Introduction to Total Anomalous Pulmonary Venous Return (TAPVR)
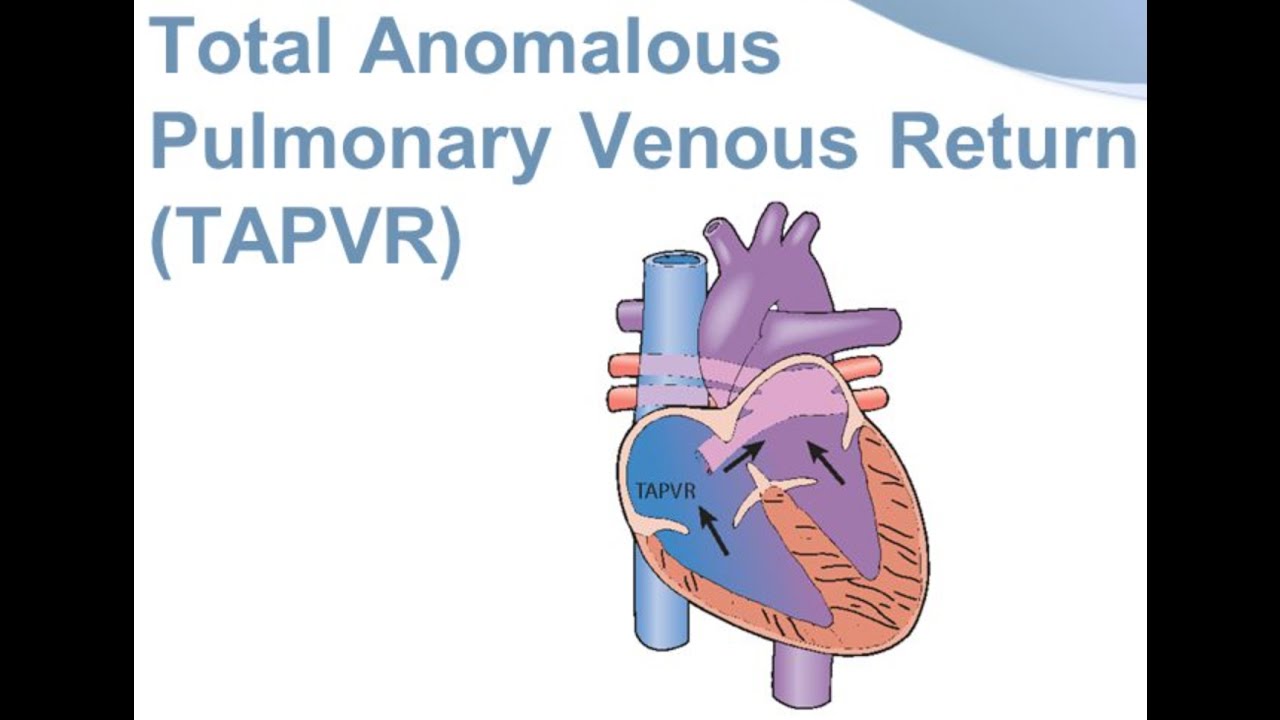
Total Anomalous Pulmonary Venous Return (TAPVR) is a rare congenital heart defect in which the pulmonary veins, which should return oxygen-rich blood from the lungs to the left atrium, instead connect abnormally to the right side of the heart or to systemic veins. This abnormal connection prevents oxygen-rich blood from entering the left atrium and thus reduces the amount of oxygen in the body.
TAPVR is a critical condition that usually manifests shortly after birth or early in the neonatal period. It is one of the most severe congenital heart diseases, with an incidence of approximately 1 in 10,000 live births. Due to the heart's inability to effectively deliver oxygenated blood, this condition can lead to serious complications such as cyanosis, respiratory distress, and heart failure if left untreated.
Types of TAPVR
TAPVR can be classified into four types based on the location where the pulmonary veins drain:
-
Supracardiac TAPVR: The pulmonary veins drain into the superior vena cava or innominate vein.
-
Cardiac TAPVR: The pulmonary veins drain into the coronary sinus or the right atrium.
-
Infracardiac TAPVR: The pulmonary veins drain into the inferior vena cava or the hepatic veins.
-
Mixed TAPVR: A combination of the above types, where the pulmonary veins drain into multiple systemic veins.
Each type of TAPVR leads to different anatomical and functional implications that influence how the condition is treated and managed.
Causes and Risk Factors of TAPVR
While the exact cause of TAPVR is not fully understood, research has identified several factors that increase the likelihood of this congenital defect.
Genetic Causes
TAPVR is often associated with genetic mutations and chromosomal abnormalities. For instance, it may occur in individuals with:
-
DiGeorge syndrome: A genetic condition caused by a deletion of a small part of chromosome 22. This syndrome often results in heart defects like TAPVR.
-
Williams syndrome: Another genetic condition that may be associated with heart defects, including TAPVR.
-
Chromosomal abnormalities: Other genetic mutations, including trisomy 21 (Down syndrome), can also increase the risk of TAPVR.
Environmental Factors
-
Maternal Health: Certain maternal factors, such as diabetes, viral infections, and exposure to teratogens (harmful substances), can influence the likelihood of developing TAPVR in the fetus. For example, maternal rubella during pregnancy has been linked to various heart defects, including TAPVR.
-
Medications: Certain medications taken during pregnancy, such as those used to treat epilepsy or autoimmune disorders, may increase the risk of congenital heart defects.
Family History
-
Hereditary Factors: Having a family history of congenital heart disease can increase the likelihood of developing TAPVR. Genetic counseling may be recommended for families with a history of heart defects.
Symptoms and Signs of TAPVR
The symptoms of TAPVR depend on the type and severity of the abnormality. In the neonatal period, symptoms are typically more severe and are noticeable shortly after birth. If untreated, the condition can lead to heart failure and other complications.
Common Symptoms in Newborns and Infants
-
Cyanosis (Blue Skin): One of the most noticeable signs of TAPVR is cyanosis, a bluish discoloration of the skin, lips, and nails caused by low oxygen levels in the blood.
-
Rapid Breathing: Infants may exhibit tachypnea (rapid breathing) and may struggle to breathe effectively.
-
Poor Feeding: Babies with TAPVR may have difficulty feeding, leading to poor weight gain and failure to thrive.
-
Fatigue and Weakness: Due to decreased oxygenation, affected infants often seem unusually lethargic or weak.
-
Swelling (Edema): Swelling in the legs, abdomen, or other parts of the body due to poor blood circulation.
-
Heart Murmur: A characteristic heart murmur is often detected upon physical examination, indicating abnormal blood flow in the heart.
Symptoms in Older Children and Adults
-
Fatigue: As children and adults with TAPVR grow, they may experience fatigue with physical exertion.
-
Shortness of Breath: Difficulty breathing, especially during physical activity or exertion, is common.
-
Chest Pain: Chest discomfort or pain may occur, especially in cases where the heart is under strain due to the abnormal blood flow.
-
Swelling: In some cases, persistent swelling in the legs or abdomen can occur.
-
Poor Physical Endurance: Individuals may have reduced stamina due to inefficient oxygen delivery to body tissues.
Diagnosis of TAPVR
Diagnosis of TAPVR is typically made through a combination of clinical evaluation, imaging studies, and sometimes cardiac catheterization. Early detection is critical to preventing complications like heart failure or pulmonary hypertension.
1. Clinical Examination
A healthcare provider will perform a physical examination to check for symptoms like cyanosis, a heart murmur, and signs of respiratory distress.
2. Imaging Techniques
-
Echocardiogram: The most commonly used diagnostic tool, an echocardiogram uses sound waves to create a visual image of the heart and blood flow. It can reveal abnormal connections of the pulmonary veins and the impact on heart function.
-
Chest X-ray: A chest X-ray can show signs of an enlarged heart or fluid buildup in the lungs (pulmonary edema).
-
Cardiac MRI and CT Scans: These provide detailed, high-resolution images that help visualize complex anatomical structures, including the abnormal veins in TAPVR.
-
Cardiac Catheterization: In some cases, doctors may use a catheter inserted into the heart to directly visualize the blood flow, pressure, and anatomy of the heart. This is usually reserved for more complicated cases.
Treatment Options for TAPVR
Treatment of TAPVR typically involves surgical intervention to correct the abnormal connections. The timing and type of surgery depend on the severity of the defect and whether there is any associated heart failure.
Surgical Repair
-
Timing of Surgery: Surgery is usually performed in the first few months of life, particularly if there is no obstruction to the blood flow. Early intervention is crucial to prevent complications such as pulmonary hypertension or heart failure.
-
Surgical Procedure: The pulmonary veins are rerouted into the left atrium, where they should normally drain. This is a complex surgery that requires careful planning and expert surgical techniques.
-
For Supracardiac TAPVR: The veins are rerouted to the left atrium, bypassing the superior vena cava.
-
For Cardiac TAPVR: The veins are redirected from the coronary sinus to the left atrium.
-
For Infracardiac TAPVR: The veins are connected to the left atrium through the appropriate venous system.
-
Postoperative Care
After surgery, the child will typically spend several days in the intensive care unit (ICU) for monitoring. Oxygen therapy and medications to manage heart function may be required. Once stabilized, the child can be transferred to a regular hospital room for further recovery.
Medical Management
-
Oxygen Therapy: To help maintain oxygen levels in the blood, especially during the recovery period.
-
Prostaglandin Therapy: Prostaglandins are sometimes used to keep certain blood vessels open until surgery is performed.
Prevention and Management of TAPVR
While TAPVR cannot be prevented, early detection and prompt treatment can significantly improve outcomes. Management after surgery typically includes long-term monitoring and lifestyle adjustments.
Prevention
-
Prenatal Care: Regular prenatal screenings and ultrasound examinations can help detect congenital heart defects early, allowing for timely intervention.
-
Genetic Counseling: Families with a history of congenital heart disease should consider genetic counseling to assess their risk for TAPVR and other conditions.
-
Maternal Health: Ensuring good maternal health, including controlling diabetes and avoiding infections during pregnancy, can reduce the risk of congenital heart defects.
Long-Term Management
-
Regular Follow-Ups: Lifelong follow-up with a pediatric cardiologist is necessary to monitor for late complications or recurrence of symptoms.
-
Physical Activity: Children recovering from TAPVR surgery should gradually resume normal physical activities, with the guidance of their healthcare provider.
-
Medications: Certain medications may be prescribed to help maintain normal heart function or manage complications such as arrhythmias.
Complications of TAPVR
TAPVR is a serious condition, and even after surgical treatment, there may be complications:
-
Pulmonary Hypertension: High blood pressure in the lungs can result from prolonged abnormal blood flow and can damage the heart and lungs.
-
Arrhythmias: Abnormal heart rhythms may develop, requiring treatment or interventions.
-
Residual Defects: In some cases, the surgery may not fully correct the abnormal venous return, leading to residual heart issues.
-
Heart Failure: Long-term effects of untreated or poorly managed TAPVR can lead to progressive heart failure.
Living with the Condition of Tapvr
For those who have undergone successful surgery, living with TAPVR requires ongoing care and management.
Emotional and Psychological Support
The diagnosis and treatment of TAPVR can be emotionally challenging for both children and their families. Support groups, therapy, and counseling can help families cope with the stress and uncertainty that come with congenital heart defects.
Physical Recovery
-
Rehabilitation: After surgery, physical therapy may be necessary to help regain strength, particularly for children who may have been restricted in their activities due to heart complications.
-
Long-Term Health: Although many children grow up to lead normal lives after treatment, regular cardiology follow-ups are critical for monitoring long-term health.
Top 10 Frequently Asked Questions about Total Anomalous Pulmonary Venous Return (TAPVR)
1. What is Total Anomalous Pulmonary Venous Return (TAPVR)?
TAPVR is a rare congenital heart defect where the pulmonary veins, which carry oxygen-rich blood from the lungs, do not connect to the left atrium as they should. Instead, they connect abnormally to the right side of the heart, leading to oxygen-poor blood being pumped into the body. This condition requires surgical intervention to correct the abnormal connections and restore normal blood flow.
2. What are the symptoms of TAPVR in newborns?
Symptoms often appear soon after birth and may include:
-
Bluish tint to the skin, lips, or nails (cyanosis)
-
Rapid or labored breathing
-
Poor feeding or lethargy
-
Weak pulse
-
Heart murmur
-
Enlarged liver
-
Cool, clammy skin
These signs indicate that the baby is not receiving enough oxygenated blood and require immediate medical attention.
3. How is TAPVR diagnosed?
Diagnosis typically involves:
-
Echocardiogram: An ultrasound of the heart to visualize the abnormal connections.
-
Chest X-ray: To check for heart enlargement or fluid in the lungs.
-
Electrocardiogram (ECG): To assess heart rhythm and electrical activity.
-
Cardiac catheterization: To measure pressures within the heart and obtain detailed images.
-
Cardiac MRI or CT scan: For detailed anatomical assessment in complex cases.
4. What are the different types of TAPVR?
TAPVR is classified based on where the pulmonary veins connect:
-
Supracardiac: Veins drain into the superior vena cava.
-
Infracardiac: Veins drain into the inferior vena cava or portal vein.
-
Cardiac: Veins drain directly into the right atrium or coronary sinus.
-
Mixed: A combination of the above types.
The type influences the surgical approach and complexity of the repair.
5. How is TAPVR treated?
Surgical correction is required for all cases of TAPVR. The procedure involves:
-
Connecting the pulmonary veins directly to the left atrium.
-
Closing any abnormal connections.
-
Repairing associated defects like atrial septal defects.
The timing of surgery depends on the severity of the condition and the infant's overall health. In critically ill newborns, surgery may be performed immediately after birth.
6. What is the prognosis after surgery for TAPVR?
With early surgical intervention, the prognosis is generally favorable. Most children recover well and lead normal lives. However, some may experience complications such as:
-
Narrowing of the pulmonary veins (requiring further procedures).
-
Arrhythmias (irregular heartbeats).
-
Need for additional surgeries later in life.
Regular follow-up with a pediatric cardiologist is essential to monitor heart health.
7. Can TAPVR be detected before birth?
Yes, TAPVR can often be detected during routine prenatal ultrasounds or through fetal echocardiography. Early detection allows for planning appropriate care immediately after birth.
8. What causes TAPVR?
The exact cause of TAPVR is not well understood. It occurs during fetal development when the pulmonary veins fail to connect properly to the left atrium. While most cases are isolated, TAPVR can sometimes be associated with other congenital heart defects or genetic conditions.
9. Is TAPVR hereditary?
TAPVR is typically not inherited. Most cases occur sporadically without a family history of congenital heart defects. However, in rare instances, it may be associated with genetic syndromes, and genetic counseling may be recommended for affected families.
10. What follow-up care is needed after TAPVR surgery?
Lifelong follow-up with a cardiologist is crucial. Monitoring may include:
-
Regular echocardiograms to assess heart function.
-
Electrocardiograms to detect arrhythmias.
-
Exercise stress tests as the child grows.
-
Monitoring for potential complications like vein narrowing or heart rhythm issues.
Early detection of any issues allows for timely intervention and optimal outcomes.


