Introduction to Tympanometry
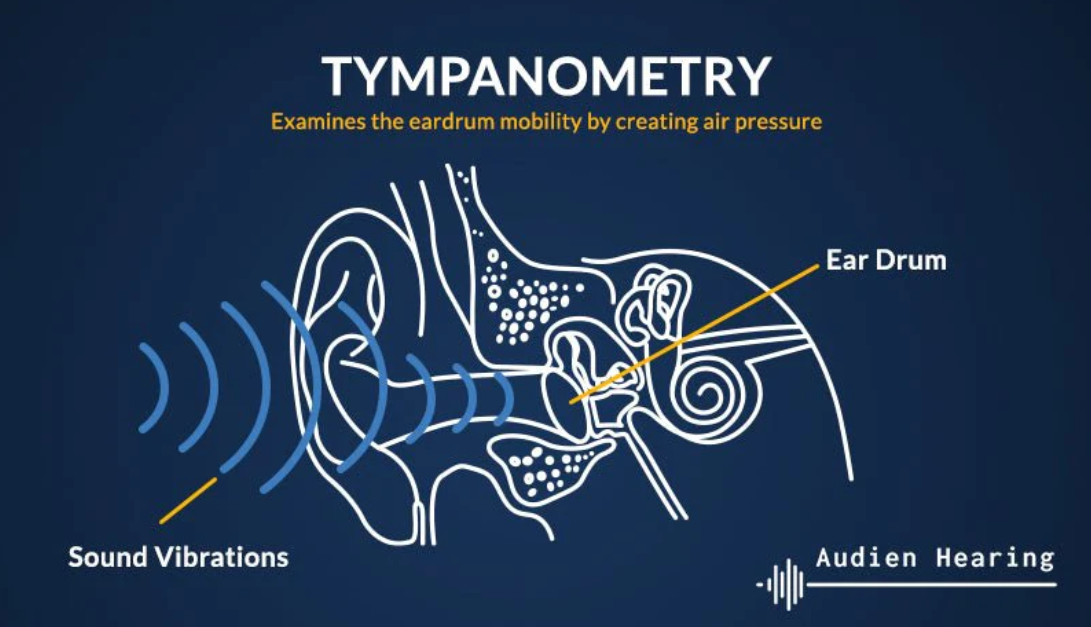
Tympanometry is a diagnostic test used to assess the function of the middle ear, including the eardrum (tympanic membrane), the auditory ossicles (small bones), and the Eustachian tube. It does not measure hearing thresholds (how well one hears), but rather how well sound is transmitted through the middle ear by measuring how the eardrum moves in response to changes in air pressure.
The test is commonly done in clinics of otolaryngologists (ENTs) or audiology departments. It is often used in children (especially when otitis media or middle ear effusion is suspected), but also in adults when there are signs of middle ear problems (e.g. hearing loss, ear fullness, tinnitus, or after ear infection).
Why is tympanometry useful?
-
It helps to differentiate between conductive hearing loss vs sensorineural loss, by identifying middle ear pathologies.
-
It guides treatment decisions, e.g., whether fluid behind the eardrum is present and persistent, whether Eustachian tube dysfunction is involved.
-
Monitoring progress: after treatment, tympanometry can be repeated to evaluate resolution or improvement.
Causes and Risk of Tympanometry
Since tympanometry is a diagnostic test, not a disease, this section refers to the circumstances that lead to needing the test, the conditions it detects, and any risk factors for abnormal findings.
Causes or Indications for Performing Tympanometry
Tympanometry is indicated when there is suspicion of middle ear dysfunction. Common conditions or causes include:
-
Otitis media with effusion (OME) — fluid accumulation behind the tympanic membrane without acute infection, e.g., in children after upper respiratory infections.
-
Acute otitis media (AOM) — may have fluid, eardrum bulging, pain, etc. Tympanometry helps assess presence of fluid and the mobility of the tympanic membrane.
-
Eustachian tube dysfunction — when the tube that equalizes pressure between middle ear and nasopharynx doesn't work properly (due to allergies, infections, congestion, etc.). This can cause negative pressure in middle ear, retraction of eardrum.
-
Perforation of tympanic membrane or previous surgery (tympanostomy tubes) — affects air pressure, volume measured by the test.
-
Scarring of the eardrum (tympanosclerosis) — past infections can stiffen or thicken the eardrum, altering compliance.
-
Earwax blockage (cerumen) — sometimes the canal occlusion can affect results or mimic pathology.
Risk Factors for Abnormal Findings
These are the factors or circumstances that increase the chance of having middle ear dysfunction (hence abnormal tympanometry). They are not risks of tympanometry but risks for what the test detects:
-
Young age, especially children under school-age, as they are more prone to middle ear infections and Eustachian tube immaturity.
-
Frequent upper respiratory tract infections, allergies, nasal congestion.
-
History of ear infections or otitis media.
-
Structural issues: cleft palate, chronic inflammation, any anatomical abnormality that affects the Eustachian tube.
-
Environmental factors: exposure to smoking, poor air quality.
-
Repeated exposure to water (swimming) or changes in altitude/pressure.
Risks of Performing Tympanometry
Tympanometry is very safe. There are no known significant adverse effects. Some minor discomforts may occur:
-
A feeling of pressure in the ear as air is pumped in or out.
-
A loud tone or sound that may be startling but not harmful.
-
In children, anxiety or movement during test may make it difficult or require repeats.
-
If there is an active infection or large perforation, results may be misleading. In some cases, testing may be postponed or modified.
Symptoms and Signs Related to Conditions Tympanometry Detects
Since tympanometry itself doesn't cause symptoms, this section rather describes what symptoms lead someone to get tympanometry and what signs are found in conditions identified by tympanometry.
Symptoms
People (or parents, in case of children) may notice:
-
Hearing loss or muffled hearing, especially one ear or both.
-
Ear fullness or feeling of pressure in the ear.
-
Ear pain or discomfort intermittently.
-
Ringing in the ear (tinnitus).
-
Delays in speech development (in young children) or difficulty understanding speech.
-
Recurrent ear infections.
Signs (on clinical examination)
-
On otoscopic exam: fluid behind the eardrum, bulging or retraction of the tympanic membrane.
-
Visible perforation or tube in tympanic membrane.
-
Discharge, redness, swelling if infection.
-
Abnormal movement of eardrum when tested via pneumatic otoscopy.
These symptoms & signs prompt the physician / audiologist to order tympanometry. After performing tympanometry you get objective signs via the tympanogram. The shapes/types of tympanogram indicate different conditions.
Diagnosis via Tympanometry
Here you detail how the test is done, what results mean.
Test Procedure
-
Pre-test preparation
-
Ensure ear canal is free of wax or obstruction. Otoscopy is done first.
-
In children, make sure they are calm, explain test etc.
-
-
Use of probe / selection of probe tone
-
A probe is placed inside ear canal; tip must seal well.
-
Tone used: standard adult probe tone often 226 Hz; in infants or younger children, higher frequency probe tones (e.g. 1000 Hz) or wideband stimuli for more reliable measures.
-
-
Varying air pressure
-
The device alternately increases and decreases air pressure in the ear canal, while measuring how the eardrum responds to sound under these pressure changes.
-
-
Recording results / Tympanogram
-
The result is graphed as a tympanogram: compliance / admittance (vertical axis) vs pressure (horizontal axis).
-
Also measured: ear canal volume, static compliance, peak pressure, gradient or width of the peak.
-
Additional Diagnostic Value
-
Tympanometry is often used together with pneumatic otoscopy to improve accuracy in detecting effusion or validating findings.
-
Used in screening infants or young children for hearing difficulties.
Treatment Options Relating to Conditions Found via Tympanometry
Since tympanometry is diagnostic and not therapeutic, “treatment options” refers to treatment of conditions revealed by abnormal tympanometry.
Depending on what the tympanogram shows, treatment (or management) will differ.
| Condition Detected | Typical Treatment / Management |
|---|---|
| Middle Ear Fluid / Otitis Media with Effusion (OME) | Often watch-and-wait for several months in children (since many resolve spontaneously), manage allergies, nasal hygiene; if persistent (>3 months) or affecting hearing/speech, may consider myringotomy (surgical drainage) with or without tympanostomy tubes. |
| Acute Otitis Media (AOM) | Antibiotic therapy (if indicated), analgesics; sometimes surgical intervention if severe or recurrent. Tympanometry helps confirm presence of fluid. |
| Eustachian Tube Dysfunction | Treat underlying cause (allergies, infections, nasal congestion), decongestants, nasal steroids, autoinflation maneuvers; in chronic cases surgical options (balloon dilation of Eustachian tube) may be considered. |
| Tympanic Membrane Perforation or Tympanostomy Tubes | Evaluate need for surgical repair (tympanoplasty), keep ear dry to prevent infection, monitor; tubes may aid ventilation. |
| Ossicular Chain Problems / Otosclerosis | Depending on severity: surgical intervention (ossiculoplasty, stapedectomy), hearing aids if surgery not possible. |
Also, after treatment, repeating tympanometry helps to monitor whether middle ear function is improving.
Prevention and Management Related to Tympanometry Findings
Again, since tympanometry is diagnostic, "prevention & management" refers to preventing or managing the middle ear conditions that are revealed.
Prevention
-
Manage upper respiratory infections early; avoid frequent colds.
-
Allergies: control with medications (antihistamines, nasal corticosteroids) to reduce nasal congestion and Eustachian tube swelling.
-
Avoid exposure to irritants like tobacco smoke.
-
Keep ears dry; prevent water entry if there is perforation or tubes.
-
Vaccinations: pneumococcal vaccine, influenza vaccine may reduce risk of otitis media.
-
Encourage good hygiene, hand-washing, avoid close contact in outbreaks.
Management
-
In mild cases or in children, “watchful waiting” with regular monitoring, including repeated tympanometry.
-
Use of decongestants, nasal sprays, autoinflation (e.g. Valsalva, nasal balloon devices) when indicated.
-
Hearing support / audiologic monitoring if hearing loss is present: speech therapy if in children.
-
Surgical interventions when conservative methods don't work: placement of ventilation tubes, myringotomy, tympanoplasty etc.
-
Patient education: what abnormal tympanogram means, what to expect.
Complications of Conditions Diagnosed by Tympanometry
Tympanometry itself has no significant complications, but the underlying middle ear conditions (if untreated or poorly managed) can lead to problems.
Possible Complications
-
Hearing loss: temporary or, in severe/chronic cases, permanent (especially in children, impacts speech/language development).
-
Speech and language delays in young children.
-
Chronic otitis media: repeated infections, possible damage to middle ear structures.
-
Tympanic membrane damage: long-standing negative pressure, perforation, scarring (tympanosclerosis).
-
Balance issues, tinnitus.
-
Spread of infection: in rare cases, to mastoid air cells or beyond.
Living with Conditions Detected by Tympanometry
How patients (or parents of pediatric patients) can cope, what lifestyle adjustments might help, what follow-ups are needed.
Daily Life Adjustments
-
If hearing is affected, consider assistive listening devices.
-
Reduce exposure to loud noise; protect ears.
-
Maintain nose and throat health (treat allergies, avoid irritants).
-
Keep ears dry, especially if perforated membrane or tubes present.
Monitoring & Follow-Up
-
Regular checkups with ENT / audiologist.
-
Repeat tympanometry to track improvements or worsening.
-
Audiometry as needed to assess hearing thresholds.
Special Considerations for Children
-
Monitoring speech development.
-
Ensuring classroom and learning environments support hearing (e.g. prefer front seating, minimize background noise).
-
Parent education: how to do autoinflation, recognizing signs of ear infection.
Emotional & Quality of Life
-
Hearing loss and ear problems can frustrate social interaction, school, work. Counseling or support groups may help.
-
For persistent conditions, surgical options may be emotionally and physically taxing; proper counselling and information is important.
Top 10 Frequently Asked Questions about Tympanometry
1. What is tympanometry?
Tympanometry is a quick, non-invasive diagnostic test that evaluates how well the middle ear and eardrum (tympanic membrane) are functioning. It measures the movement of the eardrum in response to changes in air pressure and sound, helping doctors detect issues like fluid in the middle ear, ear infections, eardrum perforations, or Eustachian tube dysfunction.
2. Why is tympanometry performed?
Doctors recommend tympanometry for several reasons:
-
To check for middle ear infections (otitis media).
-
To detect fluid buildup behind the eardrum.
-
To evaluate blockage of the Eustachian tube.
-
To assess eardrum perforations or scarring.
-
To confirm the presence and function of ear ventilation tubes.
It is an essential test when patients complain of hearing loss, ear pain, or a feeling of fullness in the ear.
3. How is tympanometry performed?
During the test:
-
A soft probe is gently inserted into the ear canal.
-
The probe changes air pressure inside the canal while delivering a series of tones.
-
The machine records how the eardrum responds to these changes.
The test is painless, takes only a few minutes per ear, and can be done in both children and adults.
4. Does tympanometry hurt?
No, tympanometry is not painful. Patients may feel a slight pressure change or mild discomfort in the ear, similar to what is experienced during altitude changes (like in an airplane). The test is safe and well-tolerated, even for young children.
5. What conditions can tympanometry detect?
Tympanometry is useful in diagnosing conditions such as:
-
Otitis media with effusion (fluid in the middle ear)
-
Acute or chronic ear infections
-
Perforated or scarred eardrum
-
Eustachian tube dysfunction
-
Otosclerosis (stiffening of middle ear bones)
-
Problems with ear ventilation tubes
6. Can tympanometry detect hearing loss?
Not directly. Tympanometry does not measure hearing ability but rather the mobility of the eardrum and middle ear system. However, when combined with hearing tests (audiometry), it helps doctors determine whether hearing loss is due to middle ear problems or issues with the inner ear/auditory nerve.
7. How are tympanometry results interpreted?
Results are displayed as a tympanogram (graph) showing eardrum movement:
-
Type A: Normal middle ear function.
-
Type B: Flat graph, indicating fluid behind the eardrum, perforation, or blockage.
-
Type C: Negative pressure, suggesting Eustachian tube dysfunction.
These results guide doctors in choosing the right treatment, such as antibiotics, ear tubes, or surgery.
8. Who should undergo tympanometry?
Tympanometry is commonly recommended for:
-
Children with recurrent ear infections or hearing problems.
-
Adults with chronic ear pain, pressure, or fullness.
-
Patients with sudden hearing loss.
-
Individuals being monitored after ear surgery or ear tube placement.
9. Are there any risks or side effects of tympanometry?
Tympanometry is a very safe test. Rarely, patients may feel brief dizziness or discomfort due to pressure changes, but there are no long-term risks. It is safe for children, adults, and even infants.
10. How should I prepare for tympanometry?
Preparation is simple:
-
Keep ears clean and free of wax (excessive earwax can affect results).
-
Avoid moving, talking, or swallowing during the test, as it can interfere with accuracy.
-
Inform the doctor if you have had recent ear surgery, severe ear pain, or drainage, as the test may need to be adjusted.


