feeling of pressure or fullness in the ears, especially in conductive hearing loss.
Signs Observed by Family and Friends
-
Louder Speech: The individual may speak louder than usual without realizing it.
-
Misunderstanding Conversations: Responding incorrectly or inappropriately in conversations.
-
Frequent Complaints: Complaints about not hearing well, particularly in noisy environments.
Diagnosis Using Pure Tone Audiometry
Pure Tone Audiometry (PTA) is one of the most common and reliable tests used for diagnosing hearing loss. It measures an individual's ability to hear sounds at various frequencies and volumes, allowing healthcare professionals to identify the presence and extent of hearing loss.
How PTA Is Performed
-
Test Setup: The patient is seated comfortably in a soundproof room wearing headphones or bone conduction devices.
-
Tone Presentation: A series of pure tones at different frequencies (250 Hz - 8,000 Hz) is presented to each ear at varying intensity levels.
-
Threshold Testing: The audiologist identifies the softest tone that the patient can hear at each frequency, called the hearing threshold. The process is repeated for both air conduction and bone conduction.
Air Conduction vs. Bone Conduction
-
Air Conduction Testing: Sounds are delivered through headphones and travel through the outer and middle ear.
-
Bone Conduction Testing: A bone oscillator is placed on the skull to directly stimulate the inner ear, bypassing the outer and middle ear. This test helps assess sensorineural hearing loss.
Audiogram Results
The test results are plotted on an audiogram. The audiogram is a graphical representation of the patient's hearing thresholds at different frequencies. It helps:
-
Determine the degree of hearing loss (mild, moderate, severe, profound).
-
Identify the type of hearing loss: conductive, sensorineural, or mixed.
-
Assess the configuration of the hearing loss, which can provide insights into specific pathologies.
Types of Hearing Loss Identified by PTA
-
Conductive Hearing Loss: A gap between air conduction and bone conduction thresholds.
-
Sensorineural Hearing Loss: Both air conduction and bone conduction thresholds are elevated similarly.
-
Mixed Hearing Loss: There's a gap between air conduction and bone conduction thresholds, and both are elevated.
Treatment Options for Hearing Loss
Hearing loss can significantly impact quality of life, but there are various treatment options available depending on the cause, type, and severity of the hearing impairment. These options range from medical treatments and surgical interventions to assistive devices.
For Conductive Hearing Loss
-
Medical Treatment: For infections or inflammation (e.g., antibiotics for otitis media or decongestants for Eustachian tube dysfunction).
-
Surgical Treatment: Procedures like stapedectomy (for otosclerosis) or tympanoplasty (to repair the eardrum) to improve sound conduction.
-
Hearing Aids: Can help amplify sound, especially in mild-to-moderate conductive hearing loss.
For Sensorineural Hearing Loss
-
Hearing Aids: Amplify sound for individuals with mild-to-moderate hearing loss.
-
Cochlear Implants: For severe or profound sensorineural hearing loss, cochlear implants bypass damaged hair cells in the cochlea and directly stimulate the auditory nerve.
-
Assistive Listening Devices (ALDs): Devices such as FM systems or television amplifiers that help in noisy environments.
For Mixed Hearing Loss
-
Combination treatments addressing both the conductive and sensorineural components of the hearing loss.
Prevention and Management of Hearing Loss
Hearing loss can be caused by various factors, including aging, genetics, noise exposure, infections, and injuries. While some causes of hearing loss are unavoidable, there are effective strategies for prevention and management to minimize the impact of hearing loss and enhance overall hearing health.
Preventive Strategies
-
Avoidance of Loud Noises: Use ear protection when exposed to loud environments.
-
Healthy Lifestyle: Control conditions like hypertension and diabetes, which are linked to hearing loss.
-
Regular Hearing Check-ups: For individuals at risk, such as those exposed to loud noise, older adults, and individuals with a family history of hearing loss.
-
Vaccination: Prevent infections that could lead to hearing loss, such as measles and mumps.
Management of Existing Hearing Loss
-
Hearing Aids: Regular maintenance and adjustment for best hearing support.
-
Speech Therapy: For individuals with hearing loss, particularly children, to improve language skills.
-
Support and Counseling: Emotional support for individuals and families to cope with the challenges of hearing impairment.
Complications of Untreated Hearing Loss
Untreated hearing loss can lead to a variety of complications that affect both physical health and quality of life. Here are some of the key complications:
Social Complications
-
Isolation: Difficulty communicating can lead to withdrawal from social activities.
-
Depression and Anxiety: Psychological impacts of feeling disconnected or misunderstood.
Cognitive Impairment
-
Studies have shown that untreated hearing loss, especially in the elderly, is associated with an increased risk of cognitive decline and dementia.
Speech and Language Delays
-
In children, untreated hearing loss can delay the development of speech and language skills.
Living with the Condition of Pure Tone Audiometry
Living with hearing loss diagnosed through Pure Tone Audiometry (PTA) involves adjusting to the changes in your hearing ability. If PTA results show hearing loss, it may affect communication and daily activities. Here are key aspects to manage:
Coping Strategies
-
Speech-to-Text Apps: Many smartphones now offer speech-to-text functionality, aiding individuals with hearing loss.
-
Lip Reading: Learning to read lips can be a useful skill, particularly in one-on-one conversations.
-
Sign Language: A complete form of communication, particularly useful for severe or profound hearing loss.
Support Systems
-
Hearing Loss Support Groups: Connecting with others facing similar challenges can provide valuable emotional support and coping strategies.
-
Professional Counseling: For patients experiencing depression or anxiety related to hearing loss.
Top 10 Frequently Asked Questions about Pure Tone Audiometry
1. What is Pure Tone Audiometry?
Pure Tone Audiometry (PTA) is a hearing test used to evaluate an individual's ability to hear different pitches or frequencies of sound. It involves presenting a series of pure tones through headphones and recording the quietest sound that can be heard at each frequency. PTA is one of the most common and reliable methods to assess hearing loss.
2. Why is Pure Tone Audiometry performed?
Pure Tone Audiometry is performed to:
-
Diagnose hearing loss and its severity
-
Identify the type of hearing loss (sensorineural, conductive, or mixed)
-
Monitor hearing changes over time
-
Assess hearing function before and after treatments or interventions like surgery or hearing aids.
3. How is Pure Tone Audiometry performed?
The test is simple and involves:
-
A quiet room where the patient wears headphones or earphones.
-
The audiologist presents a series of pure tones at different frequencies and volumes.
-
The patient is asked to indicate when they hear each tone.
-
Results are plotted on an audiogram to assess hearing levels for each frequency.
4. What frequencies are tested in Pure Tone Audiometry?
Pure Tone Audiometry tests a range of frequencies, typically between 250 Hz to 8,000 Hz. These frequencies cover most sounds found in everyday speech. The test checks for the patient's hearing threshold at various frequencies to identify any hearing deficits.
5. What is an audiogram and how is it used?
An audiogram is a graphical representation of the results from Pure Tone Audiometry. It shows the quietest sound a person can hear at different frequencies (measured in decibels, dB). The audiogram helps identify the type and degree of hearing loss, and it is crucial in planning treatment options such as hearing aids or medical interventions.
6. What are the types of hearing loss that can be detected by Pure Tone Audiometry?
PTA can help identify three types of hearing loss:
-
Conductive Hearing Loss: Occurs due to problems in the outer or middle ear, such as ear infections or earwax buildup.
-
Sensorineural Hearing Loss: Caused by damage to the inner ear or auditory nerve, often due to aging, noise exposure, or genetics.
-
Mixed Hearing Loss: A combination of both conductive and sensorineural hearing loss.
7. What does it mean if the results show hearing loss?
If the results of the Pure Tone Audiometry show hearing loss, it means that the patient has difficulty hearing sounds within certain frequencies. The severity can be classified as:
-
Mild: Difficulty hearing soft sounds
-
Moderate: Difficulty hearing normal speech
-
Severe: Cannot hear loud sounds
-
Profound: Cannot hear any sound
8. Are there any risks or side effects from Pure Tone Audiometry?
No, Pure Tone Audiometry is a non-invasive and safe procedure. It doesn't involve any medical intervention, and there are no risks or side effects. The test is generally comfortable, although patients might experience temporary discomfort from wearing headphones for an extended period.
9. How long does a Pure Tone Audiometry test take?
A typical Pure Tone Audiometry test usually takes about 15 to 30 minutes. The duration may vary based on the complexity of the test and the patient's cooperation, especially in children or individuals with special needs.
10. Who should undergo Pure Tone Audiometry?
Pure Tone Audiometry is recommended for:
-
Children who may have hearing problems.
-
Adults who experience symptoms like muffled hearing, difficulty understanding speech, or ringing in the ears.
-
People exposed to high noise levels at work or in recreational activities.
-
Individuals with a family history of hearing loss.
-
Elderly individuals as part of regular health assessments for age-related hearing loss.


