Introduction to Vasectomy Reversal
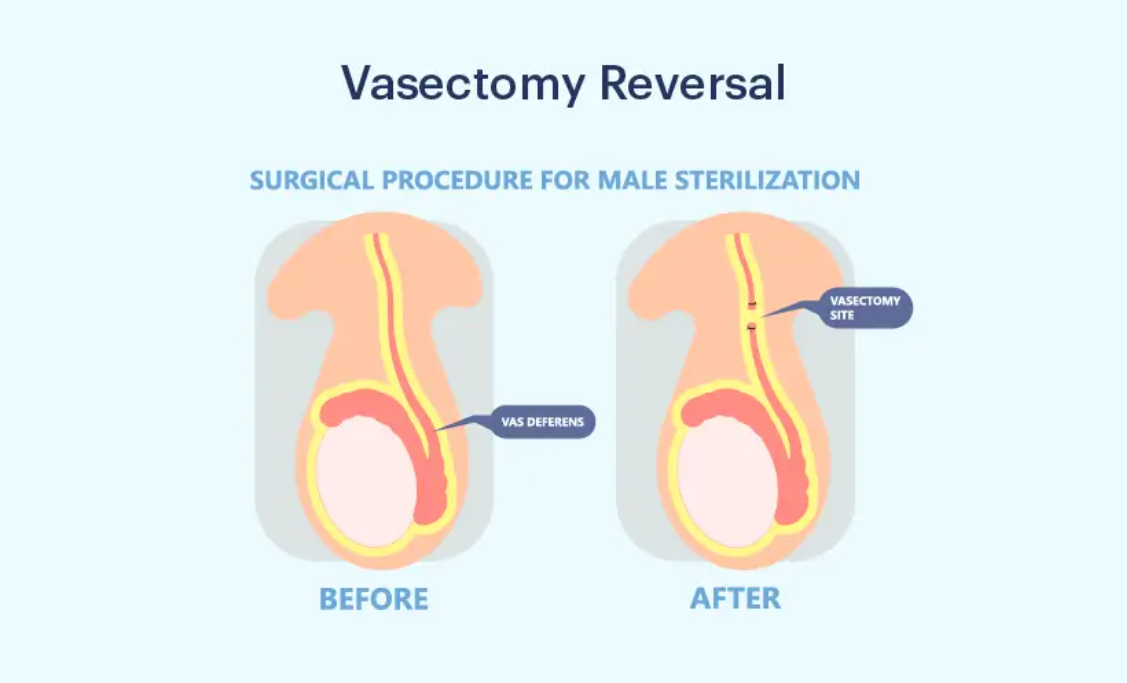
Vasectomy reversal is a surgical procedure designed to restore a man's ability to father children after a vasectomy, a permanent method of male contraception. During a vasectomy, the vas deferens, the tubes that carry sperm from the testicles to the urethra, are cut or sealed. However, for various reasons—such as changes in family planning, remarriage, or a desire for more children—some men may choose to reverse the procedure.
The reversal surgery involves reconnecting the severed ends of the vas deferens to allow sperm to travel from the testicles to the urethra again. There are two primary types of vasectomy reversal procedures:
-
Vasovasostomy: This is the most common technique, where the two ends of the vas deferens are directly reconnected.
-
Vesiculovasostomy: This procedure is used if there is a blockage at the site of the vas deferens near the seminal vesicle. In this case, the vas deferens is connected to the seminal vesicle to restore sperm flow.
The procedure is typically done under general anesthesia and may require a few hours, depending on the complexity. While vasectomy reversal is effective in many cases, the success rate depends on various factors such as the time elapsed since the original vasectomy, the presence of any scarring or damage, and the overall health of the reproductive system.
For many men, vasectomy reversal offers a chance to restore fertility and expand their family. However, the procedure may not always be successful, and sperm quality or other factors could still impact conception. Couples considering this option should consult with a urologist or fertility specialist to fully understand the potential risks, success rates, and available alternatives.
Causes and Risk of Vasectomy Reversal
Vasectomy reversal is a surgical procedure used to restore fertility in men who have previously undergone a vasectomy, a form of permanent contraception. During the procedure, the blocked or severed vas deferens are reconnected to allow sperm to again travel from the testicles to the semen. Though the procedure is considered relatively safe, it comes with specific causes for seeking it and associated risks that should be considered before proceeding.
Why Choose a Vasectomy Reversal?
-
Change in Family Circumstances: For men who initially chose vasectomy due to family planning but later seek to have children with a new partner.
-
Regret Over Permanent Contraception: The desire for more children after realizing vasectomy was too permanent a decision.
-
Healthier Relationship: The partner may not have children, creating a wish for biological offspring.
Risk Factors for Reversal Success
The effectiveness of a vasectomy reversal depends on several biological, anatomical, and lifestyle factors:
1. Time Since Vasectomy
-
Ideal Window: Reversals done within 3-7 years of the original vasectomy have the highest success rates. Beyond 10 years, the chance of successful sperm return reduces significantly, as scar tissue develops.
2. Type of Vasectomy
-
The technique used in the original vasectomy can affect reversal success. If the vas deferens was cauterized or sealed with heat, it may make reconnection more challenging compared to a traditional incision.
3. Age of the Man
-
Younger men (under 40) tend to have better sperm production and motility, increasing the chances of a successful reversal. The quality of sperm also declines with age, making reversals slightly more difficult for older men.
4. Female Partner's Fertility
-
The age and fertility of the female partner significantly impact the chances of conception after a successful vasectomy reversal.
5. Presence of Anti-Sperm Antibodies
-
Some men develop anti-sperm antibodies following a vasectomy, which may hinder sperm motility, making conception more difficult.
6. Overall Health of the Patient
-
Chronic conditions such as diabetes, obesity, and varicoceles may affect sperm production and quality, influencing the outcome of the reversal.
Symptoms and Signs of Vasectomy Reversal
Vasectomy reversal is a surgical procedure aimed at restoring fertility in men who have previously undergone a vasectomy. While it can be successful, there are specific symptoms and signs that men may experience after the procedure, which can vary depending on the individual and the complexity of the surgery.
After a vasectomy reversal, patients should watch for the following symptoms:
Post-Surgical Symptoms
-
Mild pain or discomfort around the incision sites, typically alleviated with over-the-counter pain relievers.
-
Swelling or bruising around the scrotum and the surgical site, which generally resolves in a few days.
-
Temporary changes in voice or hoarseness due to nerve involvement during surgery.
-
Fluid discharge from the surgical wound (usually mild and temporary).
Signs of Reversal Success
-
Return of sperm: The most significant indicator of success is the return of sperm in the semen. This is typically evaluated 3-6 months after the surgery.
-
Healthy sperm count and motility: After the reversal, sperm quality improves over time. Regular semen analysis will track sperm concentration, motility, and morphology.
Signs of Failure
-
Absence of sperm in semen post-surgery, indicating a failed procedure.
-
Persistent symptoms of pain or infection that do not resolve after initial healing.
Diagnosis of Vasectomy Reversal
Diagnosing the success of a vasectomy reversal involves evaluating the patient’s recovery, monitoring fertility, and confirming the restoration of sperm flow. The diagnosis process is multifaceted and involves clinical assessments, laboratory tests, and follow-up procedures. Below are the primary steps and diagnostic tools used to assess the success of a vasectomy reversal:
Pre-Surgical Diagnostic Evaluation
Before undergoing a vasectomy reversal, men undergo a thorough diagnostic workup:
1. Medical History
-
The surgeon reviews the patient's health, history of the vasectomy, and previous fertility issues.
2. Physical Examination
-
The surgeon assesses the scrotum, testicles, and vas deferens for any abnormalities or conditions such as varicoceles or epididymal cysts that could affect the reversal.
3. Semen Analysis
-
Pre-operative semen analysis is conducted to check sperm motility and concentration. If sperm is absent, it helps in assessing the potential cause of infertility, which could be crucial in deciding the appropriate treatment.
4. Ultrasound Imaging
-
An ultrasound of the scrotum helps rule out other factors such as hydrocele or varicocele that might impact fertility.
Treatment Options of Vasectomy Reversal
Vasectomy reversal is a surgical procedure aimed at restoring fertility by reconnecting the vas deferens, the tubes that carry sperm from the testes to the urethra. When considering treatment options for vasectomy reversal, there are several factors, including the time since the vasectomy, the age and fertility of both partners, and the health of the reproductive system. Below are the main treatment options for vasectomy reversal:
1. Microsurgical Vasovasostomy (VV)
The most commonly used method for vasectomy reversal. It involves:
-
Reconnecting the cut ends of the vas deferens to restore the flow of sperm into the seminal fluid.
-
Performed under a microscope for precision, microsurgical vasovasostomy offers high success rates when the vasectomy was done within 10 years.
-
The procedure is done through small incisions on the scrotum, which allows for quicker recovery.
Success Rate:
-
90% or higher for men with a vasectomy performed less than 10 years ago.
2. Microsurgical Vasoepididymostomy (VE)
Used when there is a blockage at the epididymis or if a vasectomy has been in place for more than 10 years.
-
The vas deferens is attached directly to the epididymis, bypassing the blockage in the vas deferens.
-
This technique is more complex and involves a lower success rate than VV.
Success Rate:
-
50-70%, depending on individual factors.
3. Sperm Retrieval (PESA/ICSI)
When vasectomy reversal is not an option, sperm can be retrieved directly from the epididymis or testicles using PESA (Percutaneous Epididymal Sperm Aspiration) or TESA (Testicular Sperm Aspiration).
-
These sperm can then be used for in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
Prevention and Management of Vasectomy Reversal
Vasectomy reversal is a surgical procedure intended to restore fertility in men who have previously undergone a vasectomy. While the success of vasectomy reversal depends on factors such as the time since the vasectomy and the method used for the reversal, there are several strategies to prevent complications and manage recovery effectively.
Pre-Surgery Considerations
-
Counseling: It's crucial for men to discuss the expectations and realistic outcomes of the reversal with their healthcare provider.
-
Partner Involvement: Female partners should be informed about the reversal process, and it's important to evaluate their fertility as well.
-
Physical Health: Maintaining overall health (avoiding smoking, maintaining a healthy weight) can improve the chances of success.
Post-Surgery Management
-
Pain Management: Over-the-counter pain relief and ice packs for swelling.
-
Recovery: Avoid heavy lifting and physical activity for 3-4 weeks after surgery.
-
Follow-up: Regular semen analysis to monitor sperm return. Most men see sperm in their semen within 3 months.
Complications of Vasectomy Reversal
Vasectomy reversal, a surgical procedure to restore fertility in men who have previously undergone a vasectomy, can offer the possibility of regaining the ability to father children. However, like any surgical procedure, it carries certain risks and potential complications. Below are the common complications associated with vasectomy reversal:
Immediate Post-Surgical Complications
-
Infection: Rare, but may require antibiotics.
-
Bleeding (Hematoma): Swelling from blood collection; usually resolves with rest.
-
Scrotal Pain: Temporary but may persist for a few weeks.
-
Epididymal Hypertension: Painful condition if sperm builds up in the epididymis due to poor drainage.
Long-Term Complications
-
Scar Tissue: Scar formation in the vas deferens may reblock sperm flow.
-
Antisperm Antibodies: Some men develop antibodies to their own sperm, which can affect fertility.
-
Recurrence: If the reversal fails, a second surgery or sperm retrieval options may be needed.
Living with the Condition of Vasectomy Reversal
Living with the condition after a vasectomy reversal can be an emotional and physical journey. While the procedure itself aims to restore fertility by reconnecting the vas deferens, the post-surgery experience can vary depending on individual health, the success of the procedure, and emotional adjustments. Here’s a breakdown of what living with the condition of vasectomy reversal might entail:
Daily Living Post-Reversal
-
Sperm Monitoring: Periodic semen analysis to monitor sperm quality and motility.
-
Conception Planning: Understanding that even with successful sperm return, conception may take time due to age or fertility factors of both partners.
Emotional Aspects
-
Stress and Anxiety: The pressure of wanting a child may cause emotional strain, particularly if conception doesn't occur quickly. Counseling and support groups can help.
Long-Term Outlook
-
Most men experience significant improvement in fertility, with 50-60% of couples achieving pregnancy within 1-2 years of surgery.
-
It's important to maintain realistic expectations, as multiple factors impact pregnancy success.
Top 10 Frequently Asked Questions about Vasectomy Reversal
1. What is a vasectomy reversal?
A vasectomy reversal is a surgical procedure that aims to restore fertility in men who have previously undergone a vasectomy. During the procedure, the surgeon reconnects the vas deferens, the tubes that carry sperm from the testicles to the urethra, which were cut or sealed during the original vasectomy. This allows sperm to re-enter the semen, potentially leading to pregnancy.
2. Why would someone undergo a vasectomy reversal?
Men typically seek vasectomy reversal when:
-
They regret their vasectomy and wish to have children with a new partner or their current partner.
-
They want to restore fertility after a change in family planning goals.
-
They have experienced the death or infertility of a partner and wish to start a family with a new partner.
Vasectomy reversal is often considered by men who have healthy sperm and no other fertility issues.
3. What are the different types of vasectomy reversal procedures?
There are two main types of vasectomy reversal procedures:
-
Vasovasostomy: This is the most common type of reversal, where the ends of the vas deferens are reconnected directly.
-
Vasoepididymostomy: This procedure is done when there is a blockage near the epididymis (the organ that stores sperm). It involves connecting the vas deferens directly to the epididymis.
The choice of procedure depends on the blockage location and the surgeon's evaluation.
4. What is the success rate of vasectomy reversal?
Success rates depend on various factors, such as:
-
Time since vasectomy: The chances of success are higher if the vasectomy was done less than 10 years ago. After 15 years or more, success rates may decrease.
-
Age of the man and his partner: Younger men and partners tend to have higher success rates.
-
Surgical technique: The skill of the surgeon plays a crucial role in the success of the procedure.
Overall, 30-70% of men who undergo vasectomy reversal are able to father a child, with higher success rates for those who have had the procedure within 10 years of their vasectomy.
5. How is vasectomy reversal performed?
The procedure is usually done under general or local anesthesia:
-
The surgeon makes small incisions in the scrotum to access the vas deferens.
-
The blocked or cut ends of the vas deferens are identified and then carefully reconnected or bypassed (depending on the procedure).
-
The incision is closed with dissolvable stitches.
Vasectomy reversal typically takes 2-4 hours, and most men can go home the same day.
6. How long does recovery take after vasectomy reversal?
After surgery, patients can generally expect:
-
Rest for the first few days: Avoiding strenuous activity for about 2 weeks is advised.
-
Pain management: Mild to moderate pain can be managed with over-the-counter medications or prescribed pain relievers.
-
Follow-up care: A follow-up appointment is usually scheduled within 2-3 weeks to monitor healing.
While most men can return to work within 1-2 weeks, they should avoid heavy lifting or intense exercise for 4-6 weeks.
7. Is there any risk of complications with vasectomy reversal?
As with any surgery, there are some risks, including:
-
Infection at the incision site
-
Bleeding or hematoma
-
Sperm antibodies: Some men develop antibodies to their own sperm, which can interfere with fertility.
-
Failure to restore fertility: In some cases, even after a successful surgical procedure, natural conception may not occur.
However, serious complications are rare when the procedure is performed by an experienced surgeon.
8. How soon after the reversal can I expect to see results?
-
Sperm count: After the procedure, sperm may take 3-6 months to appear in the semen, and the sperm count may gradually increase.
-
Pregnancy: It may take up to a year for pregnancy to occur naturally after vasectomy reversal. Some couples may need intrauterine insemination (IUI) or in vitro fertilization (IVF) if natural conception does not happen.
9. Does a vasectomy reversal guarantee that I will be able to father a child?
While vasectomy reversal can restore fertility in many men, it does not guarantee that pregnancy will occur. Several factors affect fertility, such as:
-
Quality of sperm
-
Partner's fertility
-
The woman's age and fertility health
If pregnancy does not occur naturally, assisted reproductive techniques (ART) such as IUI or IVF can be considered.
10. What are the costs associated with vasectomy reversal?
The cost of vasectomy reversal can vary significantly depending on:
-
The surgeon's experience
-
The geographic location of the procedure
-
Additional costs such as anesthesia, surgical facility fees, and follow-up visits
On average, the cost ranges from $5,000 to $15,000. Insurance coverage may not always include vasectomy reversal, but some may cover fertility treatments if assisted reproduction is needed after the reversal.


