Introduction to Vesicovaginal Fistula
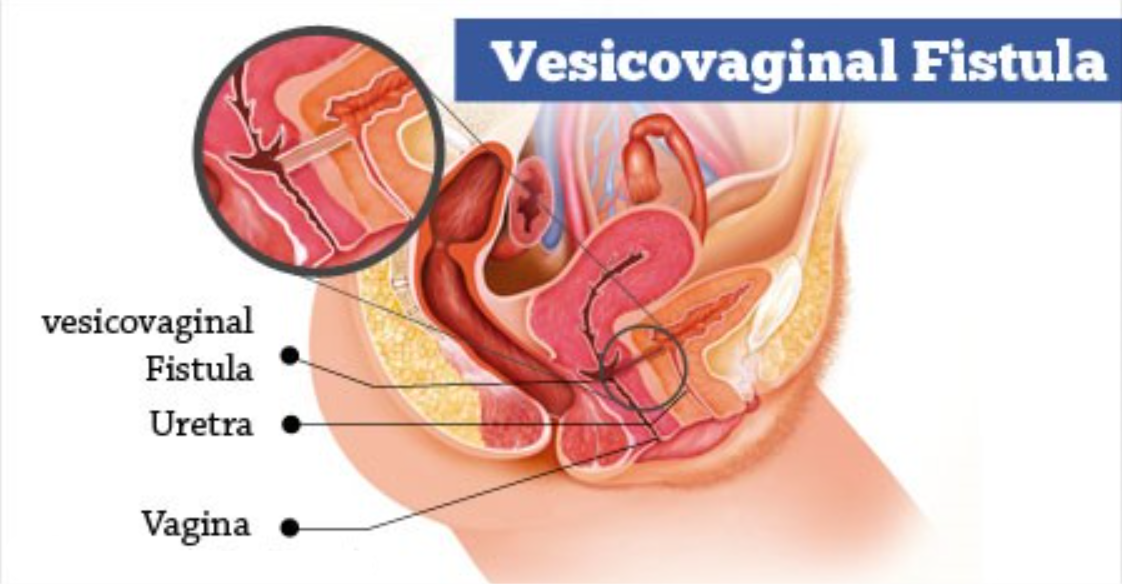
A Vesicovaginal fistula (VVF) is a medical condition where an abnormal connection forms between the bladder and the vagina, causing urine to leak uncontrollably from the bladder into the vaginal canal. This condition is often the result of childbirth, particularly prolonged or complicated labor, but it can also occur due to surgical complications, radiation therapy, pelvic infections, or trauma.
VVF leads to symptoms such as continuous urinary incontinence, vaginal odor, and skin irritation. Women with this condition may experience a significant loss of self-esteem and emotional distress due to the embarrassment and physical discomfort associated with involuntary urine leakage. The condition can also be associated with recurrent urinary tract infections (UTIs) and can affect a woman's sexual health and overall quality of life.
The diagnosis of VVF is made through a combination of clinical examination, imaging (such as cystoscopy), and contrast studies to confirm the presence and extent of the fistula.
Treatment of vesicovaginal fistula usually involves surgical repair, which aims to close the abnormal connection between the bladder and vagina. In most cases, surgical intervention has a high success rate, although the complexity of the repair depends on factors such as the size and location of the fistula, the cause, and the overall health of the patient. In some cases, patients may also require post-operative care, including the use of catheters or physiotherapy to restore bladder control.
VVF, while often debilitating, is a treatable condition, and early intervention can help restore normal bladder function and improve the affected woman's quality of life.
Causes and Risk Factors of Vesicovaginal Fistula
VVF can occur due to several causes, each impacting the quality of life for the affected individual. While obstetric complications remain the leading cause in low-resource countries, other medical conditions and surgeries can also contribute.
1. Obstetric Causes
-
Prolonged or Obstructed Labor:
The leading cause of VVF in developing countries. The constant pressure of the baby's head against the mother's pelvic region causes ischemia and subsequent necrosis in the vaginal and bladder walls, leading to the formation of a fistula.-
Obstetric fistula is often a complication of neglected obstructed labor, where skilled medical intervention, such as a cesarean section, was not available.
-
-
Instrumental Deliveries:
-
Forceps or vacuum-assisted deliveries may also lead to trauma in the vaginal or bladder wall, causing fistulas.
-
-
Perineal Tears:
Severe perineal tears during childbirth, if improperly repaired, can create pathways for urine to leak from the bladder to the vagina.
2. Iatrogenic Causes (Surgical Causes)
-
Pelvic Surgeries:
-
Hysterectomy, bladder surgeries, or surgeries to treat pelvic endometriosis can damage the vaginal wall or bladder, leading to VVF.
-
Cesarean Sections performed incorrectly or with poor technique may increase the risk of fistula formation.
-
-
Radiation Therapy:
-
Pelvic radiotherapy for cancers such as cervical or rectal cancer can damage the tissues, leading to fistula formation. This form of fistula is typically referred to as radiation-induced fistula.
-
3. Infectious and Inflammatory Causes
-
Chronic Infections:
-
Chronic urinary tract infections (UTIs), pelvic inflammatory disease (PID), or tuberculosis in the pelvic organs can lead to tissue destruction, which may result in a fistula.
-
HIV/AIDS: Immunocompromised patients have a higher risk of developing infections that weaken tissues and contribute to fistula formation.
-
4. Traumatic Causes
-
Pelvic Injuries:
-
Accidents, falls, or physical trauma to the pelvic area can damage the bladder or vagina, creating an abnormal connection between the two.
-
-
Surgical Complications:
-
Incorrect procedures during gynecological surgeries or abdominal surgery can lead to unintended fistula formation.
-
Symptoms and Signs of Vesicovaginal Fistula
The symptoms of vesicovaginal fistula can vary based on the size, location, and complexity of the fistula. The primary symptom is continuous urinary leakage, which can occur with minimal activity and significantly impact the individual's daily life.
Primary Symptoms:
-
Urinary Incontinence:
-
Continuous leakage of urine from the vagina, particularly when standing, coughing, or laughing.
-
Leakage can be moderate to severe, and it may occur regardless of the bladder's fullness.
-
-
Foul-Smelling Vaginal Discharge:
-
Due to the continuous presence of urine in the vaginal canal, odor becomes a persistent issue, leading to vaginal irritation and possible skin breakdown.
-
-
Recurrent Urinary Tract Infections (UTIs):
-
Chronic leakage increases the risk of UTIs, which may be recurrent and difficult to treat.
-
Secondary Symptoms:
-
Pain during Intercourse:
-
Dyspareunia (painful intercourse) occurs as a result of the abnormal opening between the vagina and bladder.
-
-
Pelvic Pain:
-
Chronic pelvic discomfort is common in some individuals with VVF, especially if the fistula has been present for a long period.
-
-
Skin Breakdown:
-
Constant exposure to urine can cause skin irritation, sores, and ulcers around the vaginal and perineal regions.
-
Diagnosis of Vesicovaginal Fistula
Proper diagnosis of VVF is critical to determining the best course of treatment. Various diagnostic methods can be used to identify and assess the fistula.
1. Clinical Evaluation
-
Medical History: A thorough history including obstetric history, surgical interventions, and any previous treatments.
-
Physical Examination: Inspection of the vaginal canal to look for visible signs of urinary leakage and skin irritation.
2. Diagnostic Imaging
-
Dye Test (Cystoscopy or Vaginoscopy):
-
Methylene blue or indigo carmine is introduced into the bladder to check for leakage into the vagina.
-
-
Ultrasound:
-
Transvaginal ultrasound is often the first imaging technique used to detect the location and size of the fistula.
-
-
CT/MRI:
-
Pelvic MRI or CT scan may be required for complex fistulas to assess adjacent structures and plan surgery.
-
-
Cystography:
-
A contrast X-ray used to assess the bladder's integrity and define the location of the fistula.
-
Treatment Options for Vesicovaginal Fistula
The treatment of VVF primarily involves surgical intervention, although some conservative management approaches can be used for minor cases.
1. Conservative Management
For small fistulas or newly diagnosed cases:
-
Urinary Diversion: A catheter may be used to divert urine away from the fistula site and allow healing.
-
Antibiotics: To treat any infections that might complicate the condition.
2. Surgical Repair
Surgical treatment is necessary for larger or more complex fistulas:
-
Transvaginal Repair:
-
The most common procedure for anterior fistulas. Involves cutting away damaged tissue, closing the fistula, and reinforcing the repair site using tissue from the labia or perineum.
-
-
Transabdominal Repair:
-
Used for posterior fistulas (closer to the cervix), this approach involves accessing the pelvic organs through an abdominal incision.
-
-
Laparoscopic/Robotic-Assisted Surgery:
-
Minimally invasive techniques that reduce recovery time and post-operative complications, especially for complicated fistulas.
-
-
Tissue Interposition Flaps:
-
Techniques like the Martius flap (labial tissue) are used to reinforce the fistula repair.
-
3. Post-Surgical Care
-
Bladder Drainage: A catheter is placed for 2-3 weeks after surgery to reduce pressure and promote healing.
-
Pain Management: Analgesics and anti-inflammatory medications for post-operative pain.
-
Antibiotics: To reduce the risk of post-operative infection.
Prevention and Management of Vesicovaginal Fistula
Prevention Strategies
-
Antenatal Care:
-
Proper prenatal care can help detect and prevent
obstructed labor and identify high-risk
pregnancies early.
-
Skilled Birth Attendants:
-
Ensuring that births are managed by skilled
professionals to prevent prolonged labor or
unnecessary instrumental deliveries.
-
Post-Operative Care:
-
Proper surgical techniques and post-operative management can
reduce the risk of VVF after pelvic surgeries.
Long-Term Management
-
Monitoring and Follow-Up: Regular check-ups to ensure
successful healing and to monitor for any recurrence of the fistula.
-
Psychosocial Support: Addressing the mental
health impacts of living with VVF and supporting patients
in adjusting to life post-surgery.
Antenatal Care:
-
Proper prenatal care can help detect and prevent obstructed labor and identify high-risk pregnancies early.
Skilled Birth Attendants:
-
Ensuring that births are managed by skilled professionals to prevent prolonged labor or unnecessary instrumental deliveries.
Post-Operative Care:
-
Proper surgical techniques and post-operative management can reduce the risk of VVF after pelvic surgeries.
-
Monitoring and Follow-Up: Regular check-ups to ensure successful healing and to monitor for any recurrence of the fistula.
-
Psychosocial Support: Addressing the mental health impacts of living with VVF and supporting patients in adjusting to life post-surgery.
Complications of Vesicovaginal Fistula
If untreated or improperly managed, VVF can lead to several complications:
-
Chronic Urinary Incontinence: Persistent leakage of urine.
-
Renal Damage: Recurring infections can lead to kidney damage.
-
Skin Breakdown and Infection: Prolonged exposure to urine can lead to painful ulcers and infections in the vaginal and perineal region.
-
Social Stigma and Isolation: Individuals with VVF may experience psychological distress due to the stigma of involuntary urination.
Living with Vesicovaginal Fistula
Emotional and Psychosocial Impact
Living with VVF can have profound emotional effects, including:
-
Shame and Embarrassment: Patients often feel socially
isolated due to the continuous leakage of urine.
-
Depression and Anxiety: The emotional
toll of living with VVF can lead to mental health issues,
especially in communities where the condition is stigmatized.
Physical Adjustments
-
Absorbent Pads: Continual use of pads
or adult diapers to manage urine leakage.
-
Pelvic Floor Exercises: Some individuals benefit from
strengthening pelvic muscles to regain some control over urination.
Long-Term Outlook
-
Successful Surgery: After surgical intervention, most
individuals can return to normal life, free from leakage.
Rehabilitation and psychosocial
support are key to maintaining long-term well-being.
Shame and Embarrassment: Patients often feel socially isolated due to the continuous leakage of urine.
Depression and Anxiety: The emotional toll of living with VVF can lead to mental health issues, especially in communities where the condition is stigmatized.
-
Absorbent Pads: Continual use of pads or adult diapers to manage urine leakage.
-
Pelvic Floor Exercises: Some individuals benefit from strengthening pelvic muscles to regain some control over urination.
Long-Term Outlook
-
Successful Surgery: After surgical intervention, most
individuals can return to normal life, free from leakage.
Rehabilitation and psychosocial
support are key to maintaining long-term well-being.
Successful Surgery: After surgical intervention, most individuals can return to normal life, free from leakage. Rehabilitation and psychosocial support are key to maintaining long-term well-being.
Top 10 Frequently Asked Questions about Vesicovaginal Fistula
1. What is a vesicovaginal fistula?
A vesicovaginal fistula (VVF) is an abnormal connection between the
bladder and the vagina, leading to continuous involuntary leakage of
urine through the vagina. This condition can significantly impact a woman's quality of
life, causing physical discomfort and emotional distress.
2. What causes a vesicovaginal fistula?
VVFs can result from various factors:
-
Surgical complications: Injury during pelvic surgeries such as
hysterectomy or bladder repair.
-
Obstetric trauma: Prolonged or obstructed labor leading to
pressure necrosis of the vaginal and bladder walls.
-
Radiation therapy: Treatment for pelvic cancers can weaken
tissues, leading to fistula formation.
-
Infections: Severe or untreated infections can damage tissue
integrity.
-
Congenital anomalies: Rarely, VVF can be present from birth due
to developmental issues.
3. What are the symptoms of a vesicovaginal fistula?
Common symptoms include:
-
Continuous or intermittent leakage of urine through the vagina.
-
Recurrent urinary tract infections (UTIs).
-
Foul-smelling vaginal discharge.
-
Skin irritation or rashes in the genital area.
-
Discomfort during sexual intercourse.
4. How is a vesicovaginal fistula diagnosed?
Diagnosis typically involves:
-
Medical history and physical examination: Assessing symptoms and
previous medical interventions.
-
Cystoscopy: Using a camera to visualize the bladder and identify
the fistula.
-
Imaging tests: Such as CT scans or X-rays with contrast dye to
locate the fistula.
-
Dye tests: Inserting a dye into the bladder to detect leakage
through the vagina.
5. What are the treatment options for a vesicovaginal fistula?
Treatment depends on the fistula's size, location, and underlying cause:
-
Conservative management: For small, recent fistulas, a catheter
may be placed to divert urine and allow healing.
-
Surgical repair: The primary treatment, involving the closure of
the fistula through vaginal or abdominal surgery.
-
Tissue interposition: Using grafts or flaps to reinforce the
repair site.
-
Radiation therapy: In cases where surgery is not feasible,
radiation may be considered.
6. How successful is surgery for repairing a vesicovaginal fistula?
Surgical success rates vary:
-
High success rates: In non-radiated patients, success rates
range from 70% to 100%.
-
Radiated patients: Success rates are lower, ranging from 40% to
100%, depending on various factors.
Factors influencing success include the fistula's size, location, and the patient's
overall health.
7. What is the recovery process after surgery?
Post-surgical recovery involves:
-
Hospital stay: Typically 1-2 days, depending on the surgical
approach.
-
Catheterization: A catheter is usually placed for 2-3 weeks to
ensure proper healing.
-
Activity restrictions: Avoiding heavy lifting and sexual
intercourse for several weeks.
-
Follow-up care: Regular check-ups to monitor healing and detect
any complications.
8. Are there any risks or complications associated with surgery?
Potential risks include:
-
Infection: At the surgical site or urinary tract.
-
Recurrent fistula: The fistula may reopen after surgery.
-
Urinary retention: Difficulty in urinating post-surgery.
-
Scarring: Leading to narrowing of the vaginal or urethral
passages.
Proper surgical technique and post-operative care are crucial in minimizing these risks.
9. How can vesicovaginal fistulas be prevented?
Preventive measures include:
-
Skilled surgical techniques: Ensuring experienced surgeons
perform pelvic surgeries.
-
Timely medical intervention: Addressing complications during
childbirth promptly.
-
Post-operative care: Monitoring for early signs of complications
after pelvic surgeries.
-
Access to healthcare: Improving maternal healthcare in
underserved regions to prevent obstetric injuries.
10. When should I seek medical attention?
Consult a healthcare provider if you experience:
-
Unexplained urinary leakage through the vagina.
-
Recurrent urinary tract infections.
-
Persistent vaginal discharge with an unusual odor.
-
Pain or discomfort in the pelvic region.
Early diagnosis and treatment are essential for effective management and recovery.
VVFs can result from various factors:
-
Surgical complications: Injury during pelvic surgeries such as hysterectomy or bladder repair.
-
Obstetric trauma: Prolonged or obstructed labor leading to pressure necrosis of the vaginal and bladder walls.
-
Radiation therapy: Treatment for pelvic cancers can weaken tissues, leading to fistula formation.
-
Infections: Severe or untreated infections can damage tissue integrity.
-
Congenital anomalies: Rarely, VVF can be present from birth due to developmental issues.
3. What are the symptoms of a vesicovaginal fistula?
Common symptoms include:
-
Continuous or intermittent leakage of urine through the vagina.
-
Recurrent urinary tract infections (UTIs).
-
Foul-smelling vaginal discharge.
-
Skin irritation or rashes in the genital area.
-
Discomfort during sexual intercourse.
4. How is a vesicovaginal fistula diagnosed?
Diagnosis typically involves:
-
Medical history and physical examination: Assessing symptoms and
previous medical interventions.
-
Cystoscopy: Using a camera to visualize the bladder and identify
the fistula.
-
Imaging tests: Such as CT scans or X-rays with contrast dye to
locate the fistula.
-
Dye tests: Inserting a dye into the bladder to detect leakage
through the vagina.
5. What are the treatment options for a vesicovaginal fistula?
Treatment depends on the fistula's size, location, and underlying cause:
-
Conservative management: For small, recent fistulas, a catheter
may be placed to divert urine and allow healing.
-
Surgical repair: The primary treatment, involving the closure of
the fistula through vaginal or abdominal surgery.
-
Tissue interposition: Using grafts or flaps to reinforce the
repair site.
-
Radiation therapy: In cases where surgery is not feasible,
radiation may be considered.
6. How successful is surgery for repairing a vesicovaginal fistula?
Surgical success rates vary:
-
High success rates: In non-radiated patients, success rates
range from 70% to 100%.
-
Radiated patients: Success rates are lower, ranging from 40% to
100%, depending on various factors.
Factors influencing success include the fistula's size, location, and the patient's
overall health.
7. What is the recovery process after surgery?
Post-surgical recovery involves:
-
Hospital stay: Typically 1-2 days, depending on the surgical
approach.
-
Catheterization: A catheter is usually placed for 2-3 weeks to
ensure proper healing.
-
Activity restrictions: Avoiding heavy lifting and sexual
intercourse for several weeks.
-
Follow-up care: Regular check-ups to monitor healing and detect
any complications.
8. Are there any risks or complications associated with surgery?
Potential risks include:
-
Infection: At the surgical site or urinary tract.
-
Recurrent fistula: The fistula may reopen after surgery.
-
Urinary retention: Difficulty in urinating post-surgery.
-
Scarring: Leading to narrowing of the vaginal or urethral
passages.
Proper surgical technique and post-operative care are crucial in minimizing these risks.
9. How can vesicovaginal fistulas be prevented?
Preventive measures include:
-
Skilled surgical techniques: Ensuring experienced surgeons
perform pelvic surgeries.
-
Timely medical intervention: Addressing complications during
childbirth promptly.
-
Post-operative care: Monitoring for early signs of complications
after pelvic surgeries.
-
Access to healthcare: Improving maternal healthcare in
underserved regions to prevent obstetric injuries.
10. When should I seek medical attention?
Consult a healthcare provider if you experience:
-
Unexplained urinary leakage through the vagina.
-
Recurrent urinary tract infections.
-
Persistent vaginal discharge with an unusual odor.
-
Pain or discomfort in the pelvic region.
Early diagnosis and treatment are essential for effective management and recovery.
Continuous or intermittent leakage of urine through the vagina.
Recurrent urinary tract infections (UTIs).
Foul-smelling vaginal discharge.
Skin irritation or rashes in the genital area.
Discomfort during sexual intercourse.
Diagnosis typically involves:
-
Medical history and physical examination: Assessing symptoms and previous medical interventions.
-
Cystoscopy: Using a camera to visualize the bladder and identify the fistula.
-
Imaging tests: Such as CT scans or X-rays with contrast dye to locate the fistula.
-
Dye tests: Inserting a dye into the bladder to detect leakage through the vagina.
5. What are the treatment options for a vesicovaginal fistula?
Treatment depends on the fistula's size, location, and underlying cause:
-
Conservative management: For small, recent fistulas, a catheter
may be placed to divert urine and allow healing.
-
Surgical repair: The primary treatment, involving the closure of
the fistula through vaginal or abdominal surgery.
-
Tissue interposition: Using grafts or flaps to reinforce the
repair site.
-
Radiation therapy: In cases where surgery is not feasible,
radiation may be considered.
6. How successful is surgery for repairing a vesicovaginal fistula?
Surgical success rates vary:
-
High success rates: In non-radiated patients, success rates
range from 70% to 100%.
-
Radiated patients: Success rates are lower, ranging from 40% to
100%, depending on various factors.
Factors influencing success include the fistula's size, location, and the patient's
overall health.
7. What is the recovery process after surgery?
Post-surgical recovery involves:
-
Hospital stay: Typically 1-2 days, depending on the surgical
approach.
-
Catheterization: A catheter is usually placed for 2-3 weeks to
ensure proper healing.
-
Activity restrictions: Avoiding heavy lifting and sexual
intercourse for several weeks.
-
Follow-up care: Regular check-ups to monitor healing and detect
any complications.
8. Are there any risks or complications associated with surgery?
Potential risks include:
-
Infection: At the surgical site or urinary tract.
-
Recurrent fistula: The fistula may reopen after surgery.
-
Urinary retention: Difficulty in urinating post-surgery.
-
Scarring: Leading to narrowing of the vaginal or urethral
passages.
Proper surgical technique and post-operative care are crucial in minimizing these risks.
9. How can vesicovaginal fistulas be prevented?
Preventive measures include:
-
Skilled surgical techniques: Ensuring experienced surgeons
perform pelvic surgeries.
-
Timely medical intervention: Addressing complications during
childbirth promptly.
-
Post-operative care: Monitoring for early signs of complications
after pelvic surgeries.
-
Access to healthcare: Improving maternal healthcare in
underserved regions to prevent obstetric injuries.
10. When should I seek medical attention?
Consult a healthcare provider if you experience:
-
Unexplained urinary leakage through the vagina.
-
Recurrent urinary tract infections.
-
Persistent vaginal discharge with an unusual odor.
-
Pain or discomfort in the pelvic region.
Early diagnosis and treatment are essential for effective management and recovery.
Conservative management: For small, recent fistulas, a catheter may be placed to divert urine and allow healing.
Surgical repair: The primary treatment, involving the closure of the fistula through vaginal or abdominal surgery.
Tissue interposition: Using grafts or flaps to reinforce the repair site.
Radiation therapy: In cases where surgery is not feasible, radiation may be considered.
Surgical success rates vary:
-
High success rates: In non-radiated patients, success rates range from 70% to 100%.
-
Radiated patients: Success rates are lower, ranging from 40% to 100%, depending on various factors.
Factors influencing success include the fistula's size, location, and the patient's overall health.
7. What is the recovery process after surgery?
Post-surgical recovery involves:
-
Hospital stay: Typically 1-2 days, depending on the surgical
approach.
-
Catheterization: A catheter is usually placed for 2-3 weeks to
ensure proper healing.
-
Activity restrictions: Avoiding heavy lifting and sexual
intercourse for several weeks.
-
Follow-up care: Regular check-ups to monitor healing and detect
any complications.
8. Are there any risks or complications associated with surgery?
Potential risks include:
-
Infection: At the surgical site or urinary tract.
-
Recurrent fistula: The fistula may reopen after surgery.
-
Urinary retention: Difficulty in urinating post-surgery.
-
Scarring: Leading to narrowing of the vaginal or urethral
passages.
Proper surgical technique and post-operative care are crucial in minimizing these risks.
9. How can vesicovaginal fistulas be prevented?
Preventive measures include:
-
Skilled surgical techniques: Ensuring experienced surgeons
perform pelvic surgeries.
-
Timely medical intervention: Addressing complications during
childbirth promptly.
-
Post-operative care: Monitoring for early signs of complications
after pelvic surgeries.
-
Access to healthcare: Improving maternal healthcare in
underserved regions to prevent obstetric injuries.
10. When should I seek medical attention?
Consult a healthcare provider if you experience:
-
Unexplained urinary leakage through the vagina.
-
Recurrent urinary tract infections.
-
Persistent vaginal discharge with an unusual odor.
-
Pain or discomfort in the pelvic region.
Early diagnosis and treatment are essential for effective management and recovery.
Hospital stay: Typically 1-2 days, depending on the surgical approach.
Catheterization: A catheter is usually placed for 2-3 weeks to ensure proper healing.
Activity restrictions: Avoiding heavy lifting and sexual intercourse for several weeks.
Follow-up care: Regular check-ups to monitor healing and detect any complications.
Potential risks include:
-
Infection: At the surgical site or urinary tract.
-
Recurrent fistula: The fistula may reopen after surgery.
-
Urinary retention: Difficulty in urinating post-surgery.
-
Scarring: Leading to narrowing of the vaginal or urethral passages.
Proper surgical technique and post-operative care are crucial in minimizing these risks.
9. How can vesicovaginal fistulas be prevented?
Preventive measures include:
-
Skilled surgical techniques: Ensuring experienced surgeons
perform pelvic surgeries.
-
Timely medical intervention: Addressing complications during
childbirth promptly.
-
Post-operative care: Monitoring for early signs of complications
after pelvic surgeries.
-
Access to healthcare: Improving maternal healthcare in
underserved regions to prevent obstetric injuries.
10. When should I seek medical attention?
Consult a healthcare provider if you experience:
-
Unexplained urinary leakage through the vagina.
-
Recurrent urinary tract infections.
-
Persistent vaginal discharge with an unusual odor.
-
Pain or discomfort in the pelvic region.
Early diagnosis and treatment are essential for effective management and recovery.
Skilled surgical techniques: Ensuring experienced surgeons perform pelvic surgeries.
Timely medical intervention: Addressing complications during childbirth promptly.
Post-operative care: Monitoring for early signs of complications after pelvic surgeries.
Access to healthcare: Improving maternal healthcare in underserved regions to prevent obstetric injuries.
Consult a healthcare provider if you experience:
-
Unexplained urinary leakage through the vagina.
-
Recurrent urinary tract infections.
-
Persistent vaginal discharge with an unusual odor.
-
Pain or discomfort in the pelvic region.
Early diagnosis and treatment are essential for effective management and recovery.


