Introduction to SRT (Stereotactic Radiation Therapy)
Stereotactic Radiation Therapy (SRT) represents one of the most important advances in modern cancer treatment and neurosurgical care. It is a non-invasive technique that delivers highly focused radiation beams with extreme accuracy to treat malignant tumors, benign growths, and certain non-cancerous abnormalities. Unlike traditional external beam radiation therapy, which often involves exposing large areas of healthy tissue to radiation, SRT narrows its scope to a precisely defined target. This precision is possible due to the integration of high-resolution imaging technologies—such as Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and Positron Emission Tomography (PET)—with advanced computer-assisted treatment planning.
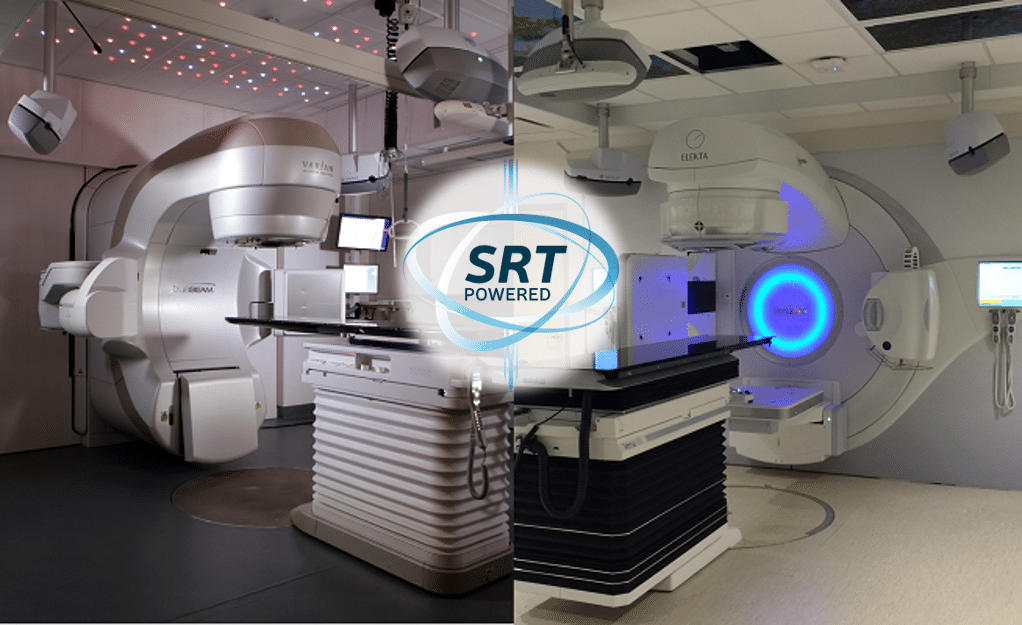
SRT can be delivered in a single session (Stereotactic Radiosurgery or SRS) or in multiple sessions (Fractionated SRT or FSRT), depending on the size, type, and location of the lesion. Outside the brain, SRT is applied as Stereotactic Body Radiation Therapy (SBRT), offering life-saving treatment options for lung, liver, pancreatic, and spinal tumors. Devices such as the Gamma Knife, CyberKnife, and Linear Accelerators (LINACs) are most commonly used to deliver these therapies.
The importance of SRT lies not only in its effectiveness but also in its reduced invasiveness. Patients who are not suitable for surgery due to medical comorbidities, tumor location, or advanced age can often undergo SRT with minimal disruption to their daily lives. Over the last two decades, clinical studies have confirmed that SRT provides local tumor control rates comparable to surgery, with fewer complications, quicker recovery times, and better preservation of quality of life.
Causes and Risk of SRT (Stereotactic Radiation Therapy)
SRT itself is not a disease—it is a treatment modality. To understand why SRT is necessary, one must examine the conditions and diseases that typically require this therapy, as well as the risk factors that predispose patients to these conditions.
Causes of Conditions Treated by SRT:
-
Genetic Mutations: Abnormalities in DNA can trigger uncontrolled cell division leading to tumor development. For example, mutations in genes like TP53 or EGFR are linked to brain and lung cancers.
-
Environmental Exposures: Prolonged exposure to carcinogens such as tobacco smoke, industrial chemicals, and ionizing radiation can increase cancer risk.
-
Infections: Certain viruses, such as Epstein-Barr Virus (EBV), Human Papillomavirus (HPV), and Hepatitis B/C, are linked to specific tumors treatable by SRT.
-
Vascular Malformations: Congenital anomalies such as arteriovenous malformations (AVMs) in the brain can be managed with SRT when surgery poses high risks.
-
Benign Growths: Acoustic neuromas, meningiomas, and pituitary adenomas, though non-cancerous, may cause severe neurological symptoms due to their location, requiring targeted treatment.
Risk Factors:
-
Age: Risk of cancers and degenerative vascular changes rises with age.
-
Family History: Genetic predisposition to tumors may lead to the need for early interventions like SRT.
-
Lifestyle Choices: Smoking, alcohol consumption, and poor diet increase the incidence of lung, liver, and other cancers.
-
Medical Inoperability: Patients with comorbidities such as heart disease or diabetes may not tolerate surgery and are prime candidates for SRT.
-
Recurrence of Tumors: SRT is often recommended for tumors that return after conventional surgery or radiation.
Symptoms and Signs of SRT (Stereotactic Radiation Therapy)
The clinical presentation varies based on the organ affected. Because SRT targets localized lesions, understanding the symptoms and signs of underlying conditions is essential for timely diagnosis.
-
Brain Tumors: Persistent or worsening headaches, seizures, nausea, visual disturbances, memory issues, weakness in limbs, and difficulty with speech or balance.
-
Spinal Tumors: Localized back pain, tingling sensations, limb weakness, difficulty walking, and in severe cases, loss of bladder or bowel control.
-
Lung Tumors (treated with SBRT): Chronic cough, chest pain, coughing up blood (hemoptysis), shortness of breath, and recurrent lung infections.
-
Liver Tumors: Abdominal swelling, pain in the upper right quadrant, jaundice, loss of appetite, and unexplained weight loss.
-
Benign Conditions (e.g., Acoustic Neuroma): Hearing loss, tinnitus (ringing in the ear), dizziness, and facial numbness.
-
Trigeminal Neuralgia: Intense, stabbing facial pain triggered by eating, talking, or brushing teeth, which may be effectively managed with radiosurgery.
Diagnosis of SRT (Stereotactic Radiation Therapy)
A thorough diagnostic process ensures that only patients who will benefit from SRT undergo the procedure. The diagnostic journey includes:
-
Initial Assessment: Patient history, physical examination, and neurological evaluations.
-
Imaging Tests:
-
MRI: Provides detailed images of the brain, spine, or other tissues to assess tumor size and position.
-
CT Scan: Helps create a three-dimensional treatment map.
-
PET Scan: Identifies metabolic activity and distinguishes between active tumors and scar tissue.
-
-
Histopathology: Biopsy may be performed to confirm tumor type, though not always required in cases where imaging is definitive.
-
Functional Imaging: In the case of brain tumors, advanced scans map speech and motor areas to avoid radiation damage to critical brain regions.
-
Multidisciplinary Tumor Board: Oncologists, neurosurgeons, and radiologists collaborate to determine whether SRT is the best option, often weighing alternatives such as surgery, chemotherapy, or immunotherapy.
Treatment Options of SRT (Stereotactic Radiation Therapy)
SRT is not a single method but a family of techniques tailored to patient needs:
-
Stereotactic Radiosurgery (SRS): Single high-dose treatment for small brain lesions, metastases, or AVMs.
-
Fractionated SRT (FSRT): Administers multiple smaller doses over days or weeks to protect sensitive tissue around larger or irregular tumors.
-
Stereotactic Body Radiation Therapy (SBRT): Targets tumors in the lung, liver, pancreas, prostate, or spine with extreme precision.
Step-by-Step Treatment Process:
-
Patient Immobilization: A rigid mask or stereotactic frame is used for head treatments; vacuum cushions for body tumors.
-
Treatment Planning: Computer software integrates imaging scans to design radiation beams tailored to the tumor’s shape.
-
Radiation Delivery: Robotic arms (CyberKnife) or rotating machines (Gamma Knife, LINACs) deliver high-dose radiation.
-
Post-Treatment Monitoring: Patients are observed briefly and usually return home the same day.
Prevention and Management of SRT (Stereotactic Radiation Therapy)
While SRT manages disease, prevention focuses on lowering cancer risks:
-
Lifestyle Measures: No smoking, moderate alcohol intake, regular exercise, and a balanced diet.
-
Vaccinations: HPV and Hepatitis B vaccines reduce risks of cervical and liver cancers.
-
Regular Screenings: Mammograms, colonoscopies, and CT scans for high-risk individuals improve early detection.
-
Aftercare for SRT Patients:
-
Use of steroids or anti-seizure medications as supportive therapy.
-
Scheduled MRI scans to monitor tumor shrinkage or stability.
-
Psychological counseling and rehabilitation when needed.
-
Complications of SRT (Stereotactic Radiation Therapy)
Though considered safe, SRT has potential complications:
-
Acute Side Effects: Fatigue, mild swelling, headaches, nausea, localized skin irritation.
-
Delayed Complications: Radiation necrosis, memory decline, or hormonal imbalances if pituitary regions are irradiated.
-
Rare Risks: Development of secondary malignancies years after treatment.
Most patients experience minimal side effects, especially compared to conventional radiotherapy or invasive surgery.
Living with the Condition of SRT (Stereotactic Radiation Therapy)
Patients treated with SRT often experience improved survival and quality of life.
-
Recovery: Most return to normal activities within a day or two, unlike surgery, which may require weeks of recovery.
-
Follow-Up: Regular imaging helps track tumor response. Many patients see tumor shrinkage or stabilization within months.
-
Quality of Life Benefits:
-
Minimal pain and scarring.
-
Better preservation of neurological and organ functions.
-
Ability to maintain independence and daily routines.
-
Emotional support is also crucial. Patients benefit from connecting with cancer support groups, psychological therapy, and rehabilitation services tailored to cognitive or motor recovery.
Top 10 Frequently Asked Questions about Stereotactic Radiation Therapy (SRT)
1. What is Stereotactic Radiation Therapy (SRT)?
Stereotactic Radiation Therapy (SRT) is a highly precise form of radiation treatment used to target tumors or abnormal tissue in the body, often in the brain or spine. It delivers high doses of radiation to the affected area while minimizing exposure to surrounding healthy tissues.
2. How does SRT differ from conventional radiation therapy?
Unlike traditional radiation therapy, which targets larger areas over several weeks, SRT:
-
Uses advanced imaging for precise targeting
-
Delivers high-dose radiation in fewer sessions
-
Minimizes damage to surrounding healthy tissue
-
Often achieves faster results with fewer side effects
3. What conditions can SRT treat?
SRT is used to treat:
-
Brain tumors (both benign and malignant)
-
Metastatic cancer in the brain or spine
-
Arteriovenous malformations (AVMs)
-
Certain head and neck cancers
-
Other small, well-defined tumors in various parts of the body
4. Is SRT safe?
Yes, SRT is considered very safe when performed by experienced radiation oncologists. Its precision reduces the risk of damage to healthy tissue, making it suitable even for delicate areas like the brain or spinal cord. Careful planning and imaging are essential for safety.
5. What are the benefits of SRT?
Key benefits include:
-
High precision targeting of tumors
-
Shorter treatment duration (often 1-5 sessions)
-
Minimal damage to surrounding healthy tissue
-
Reduced side effects compared to conventional radiation
-
Outpatient procedure in many cases
6. Are there any side effects of SRT?
Side effects are usually mild and depend on the location treated. They may include:
-
Fatigue
-
Temporary hair loss at the treatment site (if on the scalp)
-
Mild skin irritation
-
Headaches or nausea (rare, usually temporary)
Long-term complications are uncommon due to the focused nature of the therapy.
7. How is SRT planned and delivered?
SRT involves:
-
Detailed imaging using CT, MRI, or PET scans
-
Creation of a 3D map of the tumor or target area
-
Precise calculation of radiation dose
-
Delivery using specialized equipment such as a linear accelerator (LINAC) or Gamma Knife
This ensures accurate targeting and protection of healthy tissue.
8. Who is a candidate for SRT?
Ideal candidates include patients with:
-
Small, well-defined tumors
-
Tumors in sensitive or hard-to-reach areas (like the brain or spine)
-
Patients seeking non-surgical treatment or who are not suitable for surgery
A radiation oncologist will evaluate tumor size, location, and overall health to determine eligibility.
9. How long does SRT treatment take?
SRT is usually delivered in 1 to 5 sessions, each lasting 30-90 minutes, depending on the size and location of the tumor. Most patients can go home the same day, making it a convenient outpatient procedure.
10. What is the success rate of SRT?
SRT has high success rates, particularly for small tumors and metastases. Tumor control rates are often above 80-90%, depending on the type of tumor and location. Its precision minimizes recurrence and reduces complications compared to traditional radiation therapy.


